Join us on this episode of the Flex Diet Podcast with Dr. Shaun Kornfeld, a functional neurologist at Plasticity Centers in Denver, Colorado. We discuss how the functional neurology approach works to improve brain function by identifying deficient connections in the brain and prescribing exercises to stimulate these areas.
Discover the incredible potential of functional neurology in treating conditions without a specific diagnosis, such as developmental delays or concussions. We also discuss the limitations of imaging in diagnosing brain conditions and emphasize the importance of alternative approaches.
If you enjoyed this podcast, you can get more from me at MikeTNelson.com/podcast. You can see all the other podcasts and guest episodes I’ve done. And then if you scroll down, you can subscribe to my Fitness Daily Newsletter.
Episode Chapters:
-
(0:00:01) – Functional Neurology and Brain Rehabilitation
- (0:12:43) – Eye Function and Vestibular Insight
- (0:18:11) – Discussion on Sensory Mismatch and Symptoms
- (0:26:49) – Rebuilding the Brain’s Perception Systems
- (0:37:55) – The Importance of Summation in Rehabilitation
- (0:46:03) – High-Level Case Studies in Neurological Rehabilitation
- (0:54:04) – Seeking Treatment for Brain Injuries
Contact Dr. Kornfeld:
- Email: skornfeld@plasticitycenters.co
Referenced Links:
- Plasticity Centers
- Plasticity Centers/Shaun Kornfeld
- Dr Schmoe at The Functional Neurology Center
- The Carrick Institute
Rock on!

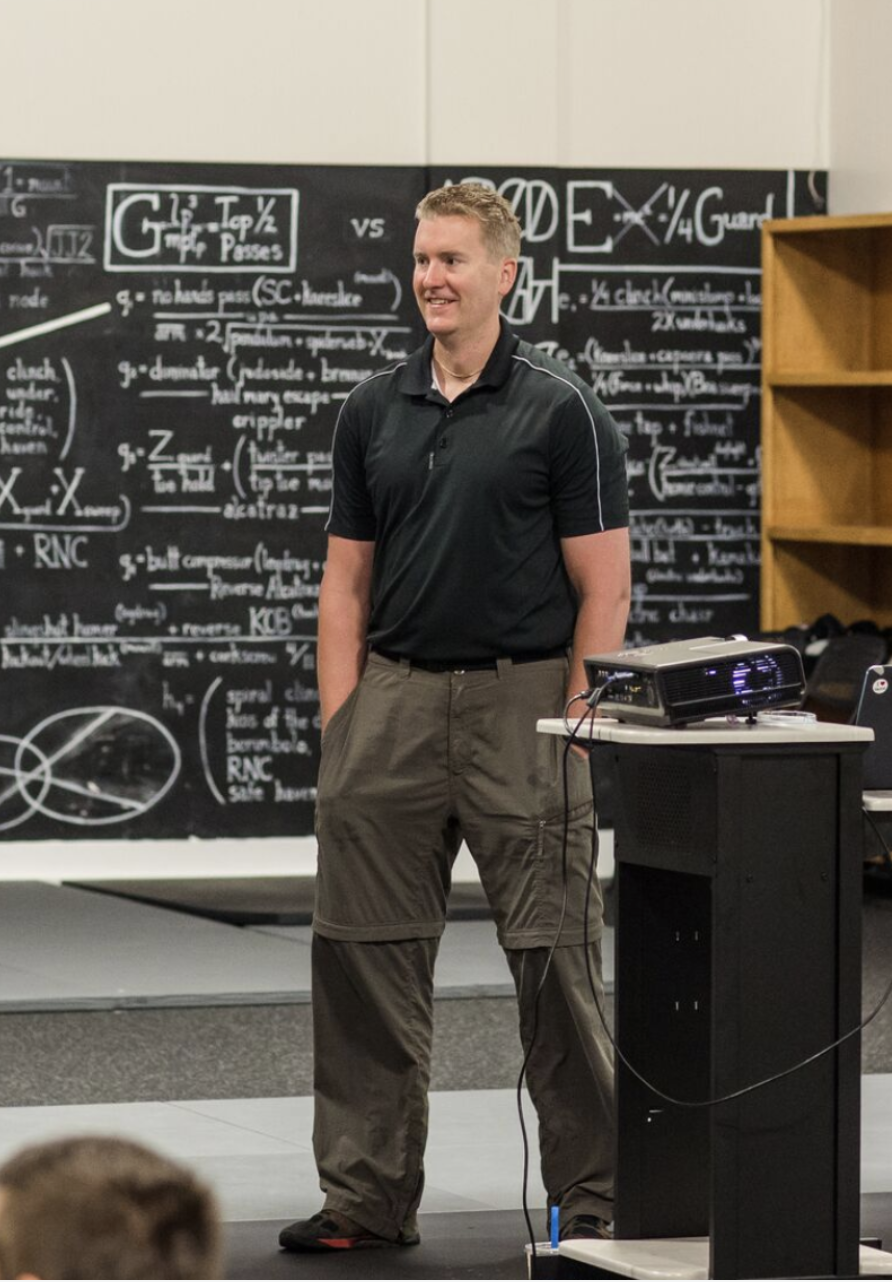
Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
[00:00:00] Dr Mike T Nelson: Hey there and welcome back to the FlexDiet Podcast. I’m your host Dr. Mike T. Nelson. I’m actually recording this from the road. We are just, we’re in Austin, Texas for a little while. Now we’re in Weatherford, Texas and wanted to let you know that this podcast is with Dr. Shaun Kornfeld. He is a Functional Neurologist at the Plasticity Center in Denver, Colorado.
[00:00:28] You might be wondering, what the heck any of that has to do with performance, and that’s what we’ll learn all about in this podcast. You can think of Functional Neurology or Clinical Neurology work as trying to figure out what part of the brain needs more trxaining. We know that the brain is what they call very neuroplastic, that it can be changed.
[00:00:53] And this could range from many different pathologies or concussion, TBI, traumatic brain injury, or in my case, just trying to get a better vision in terms of getting both of my eyes to work better for more binocular vision instead of monocular. And we talk all about that with him here. We did have some recording issues when we recorded it.
[00:01:20] We did try to put it back together as best we can. So please bear with us. There’s a couple spots where it is a little bit funky and if it jumps around a little bit bear with us. But I thought the information here was really good. And obviously I’m biased since I work as an associate professor with the Kerrigan Institute which Dr Kornfeld has done a lot of training with also.
[00:01:43] So we’ll put links to his clinic there. I’ve referred a couple people there where they’ve been very happy with their results. I’ll put a link also to the Kehrig Institute where you can get a lot more information there. And the main reason for doing this is just wanted to expand your horizons of different treatment options.
[00:02:04] And even though I’m associated with the Kehrig Institute, I don’t have any other disclosures with their clinic or anything else. You can find functional neurologists in many different areas now too. Personally, I’ve worked with Dr. Jeremy Schmoe who is in Minnesota, does some great work. A good buddy Dr.
[00:02:23] Matt, the Center for Plasticity down in Florida does good work and there’s many other places you can find too. So enjoy this podcast here on Functional Neurology and More with Dr. Sean Kornfeld.
[00:02:38] [00:02:38] [00:02:38] Dr Mike T Nelson: Welcome back to the Flex Diet Podcast. And today we’re going to talk about the area of clinical neurology or functional neurology. So, how’s it going?
[00:02:52] Dr Shaun Kornfeld: Hey there, Mike. I’m doing great. Thanks a lot for having me. And very excited to be
[00:02:56] Dr Mike T Nelson: here.
[00:02:57] Yeah. Do you want to just say a couple quick words about what you do and where you’re located? You’re out there in a beautiful Denver, Colorado.
[00:03:04] Dr Shaun Kornfeld: Sure. Yeah. Yeah. We have I’m a lead clinician here at Plasticity Centers. We have Two locations, one in Denver, Colorado, which is where I practice. And then we have another one in Orlando, Florida.
[00:03:16] And basically we’re a neurorehabilitation clinic, where we’re specializing in treating individuals with a history of concussions, brain injuries and then also developmental delays and vestibular disorders as well. So that includes things like dizziness and vertigo.
[00:03:32] Dr Mike T Nelson: Awesome. I was just talking to Dr. Matt Antonucci in Florida today by text message. So, yeah.
[00:03:39] Dr Shaun Kornfeld: Yeah, very nice. Yeah he’s my mentor. So, I owe a lot of my knowledge to him.
[00:03:44] Dr Mike T Nelson: Yeah, great guy. And that’s always just fascinating to listen to him and guys like you talk and especially putting it into practice. For someone who may not understand anything we’ve said so far, like how To a layperson who’s not familiar with this field, how would you explain what you do?
[00:04:04] Dr Shaun Kornfeld: Yeah, I explain functional neurology basically as physical therapy for your brain. We basically a medical neurologist will look at the brain’s structure. They’ll identify things like tumors plaquing strokes, things like that. A functional neurologist, or what we do, is we look at the brain’s connections.
[00:04:21] We look at how the brain is communicating with one region compared to the other. And we basically identify deficient connections in the brain, and then we prescribe exercises that stimulate those areas, become, get those areas to become more efficient. And as a result, when those areas become efficient and those pathways are functioning at a normal level, we start to see symptoms decrease.
[00:04:44] So we really work with a lot of injuries that or a lot of conditions that do not show up on MRI or any other type of physical imaging.
[00:04:54] Dr Mike T Nelson: Yeah, I like the relationship to physical therapy because people are probably more familiar with that. So one of the analogies I’ve used, I don’t know if I stole it from you or Matt or Dr.
[00:05:03] Carrick was, in physical therapy, you’re looking for the muscle that’s not really, let’s say, doing its job, whether it’s a gluten meat or whatever. It’s an oversimplified view, but You’re doing the same thing in the brain. You’re looking at these brain areas that, may not be doing the function they’re supposed
[00:05:19] Dr Shaun Kornfeld: to be doing.
[00:05:21] Exactly. So that’s what we’re doing. And with that approach, we’re not only able to treat a lot of conditions and symptoms that don’t show up on imaging, but also a lot of conditions that might not actually have a diagnosis. So somebody where take a kid for example, where they might not have autism or Asperger’s or beyond the spectrum, but they might have some sort of just developmental delay of some sort that might not have necessarily a name or condition.
[00:05:47] This approach allows us to work with those individuals or a concussion, for example, to a lot of individuals who have had a concussion. Their doctors will tell them that their MRI or their CT is normal, go home and rest. And if it’s not better, within 10 days to a month, they start to say, maybe you’re making it up.
[00:06:04] Maybe it’s in your head, maybe. You’re too anxious, right? And this approach really allows us to not only identify that there actually is something wrong, but also clues us in on what therapies are going to be most appropriate to fix that problem, or at least directly significantly improve that problem.
[00:06:23] Dr Mike T Nelson: Yeah, that’s a good point because imaging is super powerful and very useful, but it’s almost more in the biomechanical realm. We’re not at the point yet where we can image your brain and be like, oh, this one part’s not working. You can, do an fMRI and see blood flow. And even that sometimes I know has gotten some flack as being controversial for what’s actually going on.
[00:06:44] And I, I think a lot of times imaging again is useful, but the general perception, the public is that it’s a be all end all that if you don’t see it on imaging, then it doesn’t exist and you’re fine. Just go home. There can’t be anything wrong with you.
[00:07:00] Dr Shaun Kornfeld: Yep. Yeah, exactly. I mean, we see every patient we see basically in the world of concussion, at least, has a normal MRI and imaging is phenomenal.
[00:07:10] I mean, we want patients to get imaging when they have, when they first get a concussion, because we do want to rule out anything more serious. But at that point, I mean, that’s really where we operate is that gray area. They don’t have a a significant life threatening event going on, but they’re also not completely healthy.
[00:07:28] And we operate in between that.
[00:07:31] Dr Mike T Nelson: So obviously you’re going to be using symptoms of what people are reporting, but if you’re not using Imaging. How do you determine what part of the brain is not working
[00:07:40] Dr Shaun Kornfeld: the way that it should? One thing that I really like about our practice in particular is that we’ve invested heavily in different types of diagnostic equipment.
[00:07:49] So, we do a physical exam. It’s about 30 minutes to an hour of us, bedside actually doing different types of, physical tests with the patient. But we do about an hour of diagnostic testing where we have a lot of specialized equipment that allows us to objectify how the brain is functioning and how the brain is working.
[00:08:10] And then we basically have the understanding that certain findings or certain certain tasks that are dysfunctional during those tests can relate to different networks in the brain. So that’s how we’re able to identify that. In terms of our specific technology that we have, the main thing that I really like is we have the VOG, the video oculography, basically are those goggles that allow us to record eye movements.
[00:08:35] And the eyes can tell you so many different things about the brain because every single region of the brain is basically integrated into your eyes, whether it’s keeping your eyes still or allowing your eyes to move. And with these goggles, we’re able to put them on the patient and have them do different tasks on the TV.
[00:08:55] And this is great for a lot of patients because we’re able to record the video of their eyes, which how often is somebody able to see their eyes in action? It’s near impossible because that’s what you use to actually see. And then we’re also able to use graphs. So, even if something might be hard to see with an untrained eye from a patient’s perspective, the graphs are definitely a good way to illustrate what’s going on and then the level of improvement as well.
[00:09:21] We also have a balance plates that allows us to measure balance and sway positions and center of pressures. and stability percentages as well, and then we incorporate cognitive tasking. So between all of those tasks plus the physical exam, we’re able to really paint a good picture of not only how is your brain working, but how is your brain working in your actual day to day life and how is it interacting with the world in real time.
[00:09:46] And that’s one thing that imaging in addition to just focusing on the structural component imaging is a snapshot in time. With the diagnostic test here, we’re actually using real world information to be able to measure brain function while the patient’s actually doing different types of tasks.
[00:10:06] Dr Mike T Nelson: Yeah, one of the analogies I’ve used is that imagine your brain is a safe, and you’re trying to get into your brain by using the combination. And the combination you’re using is a eye function, vestibular function so the balance canals in your inner ear, and then the proprioception, this feedback from where your joints are in space, and if you triangulate all of those, you can find the right coordination of, oh, this part of the brain over here, Because the eyes were doing this, the vestibular system was doing this, the proprioception was doing this, and it allows you to open the safe and figure out with the right combo what part of the brain is not working the way
[00:10:43] Dr Shaun Kornfeld: that it should.
[00:10:44] Yeah, that’s a perfect analogy. I use a similar one with being like everything being a piece to a puzzle. And formulating a picture once you connect everything. So some patients sometimes get really concerned about one exam finding. And I always, need to illustrate the point to them that it’s just one piece of the puzzle, right?
[00:11:03] And we really need to see what the full picture is telling us. So yeah, that, the SAFE analogy is definitely a great one. I might take that one. Yeah I, the I probably stole it from somebody. Yeah, it’s true. I mean, everything is a piece to that combination or a piece to that puzzle to allow us to see the greater picture.
[00:11:22] And not only that, but also allow us to measure the level of improvement too. That’s a huge thing as well, is being able to measure this improvement because sometimes the symptomatic improvement is delayed as you’re provoking the brain with different types of therapies. So to be able to measure that as well is also important to help us determine our treatment plan and to see if we need to tweak along the way too.
[00:11:44] Yeah,
[00:11:44] Dr Mike T Nelson: tell us more about eye function because I’ve worked here in the Twin Cities with Dr. Jeremy Schmo. I’ve gone through, been to his office many times, done his whole one week intensive program. And with the eye thing, it’s pretty cool because For people listening, it’s like this goggles you put over and it’s got a little tiny camera, correct me if I’m wrong here, and you can see the image of your eyes doing different tasks.
[00:12:06] And then the computer can track where your eyes are moving, how fast they’re moving, what direction they’re going. And it was super cool when he did some of the tests and he played back for me what was going on. So, for example, one of the things I have is I don’t see very well in binocular vision. I had lazy eyes or strabismus as a kid, and so, for listeners, you can imagine you’ve got two eyes on your head, and they’re displaced just a little bit.
[00:12:30] And so each image of the eye sends a picture to the back of the brain, and the brain then fuses those images together. Because of eye position, they’re just a little bit off, and it fuses them and allows you to create like 3D vision. In my case, my right eye sits up and out too far, so I have a vertical and a horizontal deviation.
[00:12:49] And when I was a kid, I used to see in double vision. So I went in to, I think I was like four or three for an eye exam, and the eye doctor had this little dog at the end of, the long thing where you’re looking at the eye chart. And he asked me, he’s How many of these do you see? And my parents told me this story later.
[00:13:07] I guess I said two. But only one of them’s real. Because when you see in double vision, you learn, when you interact with your environment, what’s the real image and what’s the false image. Because you can’t obviously interact with a false image. And so the brain and instant wisdom doesn’t like being confused all the time.
[00:13:25] So you can have what’s called visual suppression, where you will just drop one of the images from the eye. So you go from binocular to monocular, so that way you don’t see in double vision. So when I was at Dr. Chameau’s clinic, we did the VNG, the VOG, and when my Eyes were, my head was still, all of a sudden you could see on slow speed, like both my eyes would torque to the right and would come back to neutral.
[00:13:50] Even though my head wasn’t moving, I wasn’t really doing a task at that time at all. And what we figured out was that was an error coming from the vestibular system. Because when you tilt your head, your eyes stay in the middle of your head. So my brain thought that it was an eye issue going on. But it was more of a vestibular issue, because my brain thought that I had tilted my head, so I was trying to turn my eyes to keep them in the middle of my head.
[00:14:17] So ironically, we did a lot of vestibular work over the course of a week. We did the retest that Thursday, and actually that torquing in the eyes went away. So it’s always super fascinating to me about what eye function can tell you. And that just because you see something wonky from the eyes doesn’t necessarily mean that’s the source of the problem, either.
[00:14:39] That just might be a result of what your brain is doing to try to solve some issue.
[00:14:44] Dr Shaun Kornfeld: aNd that’s where I think we work really well with vision therapists and neuro optometrists, because of that connection between your vestibular system and your ocular or your eye system. The connection there is so intimate that, if you’re looking at yourself in the mirror, for example, and you move your head to the right or the left, you’ll see that your eyes will actually move equal and opposite just from you moving your head.
[00:15:07] So there’s a direct connection there between Your vestibular system and your motion system paired with your eyes. One thing I really like, just to touch on one thing with the goggles, Um, they’re infrared cameras, so, which means that you don’t really need any light to be able to see the recording, the video recording.
[00:15:26] Which allows us to see what your eyes are doing in the dark. Which is very difficult to do without those goggles. It’s not impossible, but it’s a lot more difficult. But what’s great is we’re able to put a cover over the goggles so that the patient’s sitting in the dark and therefore the brain has nothing to do to compensate.
[00:15:43] When the brain has abnormal eye movements or when you have abnormal eye movements, you basically, the brain looks for ways to compensate. And one of the main mechanisms that it uses is the ability to fixate on something. So if I’m looking at you, through the computer here, or if I’m looking at a point on the wall or the light switch or whatever it may be.
[00:16:01] That allows my brain to actually suppress some of these abnormal eye movements. So without these goggles it’s very easy to miss some of these abnormal eye movements because the brain’s able to compensate. With the goggles though you’re able to remove the vision or the ability to compensate and you can really see a lot of abnormalities come out when that happens.
[00:16:20] So you might have somebody looking at you Who complains of dizziness, or instability, or double vision, or something like that. And you might be looking at their eyes, with the bedside, and they might look completely normal. But then when you put them in these goggles, you’ll see immediately that their eyes might start to drift, which could explain like a dizziness or a vertigo.
[00:16:41] You might see that their eyes start to converge, which can cause, something like double vision. So it really allows us to tease out some of these things by removing those compensations of the brain. And that’s really an important thing. The brain loves to compensate. It doesn’t want to manifest some symptoms.
[00:16:58] So having some of this equipment and some of these specialized tests allow us to remove those compensations and really tease out. The problem going back to what you said with identifying the root cause of these things. So the goggles is a great tool. I love using them and I use them every day.
[00:17:16] Dr Mike T Nelson: Yeah, I’ve seen a fair amount of videos of just exactly that test, right? You’re just sitting there, okay, everything is dark, like you can’t see anything, right? And so it’s weird even on myself to think, oh, okay, my eyes are perfectly normal. I, there’s nothing, everything is black. And then they show like the video replay and you’re like, Oh, and then he was showing me some video replays for some other people.
[00:17:37] And you see all the craziest shit, like eyes going one way, like anything you can think of, like it’s probably happened at some point, which is, it’s even more interesting when you, in one case, I knew the particular person and like you said if you knew what you’re looking for, you’d see these little things that would show up like here and there, but most of the time, like I function, everything, appeared normal.
[00:18:01] In her case, they did the same testing, put her on the goggles, and her eyes were just doing all sorts of stuff. It was pretty wild to see.
[00:18:10] Dr Shaun Kornfeld: Yeah, it’s true. I mean, I had a patient last month that actually had triple vision. Whoa! How
[00:18:15] Dr Mike T Nelson: does that work? I mean, it doesn’t work so well, but I honestly
[00:18:19] Dr Shaun Kornfeld: don’t know.
[00:18:19] That, that was my first case with triple vision, but by the time we were done with him, within a week and a half he was down to seeing single. One thing that I really found with him, a lot of these findings you want to try to find ways to improve them during your exam, even if it’s temporary.
[00:18:37] If you can find a way to do that, you can try, you can really build on that and try to expand so that it’s more of a permanent solution for them. But one thing that we found with him was that when he had some context behind whatever target he was looking at some contrast rather that triple vision went to single.
[00:18:53] So when he was looking at my thumb, for example, and there was nothing behind the thumb he saw the thumb as triple vision, but when he saw it, in front of my black scrubs and there was a lot of contrast there that went to single. So we utilize that to be able to help him, but that’s something where.
[00:19:11] We were looking at things on the V. O. G. because he also was complaining of things of like dizziness and vertigo. And sure enough, he had a nystagmus where his eyes were drifting. And when your eyes drift, when your head is still, that’s a sensory mismatch to your brain. And that’s really what creates a lot of symptoms, particularly in the vestibular world, is that mismatch between your different sensory systems, in particular your eyes and your
[00:19:34] Dr Mike T Nelson: motion system.
[00:19:35] Yeah, I remember my buddy, Dr. Adam Klotzig, who teaches for the Kerrigan Institute, I’ve known him for a while teaches the pain reset course and other courses, which is a great course. Obviously I’m biased because I work as a faculty member for the Kerrigan Institute, but it is great stuff. I remember him explaining it as that when You have a mismatch.
[00:19:53] You’re basically generating an error in the system, and the brain doesn’t like errors. And what I’ve noticed, just in general with movement stuff, is that it appears that a lot of times those errors can create pain or symptoms. Which, to me, I don’t know what your thought on this is that’s, like an, it’s an action thing that your brain is trying to get you to do something else.
[00:20:16] It’s this and this are not matching up. And so instead of just going about the business, not having any symptoms, having the world be fine, it’s generating this error because the sensory input doesn’t match the world it created. And so it doesn’t know, do I trust the sense? Do I trust the map that I created?
[00:20:33] There’s this mismatch, I can’t solve it. And so you get symptoms or pain, I think, as, uh, in reason to try to get you to do something different, to try to get those things to, to solve so that the error goes away one way or the other.
[00:20:48] Dr Shaun Kornfeld: Spot on. I mean, that’s how I think about everything as well.
[00:20:51] Symptoms are the alarm system of our body, right? We shouldn’t have symptoms. We have symptoms to alert us that something is wrong, right? And that’s why, we can, I’m sure, discuss medication at length and things of that nature. But medication can be great, but it also is something where we’ve gotten into using medication to suppress a lot of these symptoms, right?
[00:21:13] You have a headache every day, try to take ibuprofen or something to get rid of the headache. There’s a reason why you have the headache. And when you look at the brain soul responsibility, The brain is there to process sensory information. The only way that the brain knows what’s going on in the world is through your sensory systems.
[00:21:32] And that’s, the kind of things that we know. Vision, taste, smell, things of that nature. But it’s heavily reliant on vestibular function as well. But also all of those systems working together. So the easiest example would be like reading in the car and getting car sick, right? That happens a lot to people.
[00:21:49] The main reason why is because we have such a sensory mismatch between our vision and our emotions. So when you’re reading something stationary in the car, like a book, your eyes are telling you that everything is staying still, but your vestibular system is telling you that you’re moving right or you’re going over a bump or whatever is.
[00:22:06] whatever it is in the car. And that miscommunication there, creates a lot of nausea for people and, the need to throw up sometimes too. So, so a lot of what we try to do is identify dysfunction in those sensory systems, recalibrate those things, because oftentimes in brain injury in particular they need to be recalibrated.
[00:22:26] So an analogy I use is it’s like recalibrating a scale, except your brain is so complex. You can’t just press a reset button, you need to spend some time doing some therapy. But if we can recalibrate the sensory system, then the brain has accurate information coming in. It generally is able to process that information, at a efficient rate and then the output, it becomes more efficient and the output can be anything from thought to motor control, to emotions, to eye movements to digestion.
[00:22:57] So that’s where we’re really able to see a lot, a myriad of symptoms improve, assuming that the cause of the symptoms originate from the brain.
[00:23:10] Dr Mike T Nelson: wHat are your thoughts? I have this crazy idea about treadmills I’ve had for some time as exercise. On one hand I think, okay, yeah, it’s a good movement, getting walking.
[00:23:19] But on a treadmill, if you’ve ever been in a gym and seen someone do a long treadmill session and watched, this is probably the weird shit I do, but, watched like the first steps they take off the treadmill, it looks like they just got out of the bar and they’re a little bit stumbling around. And I think it’s because there’s a mismatch between You have all this proprioceptive information saying, Hey, we’re walking, we’re moving.
[00:23:40] But your eyeballs are like wait a minute. There’s no things going by where there’s no optic flow. We’re in the same place we were before. But the sensory information from our joints says we’re supposed to be somewhere else. And I think that kind of screws this stuff because walking is such a gate to such an ingrained pattern.
[00:24:01] I don’t see the same thing with rowing or biking or other modalities, but for some reason, walking, I think, because it’s, the treadmill is so similar to the gait pattern that I see some screwy
[00:24:10] Dr Shaun Kornfeld: stuff. Yeah I would agree. I mean, I think the one thing I’m thinking of off the top of my head between a treadmill and a stationary bike is typically with a stationary bike, you’re holding on to handlebars that are stationary.
[00:24:23] That’s providing some more, proprioceptive feedback. I find, and this might just be me, maybe I need to Go through rehab myself, but I find when I’m on a treadmill it’s very hard to know where I am if I’m not every once in a while glancing at my feet to give myself a check. And that’s not how I am when I’m walking or running.
[00:24:42] I mean, I’ve, been an athlete, my entire life playing basketball. But on a treadmill, and maybe it’s because of what you were just talking about, I definitely find, every 5 10 seconds, like I need to look down and make sure that my feet aren’t too close to the, to the front or to the back.
[00:24:59] But I agree. I mean, I think that that is a huge, it’s basically an artificial pattern, right? I mean, it’s not something that we’re supposed to be doing. It’s us, we created the treadmill and now we’re using it. So I do think there’s some level of confusion that goes on, at least when you first start on the treadmill for that session that just reminded me too of a trick that happens sometimes to people as well, where if you’re at a stop.
[00:25:24] Light or like a traffic light stopped and there’s the car next to you and they start like rolling back a little bit Yeah, exactly. You start to feel like you’re moving when you’re not even moving. So It just goes to show how complicated things can be. And, we we think that these injuries can just recover on their own.
[00:25:44] And most of them the brain is able to compensate, but there’s a fair percentage of people out there that their brain just isn’t able to compensate. And because of that, those symptoms just continue to linger. Yeah. One of the
[00:25:58] Dr Mike T Nelson: sort of worst visual vestibular experiences I had was years ago, I was working at Spirit Mountain teaching snowboarding.
[00:26:05] This was back in the early nineties and we weren’t teaching snowboarding. When we didn’t have lessons, they made all the instructors put on this big inflatable bear costume. And it had this big head with this mesh nose. And the mesh nose is right in front of your eyes. And so walking around in it was odd.
[00:26:23] Because the nose was here, the head was this much higher. So I had a duck under doorways and stuff. I scared the crap out of kids because it was a seven foot bear running around. And then my buddies and I had the idea of Oh, we should go snowboarding in the bear costume. And so I’m like, Oh, sure.
[00:26:39] And I’m like, what could go wrong? And I don’t have very good visual stuff. And it was really horrible back then anyway. So I get my snowboard on. The first thing I realized was I can’t see my feet because it’s got this big, belly on it. And I’m like, Oh, whatever. I’ll just go to the bunny hill.
[00:26:56] And I start going and you realize like how much of your motion you rely on your peripheral vision and stuff going by not just your joint information. And plus you’re trying to look out of a three dimensional nose and you can’t really see anything. And it just felt like I was on this horrible snowboard treadmill.
[00:27:14] Because you were never really sure how fast you were going. And you forget that to look at anything you had to keep moving your head around. And the way the bear costume was set up, if you moved your head too fast, the head would spin. And so now you can’t, the nose would be over here, and you could not see anything at all.
[00:27:33] But the analogy I’ve used with people who are not stuck in a bear costume snowboarding, is, so I was at Whistler and it got super, super foggy. And it was so foggy, like you couldn’t see hardly anything. And again, it was horrible because you’re trying to go and it just feels like you’re on this treadmill. And you couldn’t really tell how fast you were going.
[00:27:54] So I use that analogy for people that if you’ve got deficits in your vestibular or visual system, like your senses are either giving you bad information or no information. And it really messes with your perception of the world. So I think people who haven’t had any of those issues and have good normal function, it’s hard to imagine what some of those symptoms might feel
[00:28:19] Dr Shaun Kornfeld: like.
[00:28:21] It definitely is. I find just talking with people outside of the office that don’t have these types of symptoms Everybody can perceive the environment accurately, or so they think, right? So when everybody can do it, it becomes less novel and less special and nobody really talks about it.
[00:28:39] And it’s crazy the amount of people out there who, are generally pretty healthy. They don’t think twice about perceiving the environment or walking into a room and immediately knowing where everything is, or even perceiving something like gravity as being straight up and down. I mean, those are concepts where we talk to our patients, they’ve never even heard of those types of things.
[00:29:02] And once you have something happen to impact that sense or that sensation you immediately understand that nothing else in the world matters. Until that has been recalibrated, because it is the most fundamental system that we have, and if we lose the ability to perceive where we are in relation to everything else that your brain can do or that your body can do just goes to the wayside because of how much of an emergency situation your brain perceives that as.
[00:29:34] And that’s what we find here with our patients, whether they’re coming in for something like dizziness or headaches, Or lack of digestion or double vision. A lot of it relates back to that ability to perceive the environment. And, it’s something that, that not a lot of people really look for.
[00:29:55] So, it often goes missed and when you impact that system, not only do people start to feel better and symptoms start to decrease, but other therapies or other approaches tend to become more effective. So, as a, as an example, I’ve had a number of patients that have been to vestibular therapy or vision therapy.
[00:30:13] prior to seeing us. They haven’t really gotten the results and I love vision therapy. I refer all the time. But after seeing us, they, we refer back to vision therapy and the vision therapists are able to do exactly what they were doing before seeing us and everything becomes more effective. And it just has to do with calibrating those systems and rebuilding the brain in a certain order and hierarchy that mimics how the brain has originally developed, in, in vitro or in utero when when people are first developing in the womb.
[00:30:46] Dr Mike T Nelson: Yeah, I see something very similar. So I do some stuff with them to teach for RPR. So that reflects the performance reset. They have a level one, level two, and I think Hal and Chris are working on a level three. But, so on level two, there’s a way of just testing to basically see are your eyes helping you perceive the world or are they a deterrent?
[00:31:08] So in my case, the first time I did a lot of this work, it’s based on some hands on stuff. And nothing muscular wise is working very well for me. But the second I would close my eyes, everything worked really well. And if you think about it, that’s ass backwards, right? You should be functioning better with eyesight and having your eyes and everything working.
[00:31:32] But my eyes were in essence, giving so many errors to my brain. My brain did better just getting rid of that sentence, just cut it out, it’s just confusing the picture. And then we did some stuff to change that and then everything started working better. So even on a basic level, I’ll see people where we’ll do some stuff and hi, nothing seems to be making any change.
[00:31:54] I’m like, oh, that’s weird. We’ll do some things. We’ll just do some basic functions of checking their eyes. We’ll clear that or make sure that the eyes are actually getting correct information now. And all of a sudden, everything starts, working again. They go back to, their physical therapist or their.
[00:32:09] Whoever the trainer they’re working with, and they literally do the exact same thing they’ve been doing. The physical therapist calls back and eight weeks later, they’re like, Huh, I don’t know what you did, but like all the drills, everything works fine now. And they didn’t do anything. But if you get the system back to the way it was supposed to be designed, now all those other things are much more effective.
[00:32:30] And again, it doesn’t mean those other things or vision therapy or anything is wrong. It just means that, how I think of it, that person wasn’t able to accept that information into their nervous system because they’re just generating so many errors from something else.
[00:32:45] I
[00:32:45] was just saying that when your brain is not getting a bunch of error system, error signals, or error generations, or codes, it’s like rebooting a hard drive that has a bunch of bad sectors on it.
[00:33:00] Once you clear out those sectors, Oh, everything starts working again. So I think sometimes people blame the therapy of, I did this type of physical therapy, or I did this type of vision therapy, or whatever, and, ah, it didn’t work for me. And that may be true, but that doesn’t mean that therapy is bad.
[00:33:16] Dr Shaun Kornfeld: Your physiology and neurology may have been in a state where you just couldn’t accept that information at that time.
[00:33:23] I equate it to learning to run before you crawl or walk, right? Yeah. Sometimes those therapies are would be very effective. If you were ready for that stage in your rehab, right?
[00:33:37] And that’s where I think we have to consider and something that gets often overlooked with the world of brain treatment and brain rehab is you have to consider how These neurological systems are built on top of each other, and it’s like a house of cards where it’s like if the foundation slips away, everything is going to be impacted.
[00:33:57] So when you look at something like physical therapy, I mean, that has a lot to do with gross motor movement. It has a lot to do with strength and stretching and muscle regulation and things like that. How can you have those things work well or at, a 100 percent level when we don’t know where the arm is or we can’t perceive where the arm is in relation to the rest of your body?
[00:34:22] Or how can you decrease neck tightness and, get adjusted or get massage done or acupuncture or something like that? And have that treatment last when your brain still doesn’t be is still not able to recognize where your head is in relation to your shoulders. When those things happen your brain tries to tighten up those muscles or tighten up those neck muscles in particular to send more sensory feedback, but also to protect your head.
[00:34:51] And when you go in there and decouple that and, remove that compensation the brain typically. Still isn’t getting the input that it needs. So it will go right back and regulate that the way that it feels like it has to. So that’s where a lot of what we do in functional neurology, but specifically a plasticity is we incorporate different aspects of those of those fields.
[00:35:14] So we incorporate some aspects of physical therapy, vision therapy, massage therapy vision therapy to but do it in a combination that rebuilds the brain from the ground up, depending on what we see with our testing, some people, let’s just say there’s eight levels to neurological function.
[00:35:33] Some people, the first two levels is looking really good. Other people, the first level doesn’t look good. The third level doesn’t look good, right? So depending on the testing, we will we’ll formulate the treatment plan based off of that. But. Incorporating those things and doing those therapies in combination really allows the brain to relearn what it’s supposed to do in a way that makes sense with day to day life because in real life, you’re not just doing.
[00:35:58] PT types of exercises, you’re not just doing vision exercises you’re doing everything all at once, right? And that’s where I think a lot of people, um, don’t quite understand the brain and how it works. And that’s because we think very linearly. We think if this, then that, then this, then that. With the brain, everything’s ha a lot of things are happening all at once.
[00:36:20] And to compartmentalize brain rehab into eight weeks of this therapy, eight weeks of this therapy, six weeks of this therapy. It works for a lot of people, but there, again, there’s a large percent of the population where we need to rehab in combination with everything just as you would just as your brain would be used to interacting with your environment in day to day outside of the rehab setting as well.
[00:36:46] Dr Mike T Nelson: Yeah, and I think that’s what makes at least the work I’ve seen very different. So for example, in my example, when I was doing the week with Dr. Chemo at his place, I mean, from one day I was doing, riding in the gyro stim, which is this like little machine that’ll spin you around and different things.
[00:37:02] And you’re hitting a target with a laser. So it’s very much vestibular focus to, hitting little lights that are moving, on a screen to some proprioceptive stuff zapping my tongue to get more parasympathetic response. And it was a Kind of a multitude of different things, usually like most day.
[00:37:21] Where I think a lot of times, like you said, therapies and people tend to get very siloed where, I only do vision therapy and I only start with this and then that. If the, again, if that person’s neurology and brain is at a place where they can accept that, then you’re great, but if they’ve got all these other errors that are still firing into the system, like you may have to, work a little bit here, work a little bit there, and then bring these things back together.
[00:37:45] And not just oh, just only stay in, in one area the entire time, which is just a, like you said, a different way of thinking about the problem.
[00:37:55] Dr Shaun Kornfeld: Yeah. Yeah. And another concept to understand as well is summation where not only are you incorporating different, modalities, but maybe you’re using them at the same time too, which which is a abstract type of concept as well with conventional healthcare.
[00:38:11] We might be doing electrical stimulation. As we’re using vibration, as we’re using laser therapy, as we’re having patients look at something, for visual stimulation, the analogy that I use and I like how we both use analogies because it is easier for people to relate to.
[00:38:27] Exactly. It’s a great way for people to understand, complex concepts. But the analogy is when you’re in school. Especially nowadays with all the updated, teaching methods and stuff. They don’t teach you a concept one way and then that’s it. They teach you the concepts verbally.
[00:38:44] They teach it to you visually. They teach it to you through an activity. Then you go home and you reinforce with homework. So, it’s the same concept. When you learn something in school, three, four, five different ways. It just sticks a lot better, and that’s what we see with neurological rehab too, when we are using multiple modalities at the same time, the brain, it’s like we’re provoking the brain, it’s like we’re poking at it, five different ways, we’re going to get its attention at some point, and we’re going to get it a lot quicker than what a lot of our patients are used to.
[00:39:19] And I think a lot of it has to do with doing that combination of modalities, within a short period of time together.
[00:39:25] Dr Mike T Nelson: Yeah. Yeah, the example you gave is great, because I wish I would have known this when I started school, but it took me forever, trial and error to figure out that, okay, if I want to memorize something, I can’t just read it back to myself and expect to be memorized, right?
[00:39:41] So I ended up, it took me years to figure out to, okay, I’d have to write it out, and then later I would start writing it out in different color, and then I would copy part of it. And then I would make little flashcards, and then I would quiz myself in actually different locations at different times, after more sleep or longer periods of time.
[00:40:01] And I had all these things to basically try to get enough overlap into the brain by using as many senses as I possibly could for it to be, semi permanent. Instead, some people can just look at something and go, oh yeah, I remember that. But it seems weird to me that I was never taught that.
[00:40:19] I’m sure there’s somebody probably teaching that. And so I’ve told that to a bunch of students now. They’re like, Oh wow, that works so much better. Because you just need, so my thought was just having more sensory information, having it be similar, but yet different. It’s the same thing if you’re going to learn a motor skill, right?
[00:40:36] So if you think of an elite level athlete, a quarterback in the NFL, like you’re, yeah, you’re throwing a ball. But you’re doing it under these amazing amount of different situations. I remember a good buddy of mine does a lot of coaching for movement and he was working with Aaron Rodgers when he was with the Packers.
[00:40:55] And so he goes through this long lecture about, dynamic systems and how your brain is solving, problems and how you should set up your training and all this stuff. And at the end of the session, Aaron threw this really just weird, like almost like a side, like throw to get around a player.
[00:41:13] And he looked at my buddy who was coaching and he goes, I solved the problem. I was like, Oh, he actually gets it. Because you’re put in a position to do a job, but yet you almost have to impromise and get more practice doing things that are not the same thing that you just. If that makes sense you’re creating the stacking and this overlapping of effects.
[00:41:38] Dr Shaun Kornfeld: Yeah, exactly. And that’s where that concept I think comes in handy and is so important. And oftentimes is the Missing ingredient in people’s rehab. The way that we know that is because we see a lot of our patients where, when we’re going over the different therapies that we have or the different treatments that they’re going to be doing, they’ll make comments like, Oh I’ve already done, some of these things.
[00:42:00] I’ve already done gait stability exercises or I’ve already done the gyro stim before. And We in my experience here and in our field, I know for a fact as well these are all tools and doing them individually could yield very different results when compared to when you do them together.
[00:42:18] So I find patients that have done gait stability exercises before, first off, there’s many different ways to do them. And second off they might not have done them in conjunction with electrical stimulation or in conjunction with the gyro stim. Maybe they use the gyro stim, but they didn’t use. Laser therapy or electrical stimulation.
[00:42:37] So that combination is so important. And I also remember just a funny tidbit, too. Like I remember in college and especially chiropractic school, I forgot who told me that somebody was telling me if you chew gum as you’re studying, and then if you chew gum as you’re taking the test.
[00:42:53] You actually start to remember things better, and I don’t know if that’s entirely true, but I remember that I’ve used that strategy throughout my, times taking tests. Same thing with smells. If you smell, peppermint or something, like they were saying, you can put some on your upper lip, and then you can smell that while you’re studying, and then when you’re taking a test.
[00:43:09] I didn’t do the smell one, but I would always do the chewing gum one. And I don’t have any research behind that, but just anecdotally I seem to have done, with my tests and everything, but that plays into that concept as well as getting different types of stimulation or different modality amounts of stimulation to lead to better brain function, basically.
[00:43:31] Dr Mike T Nelson: Yeah I think there’s some stuff on that what they call state dependent learning. And I believe there’s an old Russian study that used I don’t know if it was actually like amphetamines or some type of stimulant when people were studying and what they found was, and I, this could be just one of those two stories that gets passed down forever because I can’t find the original study and a buddy of mine was telling me, so no, I was originally written in Russian and Adam, so it could be all made up, but that when they tested them, if they practice using the stimulant, Under the test condition, they used the stimulant, they had a good result.
[00:44:04] If they practiced and studied using the stimulant, but were tested not using the stimulant, they did worse and vice versa. So that their, it kind of matches that the state had to match. And so when I read that I even got as nerdy as memorizing some things when I was drinking coffee and then not drinking coffee because I wanted it to not be as a state dependent.
[00:44:27] But if I was really crammed for a test, I would study drinking coffee and then I would make sure I drank coffee before I took the test. Yeah. So same thing.
[00:44:36] Dr Shaun Kornfeld: Yep, anything it takes to pass.
[00:44:37] Dr Mike T Nelson: So yeah, it was at that point I’m like, I’ll do whatever it takes to get out of here.
[00:44:43] Dr Shaun Kornfeld: Yeah, and same thing with what’s called saliency too.
[00:44:47] So just being able to be interested in what you’re doing, right? I mean, that really helps your brain become more plastic or being able to, adapt and learn as well. So that’s another component. That is tough sometimes to do. But something that is important is trying to make the individual going through the rehab as involved, as interested as invested, as they can be to target that that component of saliency basically as well.
[00:45:17] So it’s a little hard with kids sometimes, and then with professional athletes, you always. Constantly have to make things challenging for them as well. But I find too, professional athletes are actually a good group to to use that saliency with because they think that some of these things that they’re doing from the outside looking in, like moving their head, for example, for gaze stability, might be easy.
[00:45:38] But then when they actually do it, they actually realize that they’re getting fatigued or that it’s a little taxing on their system. And that kind of perks them up a little bit and gets them a little bit more excited too. But that’s definitely another, layer to this and you can really start to see how, you can make this stuff simple, but you can get really complex and complicated with the amount of things that you’re the amount of intangibles that you’re integrating into your treatment plan as well.
[00:46:02] Dr Mike T Nelson: Yeah. as We wrap up here, can you give us some examples and just some case studies of people that you’ve, seen and at a high level what you did and what was their results from it?
[00:46:15] Dr Shaun Kornfeld: Sure. Yeah, I can tell you, I mean, I’ll tell you like one like home run type of case. I’ll tell you one that’s a medium and then I’ll, share some other ones as well.
[00:46:24] But like a home run case that we had is we’ve had, we had this woman come in young woman, early 20s from Canada and basically she had a concussion. I think she was snowmobiling and fell and hit her head. And basically dark room, sunglasses, for a few months, maybe four or five months.
[00:46:44] Couldn’t really do anything, felt dissociated, so she didn’t really feel connected to her body and things of that nature. Basically went through the exam, found a lot of the things that we were talking about that sensory mismatch between vision and vestibular not perceiving gravity appropriately, so her subjective visual vertical was off, and we really recalibrated those sensory systems, and it’s great.
[00:47:05] I mean, we, I talk about her all the time because she went from feeling like the worst ever to feeling very good. And almost like a good restart on life. Came in wearing sunglasses, left without sunglasses. Some things that we were able to measure with her balance, for example, that’s really cool, is like her stability increased by about 130 percent in five days.
[00:47:28] I mean, it was great. She and seeing that, just psychologically restored so much hope for her as well. So that was one case where, you know, what we did with her was we basically incorporated vestibular rehab. Proprioceptive therapy. So we used a lot of electrical stimulation can target the vestibular function as well.
[00:47:48] So once it hits the central nervous system the vestibular nuclei actually get signals from proprioceptive input too. We’re able to do that. We did laser therapy to help her with. fatigue and brain fog and things of that nature. So that was a really good case. One case that I just got an email from this guy yesterday, actually awesome guy basically had a head injury as well.
[00:48:11] He was a case where we went through everything and like you were saying, sometimes therapies are effective and it’s just not the right time or something like that. We went through all of his therapies and or I’m sorry, all of his evaluations and therapies. Basically we found some similar things.
[00:48:27] He was very light sensitive, a lot of fatigue to the point where he couldn’t work. And what we found was his brain was just working. Extra hard in overdrive, basically, and that’s because of that calibration that needed to take place. So anyway, we ended up recalibrating everything, we retested, his tests improved, but he didn’t really notice much symptomatic improvement.
[00:48:49] When we see a case like that, one of two things typically, either one, this is a neurological issue and that was the case not the case for him, but there was another component outside of the neurological rehab for him or number two there’s something else going on. I mean, it could be genetic.
[00:49:05] Something along those lines. So for him, what we saw was his brain was operating more efficiently, but his fatigue was still there, so I referred him over to functional medicine and I just got an email from him yesterday just by changing his diet and then having his brain work more efficiently with that rehab that we were doing.
[00:49:24] His that was the secret ingredient right there, the secret recipe, those two, approaches. And now he’s like a whole new person and he’s back to almost pre injury type of status. So that was great to see. And then another very interesting case that I see, and I think that this is relevant because I just read a report that with long COVID and everything coming out.
[00:49:44] We’re seeing a higher instance or a higher incidence of functional neurological disorder. I had a kid with FND in a couple months ago, he wasn’t able to move the right side of his body, his right arm and right leg. And he came in with his mom, having to. basically carry him. And by day three by Wednesday, he was walking out.
[00:50:06] And that was really cool. Basically for that, the approach that we used was there was no physical reason for him to not be able to move. We had to show him and allow him to prove to himself that he was able to move. So I did a lot of things with him watching himself in the mirror.
[00:50:22] Where I had him raise his arm a little bit and when he wasn’t able to raise it more, I would boost it up with my own hand and then have him hold it there. And I would just talk to him in certain ways where I would say, okay, if you’re able to hold your hand up higher like you are right now, why can’t you just move it there because you’re using your muscles to hold it up?
[00:50:41] And that type of approach, works for him to show him that he is able to do it. That approach doesn’t work for everybody with FND, but for him it worked in particular. So, so those are some cases, our bread and butter is really concussion. The last one I have is another guy who had a concussion as well.
[00:50:59] He had, he was coming in for balance issues and coming in for headaches. Which not a lot of people may think is correlated, but a lot of the times it is when you look at the different regions of the brain or networks of the brain that are involved. And for him he actually holds our record now for the highest level of, Improvement that we’ve seen in the balance testing and basically what we realized with him was that his brain wasn’t perceiving his feet Appropriately.
[00:51:30] He wasn’t getting good sensory feedback part to balance when you can’t you know, Yeah, so we did a lot of electrical stimulation with his feet We did a lot of vibration modalities as well we incorporated the gyro stim too, but his balance improve significantly. And when you have better muscle regulation and you know where you are in the environment more appropriately, there’s no reason to tighten your neck as much.
[00:51:57] And when you don’t tighten your neck as much, you typically don’t get those pain referral patterns around your head that we interpret as a headache. So his headache went away by the time we did the final exam. It was the first time in three months that he hasn’t had a headache. So, oh wow, that was really great to see too.
[00:52:13] So, definitely a lot of interesting cases, not all cases go the way that we want them to go. But an overwhelming majority do, and when they don’t, it typically means that there’s just another piece to that puzzle, right? And oftentimes it’s, I find that it’s the metabolic approach, so more like functional medicine.
[00:52:33] Sometimes there’s a psychological component to, patients. are operating better, but they’re nervous to get back out there. So they almost cling on to their symptoms a little bit. But a lot of people end up feeling a lot better, which, makes me want to get up and come in every day as well.
[00:52:49] Dr Mike T Nelson: Yeah. Yeah. That’s awesome. And last part on the concussion part that. This is, I think, sometimes both acute or people, I’ve noticed, who’ve had concussions many years ago who are still having symptoms, correct? So it’s not always just, I got a concussion last week.
[00:53:08] Dr Shaun Kornfeld: Yes, and I’m glad you brought that up.
[00:53:10] One thing that’s really erupt me over the years now is we’ve had a number of a lot of patients that have come in that have had symptoms three years, five years, 15 years, 20 years post injury. And, they’ll still be having symptoms, but a lot of the times they’ll tell me that they were told that if they’re not feeling better within 18 months, they’re not going to get any better.
[00:53:36] They’ve been told that they need to get better by, June or else they’re not going to see any more progress. We’re just not seeing that, I don’t know why patients are being told that, but that is just the exact opposite of what we see. Oftentimes for us, we’re tertiary care. We’re private pay patients don’t get injured and then five days later come in to see us.
[00:53:59] They try to go the insurance route. They try to rest. They try to do things on their own. So because of that, we do see a lot of patients that have had symptoms for years, if not decades. And what we find is the brain is just as able to adapt. Whether you got your injury five days ago or five years ago, and not only that, but sometimes we see patients that actually improve quicker that have been post injury a lot longer compared to, other people.
[00:54:26] So as an example, like sometimes we’ll see people that have had an injury, 10 years ago, they might need. 10 treatment sessions, and then they feel pretty good. Whereas somebody who got injured maybe a month ago, you may think, Oh, okay. A month, they might need less treatment. We’ve had cases where they’ve been injured for a month and they actually need, 15 or 20 treatments before they’re back to, normal.
[00:54:52] So I think time is a factor for a lot of people, but I don’t think it, it excludes anybody from being able to recover and end up feeling better.
[00:55:02] Dr Mike T Nelson: Yeah, I mean lost track of how many people I’ve referred to you guys.
[00:55:06] Maybe something else is going on either way you’re going to be, encourage people to find somebody and just get it checked out. Yeah, I think that’s a great point. I know something that we try to do secondarily is act as almost like a resource navigator for our patients.
[00:55:18] Dr Shaun Kornfeld: I’m, heavily networking and in my local community here, so I know. P. T. Psychiatrist, psychologist vision therapist, so if we’re not the right answer, or maybe we like I’ve been using that analogy, maybe we’re just a piece to that puzzle, right? Maybe we’re a large piece. Maybe we’re a small piece, but that’s something where, depending on what we find, if we can link it or correlate it to your symptoms.
[00:55:42] Then it’s okay let’s get going and let’s do some treatment. But if it’s something that we can’t correlate or maybe, all the tests come back normal, we can help you, try to find the right provider for you. And like you said, you just check it off the list because there is no right answer when it comes to the brain.
[00:55:58] And that’s where I think The healthcare community, we need to accept that because I think right now, a lot of our research specifically with medication and things like that, we’re looking for a one size fits all type of thing. I think the brain is too complex to have something like that.
[00:56:16] And the other thing I’ll comment on too is, you were talking about people with symptoms. We’re very reactive as a society with our healthcare. When you switch into that proactive realm, I think it’s important to understand. Just because you don’t have symptoms doesn’t mean that your brain is not working, or it doesn’t mean that your brain is working the way that it’s supposed to be working.
[00:56:37] There’s so many compensations and adaptations that occur in the brain, and what I find is people, when we talk about things like CTE and stuff like that, sometimes a lot of people have had a history of head injuries, but they don’t, they think that everything’s okay because they don’t have symptoms.
[00:56:52] But later in life, when the brain loses the ability to compensate, you start to see symptoms come return, you start to see early onset types of conditions, right? Not necessarily dementia, but just things like balance problems, even something like that, right? And in a world where, as you get older, you want to remain independent and maintain your independence.
[00:57:14] I would say it’s equally as important to get, an annual physical or something for your brain or like a brain baseline for your brain every single year. It’s crazy how we perceive everything because we get annual physicals for our blood, for our urine, for our body, for our ears, our eyes, things like that, but we don’t get it for our brain.
[00:57:34] And it, when you consider that’s the only thing in our body that we can’t really replace. You start to question, like, why is it set up that way where everybody doesn’t make that a priority? So, when you’re symptomatic, for sure, it’s important to get these things checked out, but even when you’re not symptomatic, I would add it into your annual, routine of of types of physicals that you get every year.
[00:58:00] Dr Mike T Nelson: Yeah, I would 100 percent agree with that, and I’ve referred quite a few people who didn’t even really have a history of concussion, didn’t really have symptoms per se. buT sometimes I’ll look at like their heart rate variability, which is a marker of stress on their nervous system and their resting heart rate.
[00:58:18] And if like, all their stressors are good and their HRV is on the low side, but their resting heart rate is very low, I’m like, Eh, that’s funky, right? It should be, your HRV should be higher as your resting heart rate goes down. Or if they report, being more tired, or they get good sleep, but they’re sleeping.
[00:58:38] 10 hours every night and nutrition’s good. Everything else is good. Like sometimes you just get this feeling that there’s something off here that doesn’t make sense and not all the time, but i’d say half the time they come back and they’re like, oh, yeah, we found this vestibular thing We found this funky eye thing and they get it corrected or therapy with it and then they’re all good to go again.
[00:58:59] Dr Shaun Kornfeld: So yeah, I would agree with that yeah, the way that I look at it is When you’re in the weeds and you’re going through this stuff, whether it’s recovery or having symptoms or whatever it may be, everything’s a drag, right? It’s man, I gotta go to this other doctor.
[00:59:14] I gotta go to this other doctor. Yeah, everything feels hard, too. When you’re on the other side of it, though, it’s like everything becomes worth right away, right? And all the stress that you had just dissolved. So, for us, it’s hard to convey that message. When a patient calls us, they’re in need, right?
[00:59:30] And they’re almost desperate and they don’t know where to turn and things like that we’re we know what it’s like to be on the other side. So we’re trying to take them to that other side. And it might be, dragging them to that other side figuratively, right? Because, they’re, they don’t trust that what we do is effective because they’ve been to so many doctors before.
[00:59:50] Why would we be the ones to help them? Like that type of thing and it, that’s the challenge that we try to overcome with our prospective patients is we know where we are going to get to, statistically with most of our patients. And I know it’s just another doctor to go to. It’s another thing to try.
[01:00:08] But when you get to that other side, it’s all worth it. I mean, it’s just like anything else, right? It’s like dieting sucks. But when you start to lose weight or when you become healthy. And when you look in the mirror it’s worth not getting the McDonald’s, McDouble or something like that, right?
[01:00:24] So, yeah it’s just like anything else. It’s you gotta put in the effort. And I get that it’s a leap of faith sometimes for people who have been to these number of doctors, 10, 20 doctors. I saw somebody who’s been to 40. Oh! Across the country. And that patient’s dad is a doctor themselves.
[01:00:43] And, so they have an in with all these other doctors. And even so they had to, they were to 40. And so, I get that it’s hard to do sometimes, but when you do get to that other side, we see our patients, who start to feel better and, all the money that they spend, all the time that they spend, all the worrying they spend, it dissolves once you get to that finish line.
[01:01:05] Dr Mike T Nelson: Yeah, awesome. Thank you so much for all your time. I really appreciate it and where can people find out more about you? I know you’re located in Denver, Colorado, but you work with people from all over the U. S., Canada, all over the world, actually. Yeah, we work from, with patients from all over the world.
[01:01:22] And for us, the easiest thing is to check out our website. It’s plasticitycenters. com. And I’ll spell that because not everybody knows how to do it. It’s P L A S T I C I T Y centers dot com. And basically that will have all the information. We have patient care specialists that you’ll be able to call and will educate you on what we do and how we would be able to help.
[01:01:47] We also have complimentary consults with our doctors as well. Anything that we can do to make people feel more comfortable with the decision, to seek this out as a treatment for them. And then yeah, like you said, Denver, Colorado, and then Orlando, Florida, depending on your geographical location.
[01:02:04] We would route you to the nearest center, basically.
[01:02:08] Dr Shaun Kornfeld: Yeah, that’s awesome.
[01:02:09] Dr Mike T Nelson: And I know I’ve had people we’ve personally referred to you. I know my buddy Matt’s worked on several people and it’s always been a good experience. Like you said there’s work involved. It can be a hassle. And sometimes you’re doing stuff multiple times per day for a week or longer.
[01:02:23] You’re doing your homework, but so far everyone has been very positive with the result. And I know even just the stuff I’ve done here with Dr. Jeremy Schmoe has been extremely helpful. So I would encourage people to. At least take the next step and check it out, especially if you’ve done a lot of other stuff that hasn’t worked.
[01:02:40] I think it’d be well worth your time. Again, I’m associated with the Carrick Institute, but I don’t make any money other than other disclosures or referrals or anything like that, so. Cool. Thank you again for your time. I really appreciate it. And we’ll put all the links for that and everything in the show notes here for people.
[01:02:56] So thank you so much. Really appreciate it.
[01:02:58] Dr Shaun Kornfeld: Yeah. Thank you so much for having me on. I really appreciate it. And if anybody wants to reach out to me personally, my email is skornfeld@plasticity.Co. We can put those in the show notes too, probably, because my name is a hassle to spell, so. I definitely appreciate you having me on, and appreciate you trusting us with people as well, and definitely looking forward to collaborating in the future.
[01:03:19] Yeah, awesome! Thank you so much!
[01:03:21] [01:03:22] [01:03:22] Dr Mike T Nelson: Thank you very much for listening to the podcast. Huge thanks to Dr. Sean for coming on the podcast. Explaining all about the great work that he does there.
[01:03:33] And as I said at the beginning of the show, we’ll put links, you can check out his clinic. I’ll put a link for my buddy Dr. Jeremy Schmoe in Minnesota. And I’ll also put a link for my buddy Dr. Matt, who also runs the Centers for Plasticity down in Florida. Again, it’s not limited to those areas only.
[01:03:51] We’ll link to the Carrick Institute, and you can find hopefully a functional neurologist in more and more locations. Now, if there’s anything you, that I can do to help out you can find a way to get a hold of me and thank you so much for listening to this podcast. Really appreciate it. If you want more cutting edge information on performance and body composition and health go to the website, miketnelson.com/podcast You can see all the podcast episodes I’ve been on before, all the current episodes, and also get on to the daily newsletter. Just scroll down below, and you’ll get all the cutting edge information delivered directly to your inbox, hopefully in a way that is semi entertaining also.
[01:04:36] Thank you so much for listening, and bearing with all the audio issues we tried to stitch together here, greatly appreciate it, talk to all of you next week.
[01:04:45] You know something? That was a sweet number. It sure was. You know something else? What? I hate sweet numbers!
[01:04:52] Nancy: This podcast is for informational purposes only. The podcast is not intended as a substitute for professional medical advice, diagnosis, or treatment. You should not use the information on the podcast for diagnosing or treating a health problem or disease or prescribing any medication or other treatment.
[01:05:08] Always seek the advice of your physician or other qualified health provider before taking any medication or nutritional, supplement, and with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have heard on this or any other podcast.
[01:05:24] Reliance on the podcast is solely at your own risk. Information provided on the podcast does not create a doctor-patient relationship between you and any of the health professionals affiliated with our podcast. Information and statements regarding dietary supplements are not intended to diagnose, treat, cure, or prevent any disease.
[01:05:41] Opinions of guests are their own, and this podcast does not endorse or accept responsibility for statements made by guests. This podcast does not make any representations or warranties about guest qualifications or credibility. Individuals on this podcast may have a direct or indirect financial interest in products or services referred to therein.
[01:05:59] If you think you have a medical problem, consult a licensed physician.







Leave A Comment