In today’s episode of the Flex Diet Podcast, Dr. Chris Morrissey and I discuss a wide range of health topics, including three common health procedures that can help you live a healthier, longer life.
Episode Notes
- Dr Chris’ background
- The top health preventive items
- Why most docs don’t talk about longevity markers, such as muscle mass, aerobic exercise and grip strength
- How med school is really set up (newsflash – minimal work on nutrition)
- How docs can get more training on exercise and nutrition
- CPAP, sleep, teeth, and cranial structure
- Who should you seek out for true preventive health?
- Best decisions, but on limited data- all the time
- Variation between you vs the next person (similar but different)
- Visceral hands-on work
- Colonoscopy
- how often is it recommended?
- risks?
- when to get tested (could be as early as 30 years old)
- what the prep is like now (PEG vs mag citrate)
- Gallbladder
- what it is
- potential causes
- pain is not local
- what is commonly done
- gallstones
- gallbladder removal
- other medical procedures
- should you avoid higher fat diets?
- Gastric Ulcers
- what are they
- who is at risk?
- H pylori (see below)
- drop in blood flow with longer endurance exercise
- what is a PPI (proton pump inhibitor)
- long term ideas for PPIs
- Lifestyle vs drugs/pharmacology
- When should you get bloodwork? How often?
- What is the PRAL score?
- The minimal dose of exercise/movement
- Find Dr Chris Morrissey:
- Podcast: “The Morrissey Movement“
- Email: themorrisseymovement@gmail.com
- H pylori follow up (Source)
- “They discovered that peptic ulcers were due to Helicobacter pylori, not stress as previously thought. In 1984 Marshall did the ultimate test by infecting himself with the bacteria, developing the symptoms of the disease and then successfully treating himself with antibiotics.”
This podcast is brought to you by the Physiologic Flexibility Certification course. In the course, I talk about the body’s homeostatic regulators and how you can train them. The benefit is enhanced recovery and greater robustness. We cover breathing techniques, CWI, sauna, HIIT, diet, and more. The course will open the first week of April 2022.

Dr. Mike T Nelson
Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
Dr. Mike T Nelson
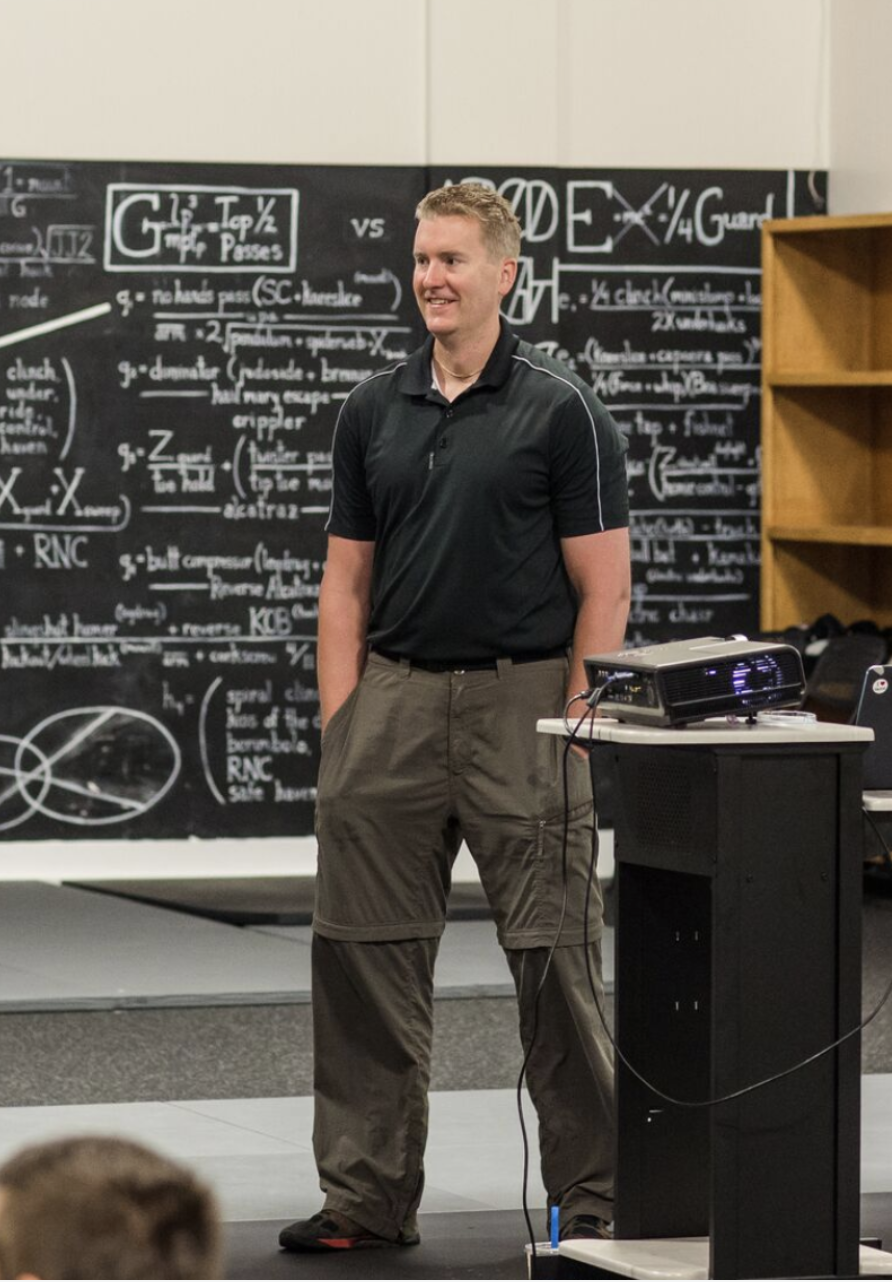
Welcome back to the flex diet podcast. I’m your host, Dr. Mike T. Nelson. This is a little bit of the intro before the intro. And today I’ve got on the podcast Dr. Chris Morrissey. And we’re talking about three kind of health procedure, things that I think as a human being walking around, and especially as a trainer or a coach, you should know more about, and Dr. Chris is the person who has done some of these procedures, he’s also working in fitness. So he is the perfect guy, in my opinion to blend these two areas.
One of them is going to be talking about the exciting topic of colonoscopies. And before you completely tune out of this episode right now, something he brings up that I was completely unaware of, is, you may even need a colonoscopy as young as 30 or 35. If you have certain conditions. So listen to this podcast, I think you’ll find it useful. And again, could definitely extend your health, which is going to allow you to train more and just generally live a better life. If you’re looking for things past exercise, and nutrition and recovery to what is the next level of things you can do to extend your longevity based on science and be more robust, increase your recoverability. If recoverability is a word, check out the physiologic flexibility, certification, go to physiologic flexibility calm.
If you’re listening to this now in March, it will open again for one week starting around April 4 2022. So that will be your next opportunity to get in on to the next enrollment. And if you’re listening outside of that time, you can still go to physiologic flexibility calm, get on the waitlist, we’ll have lots of information there in the meantime, and you’ll be the first to be notified once it opens again. In it we focus on everything from Cold Therapy hot such as sauna, how to alter pH, which looks like some low intensity interval work or some very high intensity intervals. There’s a specific way to do that. Breathing techniques, even things like fuel systems, ketones to glucose, and especially oxygen and co2. Should you be doing specific breathing techniques both at rest into the meditation session or during exercise, so nasal versus mouth breathing, etc. So go to physiologicflexibility.com for all the information and enjoy this episode with Dr. Chris Morrissey.
Dr. Mike T Nelson
Hey, welcome back to the flex diet podcast. I’m your host, Dr. Mike T. Nelson. I’m here today with our special guest, Dr. Chris Morrissey. Say hello. How you doing? Good. I like your shirt for people who might not be watching us on video.
Dr. Chris Morrissey
It says drink coffee run hard eat tacos.
Dr. Mike T Nelson
That sounds like metabolic flexibility to me.
Dr. Chris Morrissey
That it is I got it from. So I do the garage gym athlete training. And one of the guys does the merch for it. And his name’s Krampus. And he has his own little company. It’s called. I forget what it’s called. But anyway, and he’s got a bunch of different T shirts that we can buy through the website. So I bought some of those from him. So this Oh, the ones Yeah, so it’s pretty cool. That’s awesome. Yeah, yeah, I like it.
Dr. Mike T Nelson
And today, we’re talking about kind of three medical thingies for lack of technical term people should know about. And obviously this is not to be prescriptive in any way. There’s no doctor patient relationship. This is just you’re going to provide us with some cool research and things that people are listening should take to the doctor, just kind of an outline of even preventative schedules, like one of the items will be colonoscopy, which I’ve been avoiding, which I need to do.
So maybe we can give people a kick in the bud of why they should do these things. Or if they have clients, I think it’s also good. Because fitness professionals interact probably more with their clients than their physician does, for better or worse, you know, to be like, Hey, Bob, you’re 65 You’ve never had a colonoscopy, you should talk to your doctor and go get one and, you know, hopefully just kind of prod them nicely, a little bit more in that direction. Sure. Because even the amount of I always blame it on guys, because it’s typically more guys and women but the amount of guys who I work with who I’m like, Hey, man, when’s the last time you had blood work? They’re like, five years ago. I’m like, right? You should probably get that done. Yeah, for sure. Yeah. So give us a little bit of your your background.
Dr. Chris Morrissey
So like you said, my name’s Chris Morrissey. I’m actually a general surgeon, by training. I’ve lived down in Winfield, Kansas. I’ve been here Since July of 2012, so almost 10 years now, I went to medical school in Kansas City at the it’s changed names like three times, but it’s the osteopathic medical school there is now it’s called kcu, Kansas City University. So I was there for actually five years. So the first two years of medical school is all in the classroom. And then the next few years are out on rotations doing different you know, rotating through different specialties, internal medicine, family medicine, surgery and all that. And I took a year off and did an undergraduate osteopathic medical or osteopathic manipulation fellowship. So in do school, we all learned manipulation. So kind of the chiropractic stuff that makes DEOs separate from MD.
I took an extra year, just getting extra training in that because I really liked it, and it helped a lot of people. So So I did medical school for five years. And then we moved up to Grand Blanc, Michigan, from Kansas and I was there for five years doing my general surgical training. So we were about 10 minutes south of Flint and about an hour west of Detroit. So I’m close. Yeah, I was the armpit in the butthole of Michigan. Terrible towns, but anyway, I trained there for five years, and I got this job right out of residency and then came down here, towns about 10,000 people. So there’s me and one other general surgeon here and I’m hospital employed. So I get paid the same whether I work or whether I don’t. But I open our wound center. So I’ve been the one Center Medical Director since 2014.
I also moonlight in emergency room most Monday nights. So I work a 12 hour shift in there just a doc in the box type of thing. I’m also the trauma Medical Director. We’re a small like level four Trauma Center, which basically means that we stabilize and send people out if need be. And then I also am the medical director of our medicals Med Spa here in town. So I do cosmetic and therapeutic Botox and filler and PRP injections and sclera therapy. So I do a little bit of everything. But you know, as far as general surgery goes bread and butter stuff, I do gallbladder appendix bowel resections a lot of colonoscopies a lot of upper scopes, you know, hernia repairs, just kind of whatever comes in we you know, as long as we feel we can deal with it. And if it’s not, we send it to a tertiary care facility, which is like, we have two level one trauma centers about an hour up the road in Wichita. So, so that’s kind of what we do.
Dr. Mike T Nelson
So you don’t really do anything. Just sit around on your hands.
Dr. Chris Morrissey
So yeah, yeah, but then last couple years, I’ve gotten into I’m also currently doing a functional medicine fellowship, through the Institute of functional medicine online. So I just kind of fell into this type of thing. And the main reason I was really attracted to it is because I’ll have usually younger women that come in with nausea, vomiting, bloating, abdominal pain, and I’ll work up their gallbladder, if it sounds like the gallbladder, I’ll take it out. If it’s not, you know, I’ll scope them. And then if it’s nothing, then I send them on their way to somebody else. But then it’s just like, I’m getting so many of these people and I was like,
There’s got to be something I’m missing something else that I can do. And so I’ve been learning way more about, you know, the gut microbiome. And so I’ve been doing some modules, I hopefully be done my fellowship next year. So I can kind of institute that and I’ve kind of I kind of dabble in it. Now. I mean, there’s a lot of that I don’t know yet. But you know, basically the there are pillars, which is something you kind of somewhat preach in your classes too, about, you know, sleep nutrition exercise, which is something that physicians learn zero about in medical school, at least the allopathic and osteopathic physicians, you know, the naturopaths and, you know, the Indies or the chiropractors, they learn more about that than we do, but I’m just learning how it’s, everything is so intertwined, and that you can fix a lot of diseases just with good food and exercise, you know, and I’ve been doing that, and then I got personal training certification during COVID because I was bored.
So I’ve got that and trying to get up and go into and, um, you know, that’s, that’s kind of about it. So I just kind of really taken a turn to get into medical fitness. And I’m just trying to get in any avenue that I can to, you know, maybe augment a side hustle and or help my regular patients if they’re interested. So,
Dr. Mike T Nelson
wow, that’s awesome. I had this question on Instagram the other day, too. I posted some stuff about longevity. Yeah, and one of the guys commented, which is a good comment. He’s like, Well, why did most physicians never talk about this? And it was, you know, stuff like a robic base, you know, body you know, muscle mass, especially lower body strength and then grip strength. And like on that wasn’t I’d love to get your comments is that when I was doing my PhD at the University of Minnesota, like a lot of the anatomy physiology classes we took were through the med school, so my minor was in anatomy and physiology, so we got to use their gross anatomy labs and stuff. So a lot of times were hanging out with, you know, the, I don’t know, it was a third year med students or second year or whatever.
And it was interesting just talking to them about like, what they take, and you know, you could take your advanced, you know, ANP Anatomy, physiology and etc. But a lot of it was like hardcore, like pharmacology. Oh, like after that there, I was like really shocked because I always asked physicians, I’m like, well, like, how much training did you ever get just nutrition and exercise, not enough on your own. There’s a lot of, you know, Doc’s like yourself who do a lot of that on their own are very well educated in it. And it’s usually like, an hour and a half, two hours. And I’m like, what, like, out of the entire med school, you get, like, a couple hours.
They’re like, yeah, that’s just you know, what diet not to put the diabetic and we put them in the hospital and, you know, basic stuff. So we just don’t kill someone and tell them to do the wrong thing. Which, I don’t know, I just love your comments on that. Because it, it seems so backwards. And I know, like physicians are in a hard spot, cuz they get like 15 minutes per patient, and like, you know, bigger cities and stuff. So it’s, they don’t really have a lot of time to talk to him about a Bob, you should think about exercise, but it just seems like it’s very backwards.
Dr. Chris Morrissey
Yeah, no, I’ll echo exactly, that’s pretty much spot on what we learned to you know, I don’t remember exactly, you know, the the hours, but if you could count on one hand of that, I mean, it’s just, we get so much crammed down our throats on, you know, throughout the Krebs cycle, draw, you know, all the, you know, interleukin pathways and acid cycles, all these like biochemical things that we have to learn plus all the pharmacology and so like, the way my school was set up was we had a systems based approach. So we did the first six weeks was kind of just like a hodgepodge of things. It didn’t really fit in anywhere, just kind of intro stuff.
And then our second module was musculoskeletal. So we learned everything. So we learned all the anatomy, physiology of all the muscles in the body. And then pharmacology, biochemistry, so everything about that, and we took a series of tests like anatomy, practical, pathology, practical, and then just different medications and stuff, you know, pharmacology and histology, and then we would take tests, and then we move on. The next one we did was like, skin, blood and lymph. So we had two weeks for like leukemia, lymphoma, all that and then like two weeks, a DERM. And then two weeks of like blood dyscrasias, and all these different disorders, which was a lot of information. And then we went on to cardiac and then respiratory, and then Gi. So that was our first year.
Our second year was neurology, like all the neuroanatomy which was like a 10 week course, which was a ton. And then we got into more like renal, and then like integrin, OBGYN type stuff. So but as far as all that goes, Yeah, I would say we maybe had one basics on nutrition, and it wasn’t even anything about, you know, okay, how many kilocalories are in a, you know, fat, carbs? Protein, and that was pretty much it? Well, there’s nothing about different diets, exercise was just like, Yeah, you should, you know, get out walk or run maybe 100 150 minutes a week, but nothing on any type of training, nothing about, we did some functional assessments, but it was more osteopathic like, you know, finding tissue texture changes, and then doing the manipulation, you know, the cracking backs and necks and different modalities to alleviate pain, which, so that was probably the most functional like assessments that we got.
And we did like range of motion stuff, and joint testing of all the ligaments and tendons and stuff like that. But we got 00 education on sleep. You know, I learned so much from just reading Matt Walker’s book, why we sleep. Tons of stuff that I didn’t even know about that I learned. I read that, like two years ago. So yeah, we just get very little training, which is sad. You know, if you look at it from the Functional Medicine Hat, you know, like, we’re really good at acute disease, you know, strokes, heart attacks, surgery, whatever. But as far as preventative health we kind of suck at it unless we take special interest in it just because we’re not trained in it, which is whether it’s right or wrong.
I don’t know I feel it is kind of wrong, because most people will go to their family doc and be like, Well, hey, you know, what can I do? You know, my shoulder hurts I’m trying to do these CrossFit workouts What can I do is like well quit working out for six weeks, you know, the standard answer Prophetstown all they don’t go let’s go to physical therapy or Hey, instead of doing snatches, let’s work on you know, whatever. So give you a different course is that just avoid what you’re doing and or just like yeah, don’t deal with that, you know, go talk to somebody else so and not all doctors are like that. I’m not trying to bash Yeah, by any means. But in the standard training, that’s what we get, which really kind of sucks.
Dr. Mike T Nelson
Someone is like most of this audience will be interested in preventative health and obviously they’re doing a lot of stuff on their own. But is there sort of one person or sort of one training you would recommend people go to if they want to do more for lack of a better umbrella term preventive health because I agree, it seems in the US most Doc’s are just not trained in it. And you know, if I’m in a massive car accident, yes, take me to the best, you know, er Center, you can find if I get hit on the head, then yeah, do whatever you need to do. And most of the time, the places are gonna be pretty good at that. But it’s like, yeah, I got some blood work. That’s kind of weird. They’re like You know, the last in person physical I had was a doctor who looked like he could he, he was like 10 years past retirement.
Like he barely kind of made it into the room. And I’m asking him like, Hey, man, can I just do like a basic blood work? This is back when I worked for a medical device company. So it’s a long time ago. And so I had insurance. And he’s like, it’s one in the afternoon. You’re not fasted. I said, No, I didn’t eat anything this morning. Because I knew I was coming in here. I wanted to have blood work done. He’s like, Are you sure you didn’t eat? I’m like, Yes, I’m sure I didn’t eat this morning. And it took me, you know, several minutes arguing with them.
And finally, he’s like, okay, and I’m like, Well, can you look at a vitamin D level to like, 25? hydroxy? Is it guy, you’re fine. I’m like, I don’t travel. I live in Minnesota. It’s February. I think I might be low. And I know that if you suspect that it’s low, how my insurance doesn’t pay for it. He’s like, I don’t know. Like, pokes on me a little bit. Yeah. What are you? Yeah, you’re not quite 40 yet. Wear your seatbelt. You’re fine. Like, that’s my physical. Yeah. And that’s, you know, that’s horrible. Most places are not quite that bad. Right. But if someone wants to go in for more preventative health, is there any place you would recommend or things they can do? I know, it’s a super loaded question.
Dr. Chris Morrissey
Oh, kind of I mean, like, you just kind of have to seek out you know, always start with your family doc, you know, yeah. And then maybe word of mouth. Like if you go to a gym, you noticed, like, Hey, you guys go see for whatever kind of a specialties, integrative medicine, which is sort of in the functional medicine side, it’s kind of more of a global health. You know, in theory, family practice is supposed to be kind of like that. But again, it’s more of not quite as arbitrary as what you had done to you for that person.
But usually, it’s just, you know, history and physical. And they’ll you know, check basic blood work, but they usually don’t get out there and check other like vitamin levels and stuff like that. There’s more things popping up now, like different companies that have like apps, there’s one that I do think it’s called insidetracker, which I don’t know why we’re just on my own, and they the only pain in the ass is just going to get your bloodwork done, let’s say yes. But otherwise, it’s kind of cool. And they give you good, it seems to be good quality, like levels and tests or whatever. But I mean, it’s kind of word of mouth or finding some sort of, you know, functional medicine practitioner, if you can find one of those. Those are kind of more of the type that you’re inquiring about. Or the medical fitness network, you know, which I recently joined, which I didn’t even know was a thing.
Dr. Mike T Nelson
There that that was the thing, either. I’ve just heard rumblings about it.
Dr. Chris Morrissey
Yeah, I actually heard about it in the the ISSN podcast, and I reached out to this lady, and I’m actually starting to kind of do stuff with them. I haven’t really gone out yet. But I was really excited hearing about that, because they have CMEs. And they have all kinds of things. But you can look up practitioners in your area that do medical fitness, because actually I was interviewed on the garage, gym athlete podcast once and they had asked you know about, well, who can we go to? How can we find a doctor that’s interested in things like you are? And I was like, I don’t know if there is, you know, just word of mouth, I have no idea.
But then I found out the medical fitness network. And I was like, this is probably a place to start. But yeah, I would always start locally with your family doc, and then try to find, you know, you can go on that route. And as long as I’m not recommending you go off on your own and Rogue do vitamin testing and do on your own. No, that’s not good doctor really advice but if you’re fairly healthy, and you’ve been examined by a physician and you’re healthy, you just want to know more about your, you know, deeper dive into nutrition and stuff like that, I would probably seek out either Functional Medicine Practitioner or integrative medicine or, you know, naturopathic physicians, you know, they’re in these not in these, but they get like 400 hours in nutrition and things like that.
They’re considered like holistic medicine, which is sort of an umbrella term for vagueness. That’s not I don’t know, you know, the, the regular, like allopathic physicians and osteopathic physicians that kind of look at it is out there kind of thing, just because under the term holistic, but there’s a lot of good practitioners that do that stuff. So that’s probably what I would do. I’ve never personally sought sought out somebody like that. I just kind of do stuff on my own. Because I don’t know my doctor, I can do what I want. But yeah, so I don’t know, that’s kind of a roundabout answer, but that’s what I would say.
Dr. Mike T Nelson
Yeah, no, that’s, that’s super helpful, because that’s a question I get a lot and I kind of go to answers, initially just a little bit similar to you. And like, just, you know, even with my own clients, it’s like, okay, go to your doc, here’s the test, you know, that you should recommend, if your doctor needs a shit ton of research on it, I can send you with a whole bunch of PDFs to give him or her to, to read most of the time, they’ll just look at and go, Okay, whatever, and then run it. Sometimes I’ll even look at what their blood work is.
I have another guy who has a MD PhD that looks over stuff to, again, not trying to diagnose or prescribe anything, but to me, it’s just an extra level of data and a snapshot to look and see what’s going on. And then at least you can go back to their doctor Be like, Hey, next time you go in, like ask him, we have one person, like their red blood cell count was just super high, you know, and I started so my MD buddy who I have on retainer, and I’m like, I just sent him I didn’t tell him anything about it. I’m like, What do you think’s up with this? He’s like, is she a cyclist on EPO? I’m like, No, when it turns out long story short, she had massive sleep apnea.
So she’s getting so hypoxic at night, interesting. That’s her red blood cell mass is going up, because her body’s like, oh, shit, we don’t have enough oxygen to get around. Cheryl, let’s try to fix this by, you know, bumping up red blood cell mass to try to compensate and get oxygen to the tissue. Which is wild. I told him like, go back to your doc and ask, you know her about why this is high. And it just didn’t do anything. So we ended up sending her for a sleep console do like, oh, yeah, massive sleep apnea. And then the ironic part of the whole story is that she ended up not needing my services anymore, because she had to pay several $1,000 to have her basically her jaw realigned in her teeth, because her tongue just falling in the back of her mouth. And her whole kind of facial structure was kind of a disaster causing her sleep apnea, but which is fine.
She’s a lot better now. That’s crazy to me. And when I think back on it, I’m like, I wonder what would have happened, like, if she wouldn’t have just got a basic blood panel, just to look at it, you know, because, you know, as you know, right, sleep apnea, if it’s really bad, and hers was really bad, causes all sorts of other issues, you know, just on your body in general to
Dr. Chris Morrissey
Oh, yeah, for sure. I’ve never heard of us. Like, I don’t deal with sleep apnea much. But as far as having to get your facial reconstruction, just based on I’d never heard of that before, that must been super bad if they had to do that. Because usually you put them on a CPAP. And, you know, recommend diet and exercise. And usually you can do a lot of things with that.
Dr. Mike T Nelson
I did a whole podcast with couples on this too. And I think CPAP ‘s are awesome, and they definitely work. So I’m in the process to my wife has gone through this is going through now of looking at facial and jaw structure, if there’s anything you can change with that even as an adult. So the short version is, I had just the disasterous teeth when I was a kid, I had teeth that were crooked, like completely sideways behind each other. So the standard thing was, which I’m grateful I had you know, orthodontics, which was good. For four and a half years, I had headgear, I had springs, I had rubber bands.
But in essence, all they were doing was like rearranging the teeth on a structure that was already too small. So it’s not as some of the new which is actually an older approach is to, can we open up the job, maybe the palate a little bit or change some of the underlying structure, so that your teeth actually will move to a place that’s better. So we’re creating more space, not just trying to rearrange your teeth on the same structure. So the catch with some of all that is that it can interfere with your airway. And so if your airway is super narrow, then you’re going to have stress symptoms all the time. Sure. So another buddy of mine has been doing this. He’s in Chicago.
He treats kids who have ADHD, and he’s basically an oral dentist. I’m like, what do you do? The first time I talked him like six years ago, I’m like, What the hell are you doing? This makes no sense to me. And he’s like, Well, it’s this simple. He’s like, the kids, I see their structure is so bad that their airway is being impacted me image, their airway, it’s super small. And so their brain thinks they’re not getting enough oxygen. So all the symptoms they present are basically ADHD. So they clinically have ADHD, because they’re just like stressed out little sympathetic squirrels running around all day. And he’s like, once we change that structure, especially in kids are much more plastic. We get their airway open. And he’s like, so far, like almost all of them their symptoms of ADHD go away. It was just their brain was not getting enough oxygen.
Dr. Chris Morrissey
Wow, that’s awesome.
Dr. Mike T Nelson
Yeah. So off halfway down. That is one of those things where it’s like, the amount of learning just related to physiology in general is just never ending. You know, it’s just the Yeah, so I always think that’s a good good info where people can go to get more information, which is great. Absolutely. So if you’re listening, get your blood work. The other positive, I think is, it’s becoming easier to do it online.
I mean, I confess I’ve done all my blood work only online in the last few years. And because of COVID, for better or worse, I think that’ll become a much more real thing. Or telemedicine, you may not be limited to just someone in your area. Obviously start with the normal doc you see, but there may be more options and they’re dramatically coming down in cost now to does if people are listening in there business owners, your my insurance doesn’t cover anything as a major medical, so everything is out of pocket on top of it.
So having cash options that come down if you don’t have insurance or only have major medical, and you don’t have to go into someone, I think we’ll have more options in the future, which will make hopefully some of these things easier. Absolutely. So you had three items you wanted to talk about today? What’s item number one?
Dr. Chris Morrissey
Yeah, well, we kind of already brought up colonoscopy. So yeah, I guess we can start with that. Um, you know, we can kind of spin this however you want, I can just talk about the procedure and kind of what we look for. And a couple of things, if that’s what you’d like.
Dr. Mike T Nelson
Yeah, just give us some rundown. So for people who are listening to, they may not know much about it, other than I probably should have one.
Dr. Chris Morrissey
That’s, that’s number one, for sure. I just kind of go through my normal spiel that I give in the office and perfect kind of go from there. So as far as going on speech, go, you know, the the previous recommended age to get them was age 50. If you have no family history, and you’re having no problems. Now, they’ve actually lowered that to 45. And I’m not 100% sure if all insurances are on board with that yet.
I know some of them are. So I’m starting to see a few younger people that are around that age group to come in and get one done. But if you have a family history, though, you should get 110 years prior to the youngest relative that was diagnosed with colon cancer. So if your father was diagnosed at the age of 40, you need to start getting him at the age of 30.
And or if you’re having any problems, big red flags, you would see his blood, your stool, obviously, you know, bright red blood dominant pain changes in your bowel habits. Just something that’s not right, your stool is changing in caliber, you know, if they go from normal size to you know, like pencils, or, you know, pellets or something like that. So there’s actually a whole cascade of like, diagnosis of stool. It’s really weird. Pictures, and you can show people what is your stool scale?
Dr. Mike T Nelson
Yeah, exactly. So yeah. Girl in the office. The Bristol, people love talking about that stuff.
Dr. Chris Morrissey
I know. It’s crazy. It’s so funny. But anyway, so. So yeah, so someone comes to see me most often it’s for screening, they’re not having any problems. So when you from an insurance standpoint, if you’re having no symptoms, and you have no family history, typically they won’t pay for one before the age of 45 or 50. Now, but if you’re, you know, any type of changes, I’m usually very conservative surgeon but with scoping, I stopped people more often than not, I’ve had a few people that I found colorectal cancer younger than 30.
Oh, I had one guy that was a couple years ago that his only symptom was it was just harder to push stool out. He had never had bleeding, no weight loss, night sweats, none of that no family history. And I was like, Okay, well, it’s probably just diet or whatever. So I went in and scoped in and about, oh, the very top of the rectal VA, which is about 18 to 20 centimeters inside the colon, he had a circumferential mass, almost near obstructing. And so I sent him to a colorectal specialist. And he ended up having metastatic disease. He had big, you know, big balls of cancer in his liver.
Dr. Mike T Nelson
But he had no warning signs.
Dr. Chris Morrissey
I mean, he said, Hold on for about six months. And, you know, there’s unless it was a really, really aggressive cancer that it’s been going on for a while, he just had no idea what was happening. So that’s super unfortunate. So whenever I hear think about those things, I’m always like, I’m going to scope sooner rather than later. But, but it’s one of the best diagnostic and therapeutic tests that we have. So meaning you can go and you can find things but you can also li treat at the same time. It’s you know, I kind of tell people, it’s about three hours out of your day you show up an hour before the procedure.
The procedure is blocked off for about an hour but in usually takes 15 to 20 minutes depending on how much work you have to do when you’re in there as far as taking out polyps and whatever and then they go to recover for about an hour then they go home. That our hospital we use propofol which is the Michael Jackson’s use, you know, you just get some white stuff through the IV and fall completely asleep and have no idea what’s going on and it’s you wake up and you feel rested and go home.
Dr. Mike T Nelson
propofol is pretty fast acting if I remember correct. Okay, use that for cardio versions. I think two people have a fib.
Dr. Chris Morrissey
Yeah, they can it’s just to sedate him before they do dilation or whatever. Alright, it seems to be Yeah, we use propofol for a lot of things. You know, it’s it’s a great drug it and it’s metabolized by the liver very quickly. So it goes like this much respiratory issue with the D there is there. There’s some because they give a high doses it can be but yeah, and some people that are big drinkers, they tend to require a lot more profiles. So it takes way more to get just to get him sleepy enough so we can do something so but but yeah, it’s you know, painless, the worst parts of the prep. So the day before you around noon, or about two in the afternoon, actually we use a whole having take a whole bottle of MiraLAX which is a tasteless white powder that you mix and it’s have a ton of diarrhea.
You know, I always tell them if you come in full of it, so to speak, I can’t do my job very well because you can miss so many things. So just just magnesium citrate is what they used to kind of fill out or is it different? No, it’s polyethylene glycol. So that’s Oh, it’s big. Yeah. Yeah, it used to be, it used to be the Golightly, which you’d have to drink about a gallon of, of liquid mixture, then people have a lot of throwing up and just so much volume. But now you relax.
You only have to use about half the volume and it works really well. So different places use different things. And some big endoscopy centers, they’ve gone to what they call a split prep, where they’ll do half the day before and then half the morning of if you’re having it later in the day, and we just only do it in the morning. So we don’t do that. And I usually I would say, about every 100 colonoscopies, I might get one that the prep is just not very good. So most people do really well with it.
Dr. Mike T Nelson
Yeah. And I think that’s a problem that people are scared about. Because those are all like the horse. Like the friends I know. I’ve had it like, the horror stories I’ve heard where them like, I had this, like two gallons of this crap, I had to drink. And I felt horrible for this long. And I’m like, Yeah, you kind of suck it up. But I think knowing that the prep isn’t as bad as what it used to be is probably a good thing. And hopefully will be less of a deterrent for people, especially, you know, all these stories gets like cycled from like 10 years ago to one person had a bad experience. And that’s all you hear about.
Dr. Chris Morrissey
Yeah, it’s either the prep, or they have a friend that had a friend that had a friend that had a perforation from a colonoscopy and had to have surgery. And so it’s always a risk. And we always talk about it. It’s super duper rare, but it can happen but it’s very safe procedure. So you know, we drift off to sleep, we scoped the entire colon, always do a rectal exam, like for men, we check prostate you know, looking for lesions or, or enlarged prostate and then just scope the entire colon.
So when we get over to the right side, you can either see the opening of the appendix, called the appendiceal. orifice, or you see the terminal ileum. And then from there, you just back out and you’re looking for polyps, or diverticulosis, or you know, colon cancers, different entities depending on why we’re doing it. And then the nice thing is that there’s polyps that are, I don’t know, anywhere between a pinhead and even up to maybe even a golf ball, we can take them out into scopic Lee, there’s a couple different devices we use. If they’re smaller, there’s these little like pincher, graspers, almost like a little pair of tweezers type of looking band along on a long wire that we can do, or there’s like a little it’s called a snare, but I just call it a wire lasso, basically wrap it around the base of it and lop it off and suck it out to the scope. Yeah, exactly. So that’s cool. We can also tattoo the lesions when we’re in there.
So if it’s like, it’s a big mass, or either if you’re removing the entire thing, or you’re gonna mark it later on for surgery, you just tattoo some India ink, you just inject it into the mucosa of the colon, and then it’ll soak up through the mucosa out into the serosa into the abdomen. And so from a surgical standpoint, if you go in robotically or laparoscopically, it’s kind of an X marks the spot you know exactly where the lesion is, because sometimes you can’t feel it, you know? So it’ll show up on the skin, then is that correct? Not on it on the on the colon itself, but it won’t go clear through like on your abdominal wall, on the outside of your organs.
And sometimes you find this little spray of ink kind of in the area, because it all matters how to set the surgery up. Because if you’re doing right colon, you set your port sites where you’re going in one side. And if you’re doing a left colon, you just kind of got to know where it is. So yeah, if you’re getting someone to operate on that you didn’t do the scope on you don’t really know where it is you’re taking the GI guys word for it, or whoever.
Dr. Mike T Nelson
And so you got to kind of right there wasn’t there at all, right.
Dr. Chris Morrissey
And the other thing too is, you know, the scope is numbered, there’s numbers on it every 10 centimeters. And so you can say, Oh, is it you know, 30 centimeters, which should be in the sigmoid. But sometimes if you get a loop in the scope, it’s basically you know, like pushing a rope. And so you might actually be way farther, and you’re way farther out than you think. And so that really makes a difference. So but anyway, once you’re done, you go home, and then I’ll go over the pathology results in the office and you know, there’s a couple different types of polyps if you want me to go over those.
The most common usually is what’s called hyperplastic. So those are basically like a mole. They never turn a cancer, they can get bigger, they can bleed, but they never turn a cancer. Then there’s the the adenoma family. There’s tubular adenomas, which is the most common of the adenoma as it’s got like a five to 10% chance to turn the cancer depending on what you read. And then there’s the tubular Billis adenoma, which is about a 30% chance to turn the cancer and then a villus adenoma which is about 50%.
So the more you go up on that scale, the higher the risk of turning to cancer and then they look at it to see if they’ve had any cellular dysplasia and I’ll mark that on the on the pathology so then you know is okay that is rapidly dividing. We should maybe you know do a short follow up in like six months to make sure that it’s gone or talk about an elective resection if it’s got some actual cancer cells in it. So, but it’s a great test, you know, nobody wants to do it. No one’s super excited to see me in the office for
Dr. Mike T Nelson
imagine Yeah, hey, it’s my call it asked me today.
Dr. Chris Morrissey
Yeah, yeah, no one ever is excited for sure. But um, but yeah, so you can see a lot of things on the scope isn’t We’ll do this for abdominal pain or diarrhea, you can go in and take some random biopsies. You know, there’s Ulcerative Colitis and Crohn’s disease that people talk about. You can get those diagnoses. Sometimes I’ve colonoscopy, ulcerative colitis is only in the colon, and it starts like in the rectal area and spreads proximately. So you’ll always find it there.
And the difference, the main difference between those two, and you could talk an hour on each of them. But basically, Crohn’s can be anywhere between your mouth and your anus, basically, because it can skip around. And sometimes it’s hard to diagnose or as ulcerative colitis, it’s in the colon, it only stays in the colon. So you can you can usually figure that out by biopsies. So, that’s another reason you might get a colonoscopy. But, um, as far as, you know, colon cancer itself, it’s like the third leading cause of death in United States. So it’s raw, it’s up high. Yeah, it is.
And, you know, in the last 30 years, looking at statistics, there’s a higher incidence of it, but I kind of feel it’s like, well, you know, our writing group is better at finding it. So I think we’re finding it more than we were before, I don’t think it’s necessarily worse. But if you look at it with tying to dietary stuff, which we’ll talk about in a second, you know, obesity is a huge pandemic, also. And so it might be as a result of that. Also, it’s hard to say for sure, but, um, as far as a couple studies that I’d found, I saw one study in the Journal of Physiology from back in February of 19.
That did show that so these the study was small, I want to say it was like 20 people, maybe that had colon cancer, but they were they had survived it and it operated and all that stuff. But they still had some residual cells in their body with some sort of lab values, what they did is they showed that acute high intensity exercise, and they define that as four sets of four minutes 85 to 90% of your max, they would do those bouts, and then they would recheck their serum levels, I want to say like two hours, six hours and 24 hours after and then statistically significant decrease in the amount of cancer cells in your blood compared to the people who didn’t exercise.
So I’m interested in not saying that CrossFit will cure colon cancer, that is not what I’m whatever, but there’s some data that is showing that and they also had an increase in interleukin six, eight and tumor necrosis factor. So it showed some it was kind of interesting. So in a nutshell, basically, if you’re, you know, healthy, you can maybe prevent some of these things as far as with just diet and exercise alone. Another study that I’d found in cancer epidemiology from August of 2020, is basically reviewing mechanisms by which coffee can be protective against colorectal cancer and gastric cancer. Yeah, so I was excited about that. For whatever reason, it said decaffeinated appeared to be statistically significant better of downregulating cancer cells, then caffeinated. Whether that’s true or not, I don’t know.
But I personally drink coffee for caffeine. So I think my chances I guess, I don’t know. Yeah. But anyway, those are just a couple different things. But yeah, I mean, there’s different reasons why we developed polyps and or cancers, some of its genetics, you can’t really get around it. There’s been some talk about red meat.
Dr. Mike T Nelson
The questions I was gonna ask, because that always comes up like I know, acquaintances who are like, No, I stopped eating red meat because cholesterol and colon cancer and a little bit I poked around in that literature. I’m like, I don’t know I don’t think there’s a direct link but what is your thoughts?
Dr. Chris Morrissey
I don’t think there’s a direct link I think just in general that they’re looking at Americans as far as because it’s mainly in America more than anywhere else. But right, just our, our lifestyle of being more sedentary and eating crappy food and not exercising, I think that plays a big role. But like the red meat thing, again, kind of usually, the typical person you know, you have a big steak, you have a big huge loaded baked potato with everything on it and you’re not you know, in a in a soda or beer or something.
So you’re not eating healthy anyway, usually, but I think that’s what’s a bigger thing. I’ve never seen any direct like, yes, eating red meat equals colon cancer, but I think it just makes you more likely, but I don’t think it I can’t say for sure either way. And same with cholesterol. Like, I personally, I have high cholesterol. I’ve had it for years, and it’s genetic. And I’ve tried different things. I went almost vegan for one year. And I dropped like five points. And that fell off. I was like a full year. Good. turkey bacon. I mean, I was vegan, but I would just like everything healthy and it did nothing. And so I was well screw it. If it’s not going to help.
I’m going to just eat what I want and then exercise more or whatever. So but the one thing that did kind of derail a little bit for me Paleo Diet lowered my cholesterol by like 40 points. Oh, wow. That’s a big difference. Yeah, I’d read Rob Wolf’s book, the Paleo diet based on kind of got his background and I’d forgot the little mechanism for med school and I talked about excess cholesterol or excess carbs get converted to cholesterol. And so I was like, well, I’ll give that a try. And so I did it for like, four months and it dropped me from like, mine was up into like the 240 range my total and it dried got me down to about 210. And I didn’t follow my own rules I was teaching my medical students that rotate with me, it’s like always, you know, lab values is one time in space, it doesn’t matter, you gotta see where it was. And so I didn’t look at my previous ones.
And so it’s like, well, it’s still high. I’m going to go on a statin, because I’m going to be an adult. And then, so I went on for like six months, and I had a bunch of the muscle pains and weird cramps and weird injuries from lifting and running. So I was like, told my doctor, I’m like, Alright, I’m quitting this, because this is not helping me. It’s hurting me more than it is. So I haven’t checked it since then. But I still try to eat relatively healthy. And if I would have just given it more time, that might have been better for me. I don’t know. It’s just one of those things.
Dr. Mike T Nelson
yeah, I think part of that is also insulin effect on cholesterol production, if I remember right, I might be, yeah, accurate on that to the HMG. CO reductase. pathway, I think I think insulin makes it worse. So your body ends up creating more cholesterol, which is why if you look at data from unhealthy metabolic people versus healthy metabolic people, it’s like, completely two different worlds. Right. And almost all the data we have is from people that are kind of metabolic train wrecks where their glucose and insulin are unregulated and right, yeah, if you’re dumping a crap ton of carbs into that system, it’s probably not going to go well. You’re not exercising, you know, versus someone who exercises a lot.
Everything else is pretty good. Their cholesterol may be trending a little bit high, like, yeah, maybe play with a little bit lower carbs, do some stuff. I think it can be beneficial. But it’s, yeah, I think people over extrapolate from metabolic unhealthy people to recommendations for metabolically healthy people. And they’re just two different pathologies or physiologies.
Dr. Chris Morrissey
Oh, for sure. Yeah. And we just sometimes our numbers that we get things from, you know, not to derail again, but you know, the whole BMI thing. I don’t know if you’ve researched that much. Definitely. I did my own podcast that was my topic for this week is the BMI and how it’s pretty sucky and kind of talked about its origins or whatever, but it’s just, it’s all but we base everything off of that. And I, you know, yes, I check it. I mean, it’s not my paper, but you know, even me, I’m, I’m overweight, because my BMI is like 20 758 and weigh 181 85, just depending on the week or whatever, but it’s just like I, you know, yes. Do I have a six pack? No, but am I overweight? No, like, Yeah, but it’s just, it’s just not a good gauge of anything.
Dr. Mike T Nelson
Yeah. And going back to the colon exam? Yeah. What is the do you know about what the risk is of a perforation, because that’s the prep and like, the risk of perforations are probably like the two main objections I hear from people like almost all the time.
Dr. Chris Morrissey
So perforation, I want to say, it’s like the last numbers, I think, as like, 0.02%, or something like low, pretty low, possible, extremely rare has it happened to me, yes, it’s happened a couple of times, but it’s, you know, both times it’s happened, they’d had a bunch of previous operations and, and all that other medical diseases that made things more friable than, than others. And you know, it’s, it’s in risks, and we talk about it, and then if it happens, we go in and fix it, the worst part of it is, if you miss it, you don’t know that you do it.
Because sometimes at the time, you don’t know that it’s evident. You know, one of the times it happened to me is I had no idea it was just a small, tiny hole. And they came back 24 hours later to the emergency room with nausea, vomiting, abdominal pain, fever, and then got a CAT scan. And they had what’s called free air, you know, basically, where there’s a little hole in the colon and a bunch of air and abdominal wall or cavity. And so I’d go in and find the little hole and over, so it and it was fine. But sometimes we don’t know that it happens.
But yeah, it’s like, way less than 1%. And so it’s super safe, you know, probably I don’t know, statistically probably die in a car wreck before you get a colonoscopy. Perf you know, but it’s just unfortunately, with anything in surgery or medicine, there’s risks, and you just have to talk about them. And as long as you’re upfront about it, and, you know, be honest, and tell people about it. And if it happens, you know, super sucks, but you go on to fix it. And you know, it’s fine.
Dr. Mike T Nelson
So yeah, because I think people also have to be aware that there’s a pretty high risk of having colon cancer. So it’s not like you’re going in there for nothing.
Dr. Chris Morrissey
Right? If you’re going in and just doing it because you wanted it done, that’s something but if we’re actually looking for disease, and then you know, and then so if you end up having colon cancer and you know, having to have chemo radiation and or colon surgery, you know, then you’re going to have an operation part of your colon out puts you at higher risk for getting you know hernias later in life and or whatever. So it’s like from a fitness exercise standpoint, it may limit you after having it just because you I mean, some people have repaired and they’re completely fine. They can do whatever but other people are plagued with, you know, chronic pain and hernias and all that stuff. So a little to me going in with no cuts going in through the rectum. And if you can take care of things before it starts is way better than waiting too late. So for sure.
Dr. Mike T Nelson
And is there a blood test now for colon cancer? I’ve heard some rumblings that there is and some of the docs I talked to so Yes, but it’s not really that reliable and there’s sometimes false positives and the colonoscopy is still a kind of your gold standard. So yeah, if you’re gonna have a colonoscopy, why even bother with the blood test? Right?
Dr. Chris Morrissey
No, anything on that, as far as blood work, I don’t know of any specific blood tests. But you know, the, there’s the DNA sample that you can send in through the mail the color guard, you know, what’s advertised? Yeah. So it’s better than just because before, we would just do what’s called a fecal a call, or basically, you take some stool smeared on a car to put this little developer on there. And if there’s blood present, then it’s positive. But it’s nonspecific. So you could have had a little hemorrhoid, and our bowel moving been a positive for that, or gastric ulcer, or gastritis. That caused just enough bleeding to detect bleeding. But the cologuard is actually supposed to be better because it looks for actual DNA. But the false positive rate is like 15%.
Dr. Mike T Nelson
Some other data seems pretty high, if I remember right, when I just poked around a little bit, yeah.
Dr. Chris Morrissey
And so to me, I never recommend those. And it’s not because I’m greedy. And I want to do procedures. That’s not it at all. I don’t think it’s a good test. Because if it’s if it’s a false negative, that’s not helpful. Positive, it’s not helpful. And so, and out of all of the all the positive cola guards that I’ve seen, I think I’ve only found a polyp in one person, and they’ve all been completely normal otherwise. So I’ve never found colon cancer in someone with a positive cola guard, just in my experience alone. That doesn’t mean it doesn’t happen. But I just think it’s a good test. Just colonoscopy is by far the best for sure.
Dr. Mike T Nelson
Yeah, just throw it out there. Because some people are like, Oh, but I can get this other test. And I don’t have to do a colonoscopy. It’s like, yeah, yeah.
Dr. Chris Morrissey
The only reason I would recommend it is if they have like, way higher risk to benefit ratio, if they’re, you know, got horrible ejection fraction of their heart or they’re on blood thinners they can’t go off of or sure, you know, a lot of procedural risk. Yeah. So then I would say, Okay, let’s get this and follow it. But I otherwise I just recommend a scope.
Dr. Mike T Nelson
So yeah, awesome. Yeah, well, it’s number two on the list.
Dr. Chris Morrissey
So number two, we’ll go on to gallbladder, um, that’s probably one of the most common surgeries that I do. And again, we can kind of talk about whatever you want function. Now, what is a gallbladder do for people listening. So gallbladder is a little pear shaped organ that hangs out in the liver. On the bottom side. Basically, it’s a garage for bile, it’s kind of how I explain it to people. So your liver, Raj, it is. So the liver makes bile, bunch of it throughout the day. And so some of it gets stored in the gallbladder.
And so the way the gallbladder is stimulated, so like normal, natural sense, you eat a meal that’s higher in fat than your gallbladder, there’s a signal called coli Sista kinda under CCK, that’s released from your duodenal. And it goes up and says, Hey, we need help breaking this food down so that your gallbladder will squeeze, dump a bunch of bile down in there. And so help start emulsifying fat and breaking everything down. So it can be absorbed for, you know, nutrients and whatnot. So that’s the normal storage or the normal function of that, you know, most people, you know, they can get along fine. But some people, you know, they have problems.
So there’s kind of two big reasons to get your gallbladder Well, there’s more than two, but the two main ones I typically see is either you have gall stones, that is formed from over the years of bad diet and maybe lack of exercise, there’s some correlation between that or if it just doesn’t work properly. So if I get a patient in the office, that’s, you know, hey, I might have gallbladder disease, the first step we do is getting an ultrasound of the gallbladder. So go to radiology, like the jelly on your belly and look around. And so the, from a general surgical standpoint, I look for four things, I like to see if there is stones that are not, I like to see how thick the gallbladder wall is because a thicker gallbladder wall can indicate either chronic inflammation or acute inflammation or infection.
At the time of the scan, I also look to see how big the common bile duct is, which is the main bile duct that drains the liver. And then I look to see if there’s what’s called pericolo cystic fluid or fluid around the gallbladder. So basically just looking at anatomy, so if anything of that, you know, after doing a good history, physical exam, check and bloodwork and if you have stones, or it looks thickened, or whatever and your story fits with gallbladder disease, we’ll talk about taking the gallbladder out. Sometimes, though, you get in there, and they’ll just sound is completely normal. And then they’re like, Alright, what’s next? And so depending on what I think it is, if I’m on the fence where it’s like, Man, this could be stomach or this could be gallbladder, I’ll typically I’ll give the patient the option and like, okay, these are our options, we could either go continued on the gallbladder tree and do a different test, which I’ll talk about in a minute.
Or we can just go do what’s called an EGD, which is an upper scope, where we can go down and just like a colonoscopy, but you’re going down the throat into the stomach, and I’ll go through that in a minute as well. Looking for gastritis or peptic ulcer disease or you know, do tinnitus or something like that. So, this is based off where all the, you know, the embryologic origins of the gut, you know, the four gut, they all come from the same area, so some of the pain distribution is the same. So sometimes it’s really hard to figure out like, based off your story alone what it is because sometimes it’s a slam dunk. Sometimes it’s like, I don’t know good. The Flip a coin and pick.
Dr. Mike T Nelson
Yeah, it’s like abdominal pain. Okay. I mean, I think people sometimes forget that where you have pain, especially in the visceral area, abdominal area, the mid part of your body, whatever term you want to use. It can be sourced somewhere else. Yeah. You know, I mean, it could be like, I’ve got pain in this lower area, it doesn’t mean that there’s something going on in that area specifically, there definitely could be. But it’s not like, oh, point here. Oh, that’s the liver. Oh, there’s the gallbladder.
Dr. Chris Morrissey
Right. It’d be nice if it was that easy. But it’s that easy. But um, but yeah, so. So if we’re going down the gallbladder tree, the next step I would get is what’s called a high dose scan, which is a gallbladder scintigraphy. So it’s a Nuclear Medicine study, and it checks the function of your gallbladder. So your gallbladder might look completely normal, but it’s just not working well. So you go over a two part test, you get an IV, you get an injection of some dye that the dye will go up into the biliary tree and light up the gallbladder light up the hepatic branches. And then just to see if everything fills up properly. And then there’s a next step where they’ll give you synthetic CCK. And then your gallbladder empties, and then they calculate your ejection fraction of velocity and how much comes out or whatever. And they calculate how well your gallbladder function. So based off of that, we may go to the operating room and take your gallbladder out.
Dr. Mike T Nelson
It’s like a cardiac nuke scan, but for your gallbladder exam are familiar with that. Yeah, right. So you go in there, you light it up with a bunch of dye, and you see what happens. That is a dramatic oversimplification.
Dr. Chris Morrissey
Well, no, I mean, that’s pretty much what it is for sure. So. And what’s weird is, you know, the ejection fraction, what’s considered normal is greater than 35%, which, why they picked that number, I don’t really know that seems low, give you you know, look at any other percentile, that’s a low number. But but so if it’s less than 35%, that can be an indication as long as the story fits. And you know, because it can be, you know, if you’ve been fasted for a few days and haven’t been eating, if you’ve been sick, or whatever, from other entities, your gallbladder fraction can be lower, just because your gallbladder is not as full, and it sounded right functioning as well.
So it just got to go with the whole story. So less than 35% With and the other thing I always talk about is reproduction of symptoms. So if they’re like oh my god, it feels just like a day, when I end up in the ER, abdominal pain goes around to the right side into my back, like, I feel that’s a positive test, let’s go check out your gallbladder. If it’s above 35%, that’s considered normal. However, again, if it’s 50% ejection fraction, which is completely normal, but it’s exactly the way they felt, I don’t really care what the number is, I take the gallbladder out if it’s based off of that. And then in the last like three years, there’s been a new study showing that people that have hyper functioning gallbladder, so their ejection fraction is greater than like, 80%.
Because before we always consider that as normal, but I’m actually in the camp of believing that if you have hyper Kinesis, which is the word even though it’s a misnomer, but the movement, yeah, too fast or too hard, or whatever. But um, I’ve taken people’s gallbladders out for that I think I have about least 12 patients in my practice with that specific thing. And I would say all but one has gotten better, like they’re completely fine.
Dr. Mike T Nelson
So I’m not sure what’s going on with that, like, what do they present with the same symptoms, then are different symptoms?
Dr. Chris Morrissey
No, it’s same symptoms, it just water, but then it’s like, oh, well, your gallbladder function is completely normal. But then it’s like, so five years ago, I’m like, Well, it can’t be your gallbladder, it’s got to be something else go CGIAR do something different. But now that I’ve learned, I read that paper was out of like, I think it’s out of California. There’s a general surgeon that had like 25 to 30 patients that he was, he believed that there’s more to it. So he just took people’s gall bladders out, and I want to say like, 90, some percent of his patients all got better.
So I kind of based my, you know, practice off of that. And I’ve had really good luck with that. If it’s, you know, obviously the right problem. Because I always say, you know, I tell people, like, if you come back to me, thinking, I’m a magician that you feel amazing, then we did the right surgery. But if you come back and like I feel the same, it’s like, crown, chose the wrong. Yeah. Yeah,
Dr. Mike T Nelson
I think that’s something people should realize, too, is that I think there’s an assumption that physicians, even the best educated, most well intentioned physicians have all the data and that we understand everything. And that’s like so far from the truth. It’s like you’re doing the best you can always based on limited data, which means that you can follow all the rules, all of the best data, do everything to a tee. But it may not solve the issue, right? Because there’s so many things that we just don’t understand yet. For sure.
Dr. Chris Morrissey
And I always tell my patients out of like, this should help you I’m not gonna promise you, I’m not giving you 100% guarantee, you’re gonna feel amazing, because you should, but you might not. So as long as you’re on board with that, we’ll go ahead and proceed with your surgery and see what happens. So. So that’s kind of how I practice and there was a paper that came out, I don’t know eight or nine years ago that showed since laparoscopic surgery has been invented, like surgeons do too many gall bladders because it’s drive through surgery. come in and go home the same day. And in general, right upper quadrant pain does not always equal gallbladder disease.
And so sometimes we jump at the, you know, some, some people are more eager to do procedures and others as far as for whatever reason and so I’m I’m of the camp that I want to make sure that I’m doing it for the right reason not just doing it because I can. So I kind of really make sure I want to do it for the right reasons before I take someone’s gallbladder out.
Dr. Mike T Nelson
Do you think that’s a little bit of a carryover from lack of a better word old time physicians of just taking shit out? Like your tonsils? Don’t need them appendix, take it out gallbladder. I don’t know, that’s an oversimplification, I’m sure.
Dr. Chris Morrissey
There may be some truth to that. But, you know, I feel some of us that have trained more recently that were done a lot better. It has, and, you know, just doing it to do it isn’t again, always the right reason. But as long as you’re going to help somebody out, you know, but yeah, there’s some people that just, I can do this procedure, I’m going to do it because I can you know, and medicine, you know, there’s been scams over the years with different things that you read about different lawsuits for people doing unethical things. Unfortunately, it happens in our profession. But I like to think most people are out to help and not just, you know, there’s better ways to make money than doing it just to do it, you know.
Dr. Mike T Nelson
So I think we learn more about what each thing is doing as a function. Right? Because I think, you know, my guess is a gallbladder is probably doing more than just sequestering bile even though that’s its main job. And that’s what it does in life. Right. We used to think the appendix back who needs an appendix is just an extra vestigial thing that’s just hanging out there doesn’t do anything. Yep. Now we’re like, oh, yeah, it actually does some shit. Oh,
Dr. Chris Morrissey
right. No, I mean, it does have a function. It’s got a little bit of immune function. But you know, we always say God gave us an appendix for surgeons to have something to do. So yeah, that’s kind of what to say. But, but yeah, there’s in I’m sure, there’s a lot more stuff to gallbladders than we know. But, you know, obviously, people can live without him, because we do a lot of them every day.
And you know, as far as complications of the procedure, most commonly, you can have transient diarrhea, you know, after every time you eat, you go to the bathroom, and that’s just your body, your liver hasn’t figured out how to secrete more bile to help break down food, because normally it can rest when the gallbladder is present. Because then the gallbladder kind of does its job. And now the livers got to like, Hey, I got to pump out more bile over the day to help break down foods so you can be normal again. So that’s kind of one of the one of the things that can happen after gallbladder surgery, other than, you know, bile duct injuries and other things that can happen. That’s kind of the big complication, if you want to say, but it’s pretty rare to it almost always goes away, within three
Dr. Mike T Nelson
to six, I was gonna ask, do you know, well, how long that hangs out? Because that’s one of the questions I had is that, like on intake forms, like if I find someone is super sensitive to high dietary fat, I’ll ask them if they’ve had their gallbladder out. And sometimes it’s like years later, and they’re like, yeah, and in my head, I’m like thinking, what is kind of the timeline because the body is going to adapt? And over time, it’s probably going to figure this out. So is it just a coincidence that they’re having a dietary issue with fat and their gallbladder came out? And it’s not a bile issue? Or because they’re missing a gallbladder? Is it potentially a thing or who knows?
Dr. Chris Morrissey
It’s, it’s I don’t think we completely know. But what I tell my patients is on average, I say, it can be three to six months, I know I have one person in my practice that just has chronic diarrhea, every time they eat, they run to the bathroom, and there’s nothing I can do now, whether it’s other dietary things, I don’t know, I haven’t followed up with them for years, but, but in general, most people, they’ll have three to six months of possible diarrhea. I’ve had a couple people, though, they’re like, oh my god, two days later, I went and had a footlong chili cheese Kony amazing. It’s like, well, that’s the time we recommend a diet lower in fat, you know, in the short term, just make everything not work as hard and be easier on your system.
And I always tell people to it’s like, if there are foods that wrecked you before your gallbladder, just avoid those for a while. And then yeah, after a month or so just test it, just eat something and you’re not gonna hurt anything. You’ll just feel like crap, if you’re not ready to do that yet, but I would say three to six months is the general thing. So if it’s 10 years later, it could just be still a chronic, you know, with the called dumping syndrome after you know, gallbladder surgery, but it could be something else too. You know, it could be their gut microbiome is wrecked, or they’re, you know, some sort of other, you know, trash can diagnosis, IBS type of thing or something.
Dr. Mike T Nelson
So it’s hard to say, but is there any supplements or anything that may help with that in the transition period? Or do they just keep reducing fat and keep it kind of under sort of a threshold to their body adapts.
Dr. Chris Morrissey
Um, I haven’t learned any actual, like natural supplements that I know of yet. You know, there. People talk about bile salts or, you know, bile salts and ox bile and there’s yeah, I’ve never seen things out there, for sure. And I’ve never prescribed those and actually, that’s one things I’ve learned about in the functional medicine thing. So I haven’t gotten to that part yet.
But um, I would kind of tell people low fat diet, things that you know, bother you avoid those for whatever reason lettuce is a big trigger. And I don’t know why that is. It doesn’t make sense. But people have came to me before that there. Like, every time we eat salad and like what’s on your salad, you know, usually it’s eggs, bacon, fat, fatty ranch and all the things that you dress up to make it taste good. But sometimes you’re like, I just need like, a turkey burger with a little piece of lettuce and I’m just wrecked.
And so it’s like, okay, well, you know, so what? I don’t know why let us as a trigger, but that’s one that I’ve learned more often than not that people say they eat lettuce and it kind of makes me look at their gallbladder if they still have their gallbladder. Interesting. Well, yeah, it’s weird. I don’t know why that is. But yeah, a lot of times dietary things, you know, like talk about gall stones, you know, 80% of gall stones are made up of cholesterol. So typically, people that have a higher cholesterol diet, or, you know, that doesn’t mean they have high cholesterol, systemically just their dietary intake of cholesterol, that it’s more propensity to form gall stones. So the rest, like less 15% of gall stones are like calcium based usually. So but the majority of them are gall stones.
And it’s really weird. Everybody’s different. Like I’ve taken people’s gall bladders out, they have one huge one the size of an egg. And the Whoa, out is like sand. Some of them are pebbles. I took one guys out that had like a little 100 little rocks in there. So it’s just weird how different people make different things. And I don’t know why that is for sure.
Dr. Mike T Nelson
But yeah, obviously not in the vascular system, too, right? We just always assume that it was all plaque. And now there’s different types of plaque. There’s vulnerable plaque. There’s, when I did that section once we had a couple times just complete calcification of the vessel. And it was like a hard pipe. Yeah, it was just hard as a rock. You’re like, whoa, and it’s just so crazy to see differences in quote unquote, the same organ, you know, Oh, yeah. I always find that just fascinating, in a weird way.
Dr. Chris Morrissey
For sure. No, that is, it is crazy how different things are different, you know, and just when you’re like a member of medical school, some of our cadavers we had, like, 25 or so and we go around and look at different ones and just Yeah, people that are the same age, same reason they died and their organs are all just different and weird. It’s kind of crazy.
Dr. Mike T Nelson
So yeah, if you get the chance to do fresh tissue stuff, too, is that just the colors are different the arrangement like the size of stuff like it’s, it’s crazy to see how different people are one from the other but yet at the same time, similar, right? It’s like and then you get into all just the, the wacky pathologies which I often joke that it’s if most of the time everything goes right, but if something goes wrong, there’s a path ology for it and almost anything can go wrong from like, weird shit like dextrocardia where your hearts on up it’s like rotated and flipped on the other side and all sorts of crazy stuff.
Dr. Chris Morrissey
Oh, yeah. One of the craziest I saw in residency we had a 16 year old kid that came in with appendicitis. But he had total situs and versus where all of his organs backwards. And it was I’d never seen that before. I’ve never seen it since. But, so yeah, you just everything was complete mirror image. So we had to take his appendix out from the left, you know, the patient’s right side over to the left side, that’s where the appendix was, but everything else was, it was just crazy. And so I think I was like a fourth year residency. And so you have five years of residency. And usually by the time you’re up there, you do surgeries by yourself, but my attending kicked me to the side, he’s like, you’re not doing this. I’ve never done one of these either. So on but yeah, so that was, that was pretty crazy.
Dr. Mike T Nelson
I used to work for medical device company. And so I had observe a lot of procedures, I worked on technical service. And so they’re putting in a pacemaker. So they put the device in and they have little wires, they run down into the heart. And so they’re going in through the vessel, they usually get access, you know, right up at the top part of the ribcage. And they put a little wire in, and then they run the leads over it. And so we’re all watching on fluoroscopy, which is just fancy X ray. And we’ll look at the little wire and we see it go in, and then we see it because fluoroscopy is just 2d, right. So you’re just looking at the scan in lifetime, straight down.
And we see a wire which appears to go straight into the lung of the patient. And everyone in the room just like stops. And I’m standing behind the anesthesiologist and I’m looking at the monitors, and monitors are all fine. And for like half a second, a couple of seconds to the you know, even the main Doc’s like looking around. And then nothing drops. And they realize the patient has what they call persistent left main, where the vessel structure actually takes us completely different paths somewhere else. And so they were still in the vessel, they hadn’t punctured into the lung. It’s just this weird anatomy thing that makes it look like they’re in the lung because you’re looking at just this 2d view and they verified it and switch the views and stuff and they’re like, Oh, thank god. Oh, that’s good.
But it was crazy because I’m standing there and I’m going oh, I’m like started back in a way I’m like all the shirts gonna hit the fan now and everyone just stops and I’m like, oh, here the patient didn’t crash. This is good and like what’s going on? Yeah, see all sorts of weird stuff at times.
Dr. Chris Morrissey
Oh, for sure. Yeah, absolutely. So cool.
Dr. Mike T Nelson
Anything else on that any sort of preventative thing? I should know or so those possibly that they should talk to their doc?
Dr. Chris Morrissey
Yeah. So one study I read, basically, you know, increased activity can lower risk of gall stones. So basically, again, it kind of goes with, you know, obesity and diabetes, metabolic syndrome can cause an increase in gallstone formation just because you’re not healthy things aren’t moving through properly. Usually diet is bad. So again, you know, that’s one option, you know, there is one medication on the market, it’s called active all that supposedly dissolves gallstones, but it doesn’t work, I think. It’s great.
It takes over a year to even maybe be blue, but everybody ever prescribed it for because they want to be, you know, all natural, and I’m completely on board with that. And I was like, well, I’ll give this medication. But when you’re ready, call me and I’ve got all of their gallbladders because they were like, Okay, I’m taking this for five minutes, it’s not doing anything I’m ready to. So that’s one way, you know, or just trying to, you know, decrease your cholesterol intake, doing more of like a Mediterranean style diet, that’s kind of been shown to do that. And as far as exercise, also, you know, exercising does not prevent gallstones, but usually more of a healthy lifestyle, thus, you’ll be less likely to make them and so it just kind of goes hand in hand with everything else. Cool. So that’s kind of the main thing with that.
Yeah. So then there’s other like, oh, there’s like a, some sort of visceral manipulation techniques that can be done that some people really believe in, I’ve taken a course on it before. And it’s kind of different. So like, there’s, there’s a technique called gallbladder flush, which basically you kind of get behind them, you put your hands underneath the ribcage, and basically milk the gallbladder. And there’s studies shown that people had gall stones before then they ultrasound them after the gall stones are gone. So you can kind of manual manipulation type of thing, but I’ve not really done much with that. But I know it’s out there. So some people looking for, like a visceral medicine or visceral manipulation specialists can go to get different entities done, you know, supposedly breaking up scar tissue or you know, making hiatal hernias less painful by massaging the sphincter, you know, the G junction or whatever. So there’s a lot of other alternative medicines out there you can do but it’s not really mainstream medicine.
Dr. Mike T Nelson
Do you do any of this for work? Since you have kind of an osteopathic background? That’s usually bigger and osteopathy?
Dr. Chris Morrissey
yeah, we learned like, it’s kind of like nutrition, we had one course on it, we did it once. And so I actually took a full course of it back in August of last year, I went up to Denver and did a three day course, and it was, I haven’t practiced it much. It’s just interesting concept where you can, you know, just basically palpate and try to see if there’s an organ dysfunction based, there’s like your organs make these little movements that are very subtle that you try to find that and you can augment their movements to try to increase disease whether or decrease disease symptomatology and I just haven’t done enough of it to know if I buy into it or not. There’s a lot of people out there that do it, though. And so I feel just like anything else in life that if a lot of people do it, there must be something to it, that if like one crazy person only does it then it’s like, well, maybe there’s nothing to do that. But there’s a lot of people that buy into it big time.
Dr. Mike T Nelson
yeah, a buddy of mine from Australia came over to the US and did like a whole week with blanking on who was like The Godfather of visceral stuff was a guy named John Pierre Burrell.
Dr. Chris Morrissey
Who Yeah, that’s it. Well Institute he’s the guy that kind of crazy. He’s a French osteopath, that kind of Yeah, it
Dr. Mike T Nelson
was the French osteopath. And I don’t know if you followed him or one of his underlings around for like a week was super expensive. He flew all the way over from Australia to do it. And I asked my dentists that how was it? He goes, it was good. It was very interesting. I’m, like I said, my interpretation, which is overly simplistic is, it’s no different than any other type of massage, you just have a lot of organs and stuff there that you’re working around, like, the principles are the same. If something doesn’t feel like it’s moving, you’re trying to get it to move a little bit better, obviously can’t use high pressure. And he’s like, Yeah, after paying, like, I know what he paid like five or 10 grand or some a lot of money. He’s like, That’s pretty much it, and you just practice a lot.
Dr. Chris Morrissey
That is pretty much like for sure.
Dr. Mike T Nelson
Okay. you know, like anything like you get into these sub niches of people who are like, Yes, I rearrange their uterus, and they have kids now you’re like, Ah, I, I want to see some proof of that, you know, see, you have like the end of that. But I’ve just done with even just on hands on work here in Minnesota, that it’s super useful, because a lot of people who have like breathing stuff going on like real simply right, the diaphragm has to come up and go down and the viscera, the organs have to move up and down a couple inches.
Yeah, if that whole area for lack of a better word is just stuck. Then it just impacts just breathing mechanics. Yeah. I remember asking Tom Meyers this once I did a bunch of work with him. Because before I left for the training, and people were just giving me a bunch of shit for doing visceral work. And I asked him that and he’s like, we looked at me, he goes, yes, the viscera has to move up and down a couple inches and just kind of walks away. Like, why are you asking me this? Of course it does.
Dr. Chris Morrissey
Right. So you know, there’s a lot of things to that, you know, like I do when somebody is in like, there’s different ways to increase parasympathetic tone or decrease sympathetic You know, like a common use after surgery is people have a post op alias where, you know, their bowels are asleep from anesthesia or manipulating the intestines or whatever. So you can do some, like, work on the paraspinal muscles to, you know, increase parasympathetic tone to help them start moving.
So there’s some data that shows that’s pretty helpful. So there’s a lot of other things we can do. The sad thing is, is osteopath in general, you know, prob about 10% of people, you really use it, and it’s just kind of a, like, I don’t know, I guess a comfort level, like I took interest in or I feel very comfortable. And I bet 10% of my practice is just manipulation. So I’ll get people into my office just to you know, fix their neck, fix their back, whatever problems are having. And so I’m a big believer and all that. So I always feel it’s worth trying. It’s not gonna hurt anything, you know, as long as it’s not contraindicated. You’re not doing anything crazy. It’s why not?
Dr. Mike T Nelson
I mean, you know, it’s, it’d be helpful for sure. So yeah, cool. You got time to go over the last one. You okay, for time?
Dr. Chris Morrissey
Oh, yeah, no problem. So the last one we’re going to talk about is like gastric ulcers. Gastritis in general. So, you know, so people can have upper abdominal pain, and vaguely some, you know, typically it’s very shortly after eating, it can be certain foods spicy or acidic foods like citrus, pineapple, things like that. People that take a lot of anti inflammatory medications, so ibuprofen, Aleve. Aspirin.
Stress is always a big trigger, as well, I kind of always put that at the end of the list. I always look for bad things first, and then if nothing else looks fine, it’s like oh, how stressed Are you? Oh, I’m a lot of stress, okay. A lot of alcohol consumption smoking. There can also be a bacteria called H. Pylori, are going to come back to pylori that can cause gastritis and gastric ulcers. So the only way to really diagnose that is off of endoscopy and biopsy saying there is a stool sample you can do that’s probably the most accurate of the non invasive testings for H. Pylori, but that the best way is into scopic, you know, visualization with biopsies.
Dr. Mike T Nelson
And that’s positive, you get to do antibody discovery of that, like it used to all the stress and wasn’t the main researcher who discovered it, so to speak, didn’t he give himself H. Pylori and give himself an ulcer and had an image, I think, sort of as an end of one to prove because no one else believed him. And they told him he was full of shit, right? I’m pretty sure that’s how that went down.
Dr. Chris Morrissey
Yeah, it could be just a rumor, but it makes a cool story. For sure. Kind of like the guy that, you know, came up with the idea of washing her hands after surgery or in between cases, little animals that lived on us that are bacteria.
Dr. Mike T Nelson
Nobody knew that, like why you’re crazy, man.
Dr. Chris Morrissey
Yeah, for sure. So, but, um, but yeah, so that’s the most common thing you see is abdominal pain or whatever. And so to me, I like to know what I’m treating instead of just giving them an anti, you know, like an h2 blocker or, or a a proton pump inhibitor, like an F Risala. Promise, like, I like to scope them to see especially that never had one before. Now, if they’ve had a scope as a year ago, usually it’s like, Okay, let’s get you back on your medication. Let’s try avoiding certain foods. Let’s try, you know, how much caffeine Do you drink?
How much how much do you sleep and try to do lifestyle modifications, but But if people you know, increase your exercise, and they really cope with their stress, well, they can stop smoking and taking alcohol and or, you know, increasing their sleep that’s been shown to be helpful. There’s a couple studies that I’ve read recently that during exercise, so basically, your blood if you’re especially like endurance athletes, where you’re out running for long periods of time, your blood gets all shunted to your skin and your muscles and your gut takes a hit just because while we’re not using it right now, so you just have to dig ahead, and you can get like, I want to say that the study that I read, if you’re exercising around 70% of your VO to Max, you get about a 60 to 70% Decrease in your splanchnic blood flow. So you’re only getting you know 30% of your blood flow to your organs like you normally do.
So you hear about, you know, marathon runners getting severe diarrhea during running just because they have no blood flow to it from ischemia. So another thing that I read is that you can exercise can increase serum oxytocin levels, and if you’re given exogenous oxytocin, it has an anti ulcer effect. So, in theory, I think people think that if you by exercising more, you’re triggering internal or intrinsic oxytocin that may help with anti ulcer formation. So that’s something that’s kind of in the literature that’s been shown. Another thing is taking Tumeric Tumeric got a lot of a lot of properties that you can use, but it’s been shown to be anti inflammatory, anti cancer, antioxidant wound healing. So the curcumin which is in it, it’s about you know, two to 5% of the Tumeric acid and so it’s got properties like vitamin C and E, as far as the antioxidant properties. But there was a study that they did basically they had people I think it was endurance athletes again, where they had them go out running, and they had the same program, but one arm got tumeric and one didn’t.
And the ones that got Tumeric were they they they showed to be severely like gastroprotective so they had less, less incidence of ulceration formation, just from exercise. asking too much or whatever. So it’s one of those things where I feel that it’d be worth looking at, as far as taking out if you can paint a letter you want to or whatever.
Dr. Mike T Nelson
Do you have any preference on the type of tumeric. Because historically, the bioavailability is kind of crappy. So there’s people who put it in, you know, fighters ohms. And supposedly, like with spirit and putting it with a little bit of oil, or do you have any? I personally on that,
Dr. Chris Morrissey
I personally don’t, I haven’t really prescribed it a whole lot. I’m still kind of tinkering with this stuff, you know, so I don’t have you know, I kind of just tried to research to see what you know, less ingredients and things. Yeah, probably won’t get it from Walmart, I’d probably a little more money, for sure. But yeah, I don’t have a brand or anything that I like, endorse or whatever. I’m just kind of like, well, you know, go get it. You know, I’ll research here’s a couple, you can give it a try and see what you think and whatever. But I haven’t prescribed it a whole lot.
Dr. Mike T Nelson
yeah, number iva, that’s a trade NET Brand has some interesting data on it, too. And oh, Thoren has that and some other companies do. So I’ve, I’ve used that. And I’ve used versions that have a little bit of coconut oil with it. And it’s anecdotal. I can’t say I’ve noticed the difference per se between people. But yeah, that’s interesting.
Dr. Chris Morrissey
Yeah, for sure. So and as far as you know, preventing gastric ulcers, because, you know, if you let them go too long, you can lead to what’s called a gastric perforation, or you come in and overnight with a hole in your stomach. And, you know, it’s kind of, it doesn’t happen very often anymore. But kind of a, it’s kind of weird. Some pathologies like appendix, they’re kind of like I think it started a day or two ago, but usually with gastric purse, or like it was 817, I was watching TV and this habit, it’s very specific of when it happened.
And to go in and fix it. Basically, you just go in and you can just oversell the hole and drag a little bit of what’s called your omentum, which is the kind of fatty ape and that hangs off your colon, we use that as what’s it’s called, it’s like a plug in patch, basically, you just go over pull the momentum over, it’s so that down and kind of plug the hole and then you put an injury to bounce them for a couple of days and make sure there’s no leak, and then you can take it out and start feeding them.
And so you don’t have to do this big gastric resection or, you know, like a gastric bypass type of thing that people get. And it’s kind of a non, it’s still invasive, but it’s less than it used to be years ago. So that’s kind of would be a good reason to, you know, prevent this happening is having a hole in your stomach and you got to go in and so yeah, for sure.
Dr. Mike T Nelson
Do you see, like PPIs? Right, so proton pump inhibitors, as you mentioned, are one of the main drugs used to treat that? Do I just see more clients now coming in on them? And to me, again, I’m not a physician, but it it makes sense to my brain in the short term, but I always have them like, like, go back to your doc and ask him like, are you going to be out in this like the rest of your life? Or like, what’s your plan to kind of get off it? And a lot of times, they’re like, I don’t know, they just told me to stay on it, which is, from what I’ve read, I don’t know if that’s the best idea.
Dr. Chris Morrissey
Yeah, the high dose long term use has been shown to like chronic kidney function, right, fine, and everything like that. And it just depends on the person because typically what I do if I sculpt somebody, and they’ve got pretty bad gastritis, or ulcers or whatever, I’ll put them on. Like, my go to is a mint Rizal or process because it’s been around the longest, and it’s cheap, and it works. So I’ll put them on that twice a day. And then I also give him sucralfate, or carafate, which is a medicine, they’ll kind of coat the stomach. And so you you take them together. And so the thing about that when that sucks is you got to do it four times a day to be completely effective. If you take it three times a day, it’s still pretty good. So the the carafate I’m typically haven’t been on it for a month. So once they’re off once they’re done with a month and I say okay, you run out of that medicine, you’re done.
And then usually I’ll tell them is like okay, drop from twice a day to once a day on the prowl a second, see how you feel. And within a day or two, if they’re not ready, then they’ll be like, Oh my god, I felt like crap. Again. I was like, Alright, go back on it for another month, twice a day. We’ll see how it goes. And I always try to get people off of them. But there’s just some people that I don’t know you live in the Midwest, also. But in Kansas? Yes. People come to see me or they you know, they love fast food.
They don’t want to women want to do other changes, right? Yeah. Yep. So then they’re stuck was like, Well, you know, okay, I guess be honest, for the rest of your life, if you won’t do any of their lifestyle changes, because it’s really hard to you know, as you know, to get people to change. And so it’s like, alright, well try to go off if you can, you know, but then if you’re there’s been some disease processes that you have less gastric acid, you know, that you can lead to other, you know, gut problems or whatever. So you get in this big, vicious circle that you can’t get out of sometimes.
Dr. Mike T Nelson
yeah, because then I’ve seen it’s like you said the catch 22 of now they start having digestion issues going on that they didn’t have before, but they probably need to be on the med because they’ve got the thing going on in the stomach. And I’d right yeah, that’s what makes me nervous about people long term. And I get it like, if you’re not going to do anything to change your lifestyle, then you’re kind of stuck with what you have. But I think sometimes physicians don’t explain to them that, hey, here’s what’s going on.
Here’s our plan of what we want to do. Oh, and by the way, this involves you changing your lifestyle and you know, some people are gonna want to do that. Some people won’t. But I think it’s probably easier because so many people don’t want to do any lifestyle changes. You’ve got 15 minutes to talk to someone, do not give them the potential option either, you know, because that’s more work more interaction in the back of your head, you’re probably going to 90% of people don’t do it at all. So I get why there’s not always the option of you know, here’s kind of the long term plan to write.
Dr. Chris Morrissey
And typically what I always do too, is I was you know, I think you know, with polypharmacy in America, I always look at medicines, I’m like, well, couple these are, could be causing your problem, you know, you’re on, you know, chronic Meloxicam for your low back pain and, you know, taking not twice a day or once a day or whatever, can cause ulceration.
So I kind of try to find medications and see if we can stop them. Also, that may help or if you’re taking ibuprofen every six hours, it’s like, well, let’s try not doing that and get better, right? And so, but a lot of people don’t I always give them options. I’m like, Hey, if you want to do lifestyle changes, you know, I like doing those things, come back and see me, we’ll sit and talk about it. And I bet maybe one out of every 100 Actually do don’t want to and it’s so frustrating for me, it’s like, help me help you. I’d love to help you. And I’ll block off time just to talk to you. But most people just don’t want to I just wanna take a pill and be fine and whatever.
Dr. Mike T Nelson
yeah, if somebody doesn’t want to do lifestyle changes, what would be like one of those top three things you would look out for that? I mean, from what I’ve read, it’s, it’s pretty hard. Like I have one client, I’ve got a couple of clients who’ve had it and like the literature, I’ve pulled on it for lifestyle stuff, it just seems like I’m so take a shotgun at a target and just kind of start guessing stuff.
Dr. Chris Morrissey
Yeah, for sure. You know, and it’s, it’s, again, if there’s easily modifiable things, which definition of easy depending on who you are, but like smoking alcohol, right? Um, you know, acidic foods, stress, likes, all those things, you can get those in check, I think that would help a lot. And then again, looking at medications, or, you know, whatever, but everybody you know, it’s like,
Well, every time I eat pizza, I feel like crap, but I love pizza. It’s like, Well, okay, you know, another choice. So, it’s, most of it comes down to lifestyle modification, you know, weight loss has been shown to help with reflux disease, you know, and all of that, too. So, just, as far as non lifestyle changes, there’s not really a lot that I can work with with that. So I can’t even really speak on that, because a lot of it on the patient, they’re going to do it they’re going to do so sometimes it’s really hard to deal with that.
Dr. Mike T Nelson
Yeah. Cool. Awesome. Any other concluding thoughts, and we’ll give people where they can find you.
Dr. Chris Morrissey
Um, I mean, just, you know, get your colonoscopy be healthy, you know, do some sort of exercise that can you can change a lot of medical problems, and I feel, you know, diabetes is a complete lifestyle disease. I mean, yes, some people are plagued with genetics, and, but more often than not, it’s just, you know, lack of education on diet and exercise. Just try to be as healthy as you can, if you don’t like going to doctors, well, then, then be a better human for yourself. That way, you can avoid seeing people like me, maybe, you know, but that’s, you know, that’s pretty much it. I’m out here to help people if they want to be helped, you know, and I just love doing this kind of stuff.
Dr. Mike T Nelson
That’s awesome. I think you also highlighted how much of an effect exercise has and I know, that seems like a like, Duh, like kind of statement. But, I mean, I went to school to be an exercise physiologist. And like, every day, I continue to be like, just massively impressed about the effects exercise has on almost everything in the body. And this is an area that is like, incredibly, like, under studied, right, because no one’s really paying for a lot of these studies. Right? It’s an area that we don’t have a lot of data, almost all the data we have so far shows that it’s beneficial to literally almost every organ system and cell in your body, which just continues to like, fascinate me.
Dr. Chris Morrissey
Oh, yeah. I mean, between the, you know, fasting for like a toffee G and just getting out and walking, you know, some people they equate, well, I can’t run, you know, America, I try, it’s like, just don’t walk. I mean, I’m all about simple you know, you don’t you don’t go to the gym, you know, getting memberships, just put on your shoes, go out, walk for 15 minutes and come back in 15 minutes, three times a week, start with that and then things get easier just getting started.
You know, as you talk in your different classes and courses that you offer, you know, just get going and do something is better than nothing. And because some people just equate they gotta go, you know, do CrossFit or go Do you know, heavy weightlifting which I’m a huge proponent for resistance training has been shown to be beneficial more than anything else. But if you don’t want to do that, get up and walk or just do you know, Chair squats, go home and stand up out of your chair 10 times holding the can of soup or something or it’s, it’s so easy to do, because nobody wants to take the time to do it.
Dr. Mike T Nelson
Yeah, and that’s the benefit to have. If you are untrained and you’re listening to this and you’re not doing a lot of formal exercise. The the benefit you’re gonna see from like, zero to like one, like one day a week is massive, right? Just doing something you’re gonna see so much of a benefit, like if we look at the amount of exercise it takes to slightly lower blood pressure. It’s not that much exercise, right? These are all untrained people. Like you can kind of be you and go to the gym and get better for the first several months.
Right. So I think that’s actually something that my profession has done a very poor job of explaining to people, because it’s still, oh, you got to walk, you know, 10,000 steps a day or your slog, and people like, I can’t do 10,000 I’m not even doing anything. It’s like, if you did 5000, you would see a huge benefit from the 2000 you’re doing right now. I think we do a poor job of kind of overselling the high end and underselling just do something, and you’re going to be better and just start there, like, move where you can, and then get a little bit better over time.
Dr. Chris Morrissey
So that’s, that’s my blog, for sure. Oh, yeah, you know, and it’s so hard to get, it’s hard to get started. But once you get going, you feel better. You know, I know when I’ve had an exercise for about two or three days, and just irritable and whatever, and just, like go to the gym, you know, I just got to go out and run and go lift or something, and I feel so much better. And you know, your cognition is better, you just have all these health benefits that you don’t think about that. Just Just do something, you know, and just do something you like, you know, if you hate running, don’t run, you know, go ride your bike, go swimming, there is an aerobic exercise, you can do that. I don’t think you hate every single thing. Just find something that you enjoy, and then do that, you know, it’s not just going out to train for a half marathon or whatever. Just do get up and walk, go. Yeah, whatever.
Dr. Mike T Nelson
You know, do recreation. Like go do Brazilian Jujitsu, do tennis, do something that your brain has to think about. Obviously, be biased, go learn to kite board or whatever. Yeah, but get movement, do something you enjoy, get some brain function. You know, that’s a easier starting point than even formal exercise for a lot of people. So absolutely, yeah. And where can people find more about you? I know you’ve got some info. You’ve got a super cool podcast if people want more of the intersection of fitness and medical stuff. Yeah. So
Dr. Chris Morrissey
I started a medical fitness podcast probably about I don’t know three months ago now. It’s called the Morrissey movement. So you can look at it all the main podcast players on Apple Google
Dr. Mike T Nelson
spot on how do you spell that for people who are bad spellers like
Dr. Chris Morrissey
Morrissey Movement. So that’s my podcast, and you can just Google it. And I use Captivate for my podcast hosting that can take you to that website, and you can listen to it off of there, or you can go I actually put them on YouTube. Also, I have a YouTube channel, there’s no video I’ve just been making audio for now. But probably someday I’ll do some video stuff. But it’s fairly easy to find.
And then the same email address that morrisseymovement@gmail.com You know, I’d be happy to take any, you know, either ideas for topics to talk about and my target audience is pretty much general population, I don’t target to you know, medical professionals or you know, fitness, you know, high end people, just general public and I usually pick one thing in medicine and one thing and fitness and try to time together. And a lot of my caught my content comes from just questions I’ve been asked as a physician over the years, like, you know, what’s the colonoscopy?
What’s it like your gallbladder out? And so I just go through simple things. I don’t use a lot of big medical jargon. I just tried to make it simple to understand. And simple short to the point. Sometimes I ramble, but not a whole lot. But yeah, I’d be happy to, you know, talk with anybody or do whatever, I love the stuff. So hit me up, I’d be happy to help.
Dr. Mike T Nelson
yeah, I’ll give a plug for the podcast, too. I think if someone’s listening to this, and they’re a coach or a trainer, most of the time, you don’t really get much medical training, but you’re going to have clients that will ask you medical questions. And of course, yes, send them back to their doc, of course. But I think if you can provide any background or character or that’s kind of also why haven’t you on this podcast, I think it’d be helpful, then go listen to your podcast in more kind of plain speak and have more things they can tell their client about, you know, colonoscopies, or even BMI or other topics. I think that’s an easy way for them to just get a little bit more educated on those things.
So that when those questions come up, they can give them a little bit more context and hopefully then the client is more likely to actually follow up with their own physician and and do something then. So absolutely. Awesome. Well, thank you so much for all your time today. I really appreciate it. This is super interesting. Now.
Dr. Chris Morrissey
It’s been a blast. I really enjoyed it. Thanks for having me on.
Dr. Mike T Nelson
Thank you so much for listening to this podcast and this episode with Dr. Chris Morrissey really encourage you to check out his podcast, I think it’s a very cool intersection of medical and fitness. And I think it’ll answer kind of a lot of, you know, just questions people have. Unfortunately, a lot of people I know don’t even have a general physician right now. Or if they do try to get a hold of him or her is very difficult. So trying to educate yourself as best that you can, again, not looking to substitute advice from your doctor.
But I think everyone should be educated to their best ability on all matters, health, and even basic exercise performance and nutrition. That’s all I wanted to have Dr. Chris on the show to talk about those three common procedures, that guarantee that are either going to apply to you or to someone that you love. So feel free to forward this podcast to them make sure to check out his stuff. As always, we’d love any type of review you want to leave it just takes a couple seconds really appreciate it. And subscriptions also help bump up for the podcast and all the ratings.
This one is brought to you by physiologicflexibility.com, go there for a complete system on how to increase your ability to recover faster, increase your longevity and just be much harder to kill everything from cold water immersion to sauna to breathing techniques to high intensity exercise training or hit ketones, glucose, the whole nine yards and we go through the big picture to understand the complex concepts of it. Then we break down a lot of Have the research. And then I show you how to specifically apply it with five action items per area.
So there’s four main interventions each have two sides. So that’s eight areas, and there’s five interventions per area. So that’s 40 different action items you can pick from, again, not expecting you or your clients to do all of them. But it’s just giving you options in a system so that you can match the correct action item for more yourself or your clients are at to go to physiologic flexibility calm. Yeah, big thanks to Dr. Chris Morrissey for being on the podcast. We will see you all next week.






Leave A Comment