Every quarter when I teach Exercise Physiology, I issue a challenge to my students to see if they can find a peer reviewed study asserting that in healthy people, too much protein will damage their kidneys.
Can you guess what they find?
Nothing, nada, zilch, zip. The data does not currently exist.
Then how did this myth get started?
Part of the reason for this myth is that eating more protein will increase the amount of work done by your kidneys. Markers such as creatinine and GFR (glomerular filtration rate) may go up indicating that your kidneys are working harder. But do actual damage markers (such as urine microalbumin) change?
Let’s dive in.
Here is a quote to kick it off.
From Phillips, SM 2014:
“.., an examination of the statements made by both the Institute of Medicine in setting the protein RDA in North America [1], as well as the World Health Organization’s (WHO) report on protein intakes [2], indicates there is no evidence linking a higher protein diet to renal disease.”
According to two top agencies, the risk on our kidneys in healthy subjects appears to be slim. This myth is not looking good.
“Prolonged intake of a large amount of protein has been associated with potential dangers, such as bone mineral loss and kidney damage.
In otherwise healthy individuals, there is little evidence that high protein intake is dangerous. However, kidney damage may be an issue for individuals with already existing kidney dysfunction” (Tipton KD, 2011).
So far, it appears that having your kidneys do more work by itself is not a bad thing.
When you go to the gym to do the “sun’s-out-guns-out” session, your biceps do more in the hopes (fingers crossed) that they get bigger (hypertrophy).
Could the same thing happen with your kidneys?
“… an increase in protein from 91 to 108 g/d increased kidney volume by 9.1 cm3 and GFR by 5.2 mL/min, without any change in microalbuminuria…” – Bie P & Astrup A, 2015
In English?
Increasing protein did put the kidneys under more work (as shown by an uptick in GFR); however, it did not do any damage to them (no increase in microalbuminuria). The kidneys, just like your biceps, did get bigger, but that was not from any damage. They were just adapting to the stress placed on them.
The current data does not support these assertions that protein is dangerous, but what if you are a hard training bro and consume a metric piss ton of protein.
Show Me The Bros Studies
I get it. You lift weights. You therefore are a special snowflake; thus, need studies done on your snowflake friends. I gotcha. Ask and you shall receive.
One of first studies on this was from Poortmans JR and Dellalieux O in 2000. At the time (and even now) it was suggested that excess protein would be hazardous to the kidneys.
This study investigated body-builders (yeah, bro!) and other well-trained athletes with high and medium protein intake. They did their research work and took samples including urine collection, more general geekery in the name of science and such. What they found was that while the high protein seekers did have higher plasma concentrations of uric acid and calcium, the bodybuilders had normal renal clearances of creatinine and urea (waste products). Scientists concluded that protein intake under 2.8 g/kg did NOT impair renal function in well-trained athletes.
Score 1 for the bros and their protein consuming mad wheys. (Get it- funny joke I make).
Another study was done by Brandle and colleagues in 1996.
While the study was not “perfect,” it was the first to look at the effects of protein on kidney function. They found no correlation between albumin excretion rate (urinary albumin arguably being a damage variable) and gross protein intake (as assessed by nitrogen excretion rate).
These two studies are summarized below in a nice table by Lowery, LM and Devia L. (2009) for the super nerd herders.
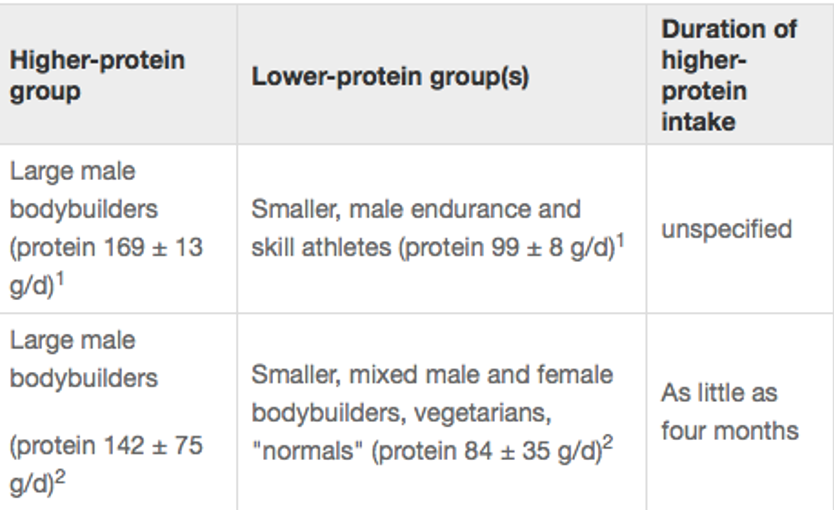
Study Summaries
1. Relative protein intake 1.94 ± 0.13 g/kg daily (Higher group) vs. 1.35 ± 0.12 g/kg daily (Lower group) 2. Relative protein intake 1.65 ± 0.87 g/kg daily (Higher group) vs. 1.41 ± g/kg daily (Lower group) 3. Exercise not specified but catabolic events were controlled.
The Dozen Dude Brah Study
In a recent study done by Dr. Jose Antonio and colleagues (2016), they took it to the extreme by looking at heavy benching dude brahs on lots and lots –o-bro-tein.
They used all the great uber geek words like “a randomized, crossover design, resistance-trained male subjects.” Yep, these dudes lifted and ate copious protein. The average bench press at baseline was 126.4 kg (which is 278 lbs for those who think the metric system was invented just to torture you). That is not elite standards, but for most studies that is up there.
For eight weeks, participants scarfed down a high protein diet at over g/kg/day –which for a 220 lbs. person (100 kg) is 300 grams of protein per day. And they coupled it with a periodized heavy resistance training program. During the other 8 week period, they consumed their normal (lower protein) diet.
What did they find?
Even though the high protein time they were eating more calories as protein, there were no significant changes in body composition (i.e. they did not get fat) or markers of health in either group (i.e., blood lipids, glucose, renal, kidney function etc.). You read that correctly. Despite hoovering up massive amounts of protein, their kidneys did not launch an attack to exit their low back due to the high protein intake.
To further back up their point, researchers did a cool subanalysis on 2 subjects who ate the most protein. They did not find any renal (kidney) issues despite them consuming 483-724% OVER the RDA for protein.
I Need More . . .
Ok, so you are still not convinced despite all my super advanced pubmed ninja-ing all over your pectorals-es (that is the plural form, right?).
You could argue (and rightfully so) that this data is still short term. Most people are eating high protein for months to years to decades. What about 6 months into their high protein eating plan? Maybe their kidneys are starting to get tired and want to take the big dirt nap?
Ok, I got ya, bro…
Dr. Jose Antonio again with his super nerd friends in 2016 published a one year study.
Yep. Put that in your shaker cup, and drink it.
In terms of science, that is an eternity.
They took fourteen healthy resistance-trained men who had been training and average of almost 9 years for a randomized crossover design study. They had them consumed their normal diet altered with a high protein version (>3 g/kg/d) so that on average, each subject was on each version for 6 months each. They found that in those who consumed a high protein diet (about 2.5-3.3 g/kg/d) for one year, there were no harmful effects on measures of blood lipids as well as liver and kidney function.
And similar to their previous study, despite the total increase in energy intake during the high protein phase, subjects did not experience an increase in fat mass.
Yep, tons of protein for 1 year in high level trainers with free living humans. For science, it does not get much better than that for data.
Out of all the things you could do to improve your health, performance, and body composition, worrying about too much protein is waaaaaaaaaaay down on the list.
Most people I work with do much better by increasing their protein intake.
Now this does not give you free reign to consume 400 + grams of protein every day for months to years on end to prove some lab coat nerd wrong. At some point it would be bad. Too much is too much…. Too much freaking water can kill you too (REF – LD50 water).
The data that protein is harmful to your kidneys is just not there. Sit back, relax, have a protein shake, and your kidneys will be just fine.
Pass me the protein,
Dr Mike
References
Proc Nutr Soc. 2011 Mar 7:1-10. [Epub ahead of print]
Efficacy and consequences of very-high-protein diets for athletes and exercisers.
Tipton KD.
“Stuart M. Phillips. A Brief Review of Higher Dietary Protein Diets in Weight Loss: A Focus on Athletes Sports Med. 2014; 44(Suppl 2): 149–153. Published online 2014 Oct 30. doi: 10.1007/s40279-014-0254-y”
Bie P, Astrup A. Dietary protein and kidney function: when higher glomerular filtration rate is desirable. Am J Clin Nutr. 2015 Jul;102(1):3-4. doi: 10.3945/ajcn.115.112672. Epub 2015 Jun 10.
Poortmans JR, Dellalieux O Do regular high protein diets have potential health risks on kidney function in athletes? Int J Sport Nutr Exerc Metab. 2000 Mar;10(1):28-38
Brändle E, Sieberth HG, Hautmann RE. Effect of chronic dietary protein intake on the renal function in healthy subjects. Eur J Clin Nutr. 1996 Nov;50(11):734-40.
Lowery LM, Devia L. Dietary protein safety and resistance exercise: what do we really know? J Int Soc Sports Nutr. 2009 Jan 12;6:3. doi: 10.1186/1550-2783-6-3.
Antonio J, Ellerbroek A, Silver T, Vargas L, Tamayo A, Buehn R, Peacock CA. A High Protein Diet Has No Harmful Effects: A One-Year Crossover Study in Resistance-Trained Males. J Nutr Metab. 2016;2016:9104792. Epub 2016 Oct 11.
Antonio J, Ellerbroek A, Silver T, Vargas L, Peacock C. The effects of a high protein diet on indices of health and body composition–a crossover trial in resistance-trained men. J Int Soc Sports Nutr. 2016 Jan 16;13:3. doi: 10.1186/s12970-016-0114-2. eCollection 2016.

Leave A Comment