Welcome back to the Flex Diet Podcast! I’m Dr. Mike T. Nelson, and in this episode, I sit down with Dr. Hamel Patel, Chief Scientific Advisor to Discovery and the brilliant mind behind the ME screen blood test for mitochondrial function.
We dive into Dr. Patel’s fascinating journey into the world of mitochondrial research, how mitochondria impact everything from metabolism to resilience, and why he developed a personalized blood test to better understand mitochondrial health. We also get into some really cool topics like how heat and cold exposure affect your mitochondria, the intersection of meditation and cellular health, and even the emerging role psychedelics might play in this space.
Dr. Patel also shares his top tips for optimizing mitochondrial function and explains the science behind this cutting-edge testing method. If you’re curious about performance, longevity, or just want to geek out on mitochondria with two scientists, this episode is for you. Let’s dig in.
- Tecton Life Ketone drink! https://tectonlife.com. Use code DRMIKE to save 20%
- LMNT electrolyte drink mix: miketnelsonlmnt.com
- Daily Fitness Insider Newsletter: Sign-up here
- Flex4: Dr. Patel’s top 4 recommendations to improve mitochondria
Available now:
- Grab a copy of the Triphasic Training II book I co-wrote with Cal Deitz here.
Episode Chapters:
-
05:51 Dr. Patel’s Journey into Mitochondrial Research
- 08:34 Heat and Cold Stress in Mitochondrial Function
- 12:18 Mitochondrial Function and Health
- 19:50 Innovative Mitochondrial Testing
- 31:05 Understanding Mitochondrial Respiration
- 31:20 Testing Mitochondrial Efficiency
- 31:51 Energy Production Pathways
- 32:24 Free Radical Generation and Stress Testing
- 32:58 Exercise Physiology and Mitochondria
- 33:50 Personalized Mitochondrial Health Recommendations
- 33:59 The Complexity of Mitochondrial Adaptation
- 37:28 The Role of Membranes in Mitochondrial Health
- 38:49 Oxygen’s Dual Role in Life and Aging
- 41:05 Preconditioning and Cardiovascular Health
- 43:07 Hypoxic Training and Breath Work
- 43:50 Meditation and Mitochondrial Function
- 48:03 Psychedelics and Mitochondrial Changes
- 54:33 Practical Tips for Mitochondrial Health
- 56:12 Conclusion and Final Thoughts
Flex Diet Podcast Episodes You May Enjoy:
-
Episode 164: How to use diagnostic testing to improve your metabolic health: An Interview with Sam Miller
- Episode 190: Let’s Get Woo Woo – From Physics To Scientific Testing To Exercise Performance with Ian Mitchell of Wizard Sciences
Connect with Dr. Patel:
- Website: mescreen.com
- Enter code DRMIKE to save $100 – I don’t make a dime off it. I would love to hear what you find, so hit me up if you try it!
- Instagram: @hamalpatelphd
Get In Touch with Dr Mike:
Rock on!

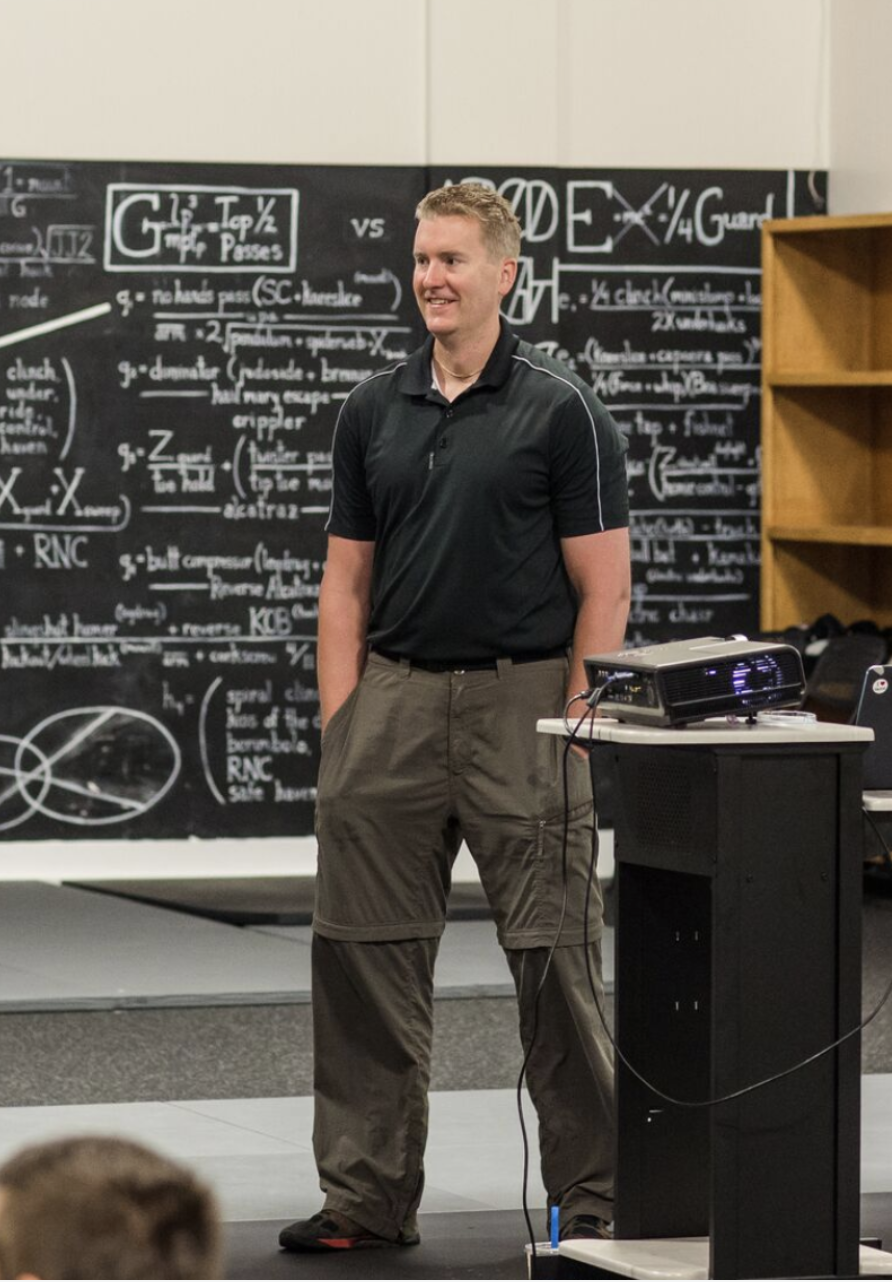
Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
Dr Mike T Nelson: [00:00:00] Welcome back to the Flex Diet Podcast. I’m your host, Dr. Mike Nelson. On this podcast, we talk about all things to increase performance, improve body composition, do all of it without destroying your health within a flexible framework. Today on the podcast, we’ve got a very cool one here with Dr. Hamal Patel.
He is a Chief scientific advisor to discovery and they’re the creators of the ME screen blood test to look at mitochondrial function. He’s also a tenure professor and vice chair for research, the Department of Anesthesiology at the University of California, San Diego. He is done a lot of really interesting research that we talk about here, looking at different types of physiology, metabolism, and even.
Some cardiac ischemia, reperfusion [00:01:00] injury models. And in this podcast we talk about what got him into researching mitochondria exploring some heat and cold stress what do actually the mitochondria do. And then we talk about the test that he’s developed which is a blood test to look at all the different aspects of mitochondrial function.
There will be some ways you can personalize these recommendations, the role of oxygen, and then we even got into the discussion about metabolic effects, meditation, and even potentially the effects of psychedelics such as ayahuasca on mitochondrial function. And if you want his top four tips for mitochondrial function, you can find that at the flex four.
So go to the link down below, put your name in there and your email, [00:02:00] and we will send it to you directly. You’ll also go onto the Daily Insider newsletter list. At the same time, if you’re already on my insider newsletter list that I send most of my content too you will get that sent to you directly.
So if you want the top four tips from Dr. Patel about mitochondrial function and what you can do in about. Four minutes. Go to that link, put your email in there and we’ll send it to you directly. Also wanted to say that he was kind enough to have a discount code for the ME screen, which you can find at me screen, S-C-R-E-E n.com.
We’ll put a link down below. You can use the code Dr. Mike at checkout, and you will save a hundred dollars on that. In my case, this is not an affiliate link, so I don’t make a single dime off of it. But wanted to encourage you to do it and if you [00:03:00] would be open to sharing your results of what you find, I think that would be really fascinating.
So this is very new technology. He talks about how this has been vetted through NASA and through actual research. But with all new things, I’m interested to see how do people use it? What changes can they make, and what do they find for their results? So if you’re open to sharing them I would love to see what you find show sponsors.
We’ve got ketones from Teton. You’re looking for ketone EERs to get an a state of ketosis, then a very short period of time. Check them out below. I’ve been using them a fair amount. Some down here in South Padre height boarding still. And then we also have another thing I’ve been using a lot down here, our friends over at Element electrolytes.
So you can go to the link down below, get my favorite electrolytes from Element also. And without further ado, here is the podcast with Dr. Patel [00:04:00] all about mitochondrial function and how to test for it. Thank you so much for listening to the podcast. Really appreciate it. Huge thanks to Dr. Patel for being on the podcast, sharing with us all the wonderful new testing and just all the amazing research that he is doing really fascinating stuff.
So make sure to check out the me screen.com for mitochondrial efficiency test, all the other research and everything else that he’s got going on. Use the code Dr. Mike at checkout. If you purchase the me screen test it is not an affiliate link. I don’t make any money off of it. I wanted to give you guys the biggest discount I could arrange, even if I don’t make any money off it.
So I’m super curious to see how this works, how people use it, what are their results, and as you mentioned in the podcast. Having a solid test for mitochondrial function I think is something that is extremely useful. [00:05:00] And hopefully with more testing just based on a simple blood draw, we’ll have more information that allows everyone to make better decisions about their health and performance.
Also, check out, we mentioned ketones. We’ve got Teton for ketones, we’ve got element for. Electrolytes. So I’ve been using both down here in South Padre, Texas. So thank you so much for listening. I really appreciate it. And if you want Dr. Patel’s top four things to improve your mitochondrial health go to the flux four down below, put your email address in and we will send it directly to you and also puts you on the exclusive newsletter Insider.
A list too.
Welcome to the podcast, Dr. Patel. How are you? Good. Good to see you. Yes. Very nice to see you. Thank you for doing this.
I really appreciate it. Yep. For your research, like how did you get interested in I. Mitochondria. We’ll talk about, you’ve got a test for mitochondria and, but [00:06:00] I’m always curious like what kind of got you into that area?
Dr Patel: Yeah, so I’ve been doing mitochondria work since graduate school days.
So the project that I focused on for my PhD thesis was looking at how you can protect. The heart from an ischemic event. So from having a heart attack, how do you protect that from dying during that injury? And one of the things that the lab I was working in that discovered is that opioids have this magical protective effect that’s very reminiscent of preconditioning this, endogenous that the heart.
And every other organ has that. If you subject it to a small stressor and you give it a big stressor a little bit after it adapts to that. And the way the heart adapts, which is a highly energy consuming organ, is it has to preserve its mitochondria in a unique way. And so we started thinking about mitochondria.
Oh, I guess that’s what, 25 years ago from that perspective,
Dr Mike T Nelson: You were in before it got sexy.
Dr Patel: I [00:07:00] know. Yeah, we were in for a long time. And then I did that in, at the Medical College of Wisconsin in Milwaukee. I moved to San Diego to UCSD in 2002, and I started working on cell stress systems.
So basically looking at how different pathologies are tied to. Membrane biology, and we hit upon this idea that it really is the membrane’s regulation of mitochondria and internal structures. That creates disease and resiliency against disease. And so we started looking at this unique relationship and so we’ve then expanded to creating unique tools and unique resources where you can look at mitochondrial function in all kinds of things.
Isolated mitochondria and cells and organs and tissues from humans. Everything you can imagine the lab was able to do. And we developed these over the last decade and a half. And it’s really come to fruition, to now commercializing a test that people could do this in the comfort of their own home.
Dr Mike T Nelson: Very [00:08:00] cool. I did some work at the University of Minnesota took some classes and work with Dr. Paul Ozio. Okay. And he did a lot of work with, he was an anesthesiologist but looked primarily at cardiac function. And so the two things he had looked at in the past was people who had gotten very cold core temperatures, usually did a bunch of research on Lake Superior with, basically taking people and getting them quite cold.
’cause they’ve shown that’s cardioprotective. Then he also looked at hibernating bears. Yep. To try to figure out like what’s going on in their systems.
Dr Patel: They, yeah. So we were in the same space, but in the other extreme, so we were looking at how heat stress,
Dr Mike T Nelson: oh, the other end,
Dr Patel: right. So, cold stress does the same thing.
It activates heat shock proteins to create. Chaperones and which help your proteins fold the right way and protect them from damage. And then hibernation was always a fascination of mine. One of the big questions in this field has been what induces a hibernation induction trigger? [00:09:00] Right? Something after, right.
Trigger it. And so I don’t know who does these studies, but people go poke bears and bleed them when they were going to this place. Yep. That’s
Dr Mike T Nelson: what he was doing.
Dr Patel: When you look at their plasma, it becomes this almost milky white kind of consistency. And so one of the thoughts that has always been there is that you get this massive release of lipids that then cause this hibernation induction trigger and possibly that there’s a secreted opioid, like an endogenous opioid that creates this effect as well.
So lots of overlaps in ties. Yeah, on the, what did you find on the heat stress side? You could raise, you could elevate core temperature for a short amount of time and you would elevate these heat shock proteins, inducible proteins. I think we were focused on heat shock protein 72 as a major factor in creating this, and you could see this protected state that would come about from this.
And this has been done over and over again in animal models. I don’t know if it really works in humans. I guess you could try [00:10:00] hot yoga and see if that creates Yeah. Effect. But the correlate, I don’t know. It’s interesting to, to see there’s a lot of focus on this right now with, all the climate change things and other.
Things that are happening in the world Sure. That, that the world is getting hotter. And so heat may create stressors. And the caveat to this is and I think Nietzsche said it right, what that doesn’t kill you makes you stronger. But if you get too much of something, it will eventually kill you. And so the worry with the heat is small bursts of heat for short amounts of time are protective.
Long periods of that stress may be detrimental ultimately. Right. And so that I think has to be balanced in a unique way.
Dr Mike T Nelson: Yeah. What do you think about this? So one of my thoughts is that we have systems that we have to hold very constant. Obviously, temperature being one of ’em, right? 98.6.
Dr Patel: Yep.
Dr Mike T Nelson: We can vary a little bit on core temperature above or below.
But we have a fair amount of data from sauna and from heat [00:11:00] adaptation showing positive benefits. Some data from cold, probably not quite as much. So my bias is if we can expand the kind of that human dynamic range, you can be more adapted at heat and you can be more adapted at cold. Yeah, I think that’ll transfer into other areas of physiology we haven’t really looked at yet, but.
In terms of benefits, I don’t know what your thoughts are on that. Just like, exercise, like a short stimulus of something to move it in that direction.
Dr Patel: I think there’s something there, right? I think we’ve been looking at heat, stress, cold stress, other things. Lots of labs have done it. It definitely pans out in preclinical models.
Whether it works in humans. I think that’s an open-ended question. Yeah. There are some studies that have shown a positive trend, but nothing that’s really extensive that people have done with cold and heat stress. And this is what most biohackers are doing right now. Either they’re doing these infrared saunas or they’re plunging into a cold plunge or putting their face into a cold [00:12:00] bowl or other things.
I think it’s. It may work for certain individuals and it may not for others, right. I think it BA may has a lot to do with your genetics, your baseline mitochondria, how old you are, what are your comorbidities and all these things, I think play into that ultimately.
Dr Mike T Nelson: Yeah. Yeah. Back to mitochondria.
Yeah. How do you view. Increasing mitochondria. And would you say having just more, and my little air quotes here, more mitochondria is good? Or how should people think about what mitochondria are doing and the upregulation of them?
Dr Patel: Yeah, it, it depends again, right? Any, anything that is really good can be really bad for things like cancer.
This is one of the caveats we work with in biology is anything that allows cancer to survive. Is horrible for cancer, but could be great for the heart or great for the brain. Because those cells don’t respond and survive to stress in an optimal way like cancer does. And so there’s that caveat and cancer is a prime [00:13:00] example of this.
One of the things that is a trigger for a cancer cell to divide is the fission of mitochondria in that cell. That gives, that cue that. Oh, I need to start breaking up my cell material and making a second cell to then allow for that. So I think there’s a caveat to all of that. I think one of the hot areas right now that, that is just starting to take flight and I think it’s open-ended, and whether it’s gonna be positive or negative, is this concept of mitochondrial transfer, right?
That you can actually purify and source mitochondria from an optimal source and then transfer it into systems that are not doing so well. To replenish those new mitochondria We’ve played around with this in the lab. I’ve read lots of grants and there’s a few papers that have come out on this that show some positive benefit, but I think we’re in the early days right now, but I think there is some caveat to more mitochondria.
I. More functionality. I think where it matters is gonna be in organs that consume a lot of energy and make a lot of energy. So heart may be one of these [00:14:00] places, the early preclinical studies that have been done on this they basically take a heart failure model in an animal and they do autologous mitochondrial transfer.
So they’ll identify an organ bed that’s not damaged, and so they’ll create a heart failure model. They’ll take some skeletal muscle from that same animal, purify mitochondria from that skeletal muscle, and they’ll inject it into this disease myocardium. And it’s magical. The heart failure tends to go under control.
Less pathology in those kinds of things. So, the preclinical data always is very promising. The translation to a human. Condition becomes way more difficult ’cause there’s so many barriers that you have to go through. But it’s an interesting idea, I think, ultimately
Dr Mike T Nelson: is that, do we know in that model what the mechanism is?
’cause correct me if I’m wrong, if I remember right, I. Some of the studies on cardiac tissue with mi, so myocardial infarction where they had a scar, they did some of the early stem cell work [00:15:00] and they put stem cells in and they saw, increase in ejection fraction, these great outcomes. Yeah, and I believe it was later when they radioactively labeled them somehow.
Most of the cells weren’t there. They weren’t. They’re like, where did they go? What We saw this good functional outcome,
Dr Patel: This has been a huge conundrum in, in the regenerative space, is the heart is an organ that once it dies, it doesn’t really regenerate Right. In a massive state or another heart attack.
Yeah, there’s probably a turnover of maybe two, 3% in an extended period of time, but a massive injury, you just can’t replenish that much tissue. So the holy grail of this. People thought was, take stem cells and put them in. Turns out stem cells don’t integrate into the metabolism of the heart. One of the hypothesis we’ve had in this space is the reason why those cells, you can’t find.
A month, two months, three months, six months later is metabolically, they’re very different than what an adult cardiac myocyte would look [00:16:00] like. So those cells can’t metabolically couple and so they can’t metabolically in tune. There was a study done early days with this by Bob Cloner. I think this was, he was at USC at the time.
The strongest data I’ve ever seen for cell integration into myocardium was where he took neonatal myocytes. So these are myocytes that are past the stem cell stage and they’ve turned and they’re starting to turn into cardiac tissue. And when he integrates these into an adult heart, they’re actually there six months later.
And so really look metabolically more similar. And so I think the problem with stem cells. Is you just have to coax them along the metabolic pathway to look more like an adult, to get them to integrate The benefit that people saw initially of that stem cell injection and with ejection fraction and those things going up, they think now is all tied to pericrine factors.
So these stem cells were releasing, right? All kinds of factors that then create that positive benefit. But again, once they’re gone in a month or so, they don’t see that effect anymore. [00:17:00] So
Dr Mike T Nelson: interesting. So. On the mitochondria, did they think the mitochondria are incorporating into the cardiac tissue then?
Is that correct? Or are they doing some other type of function?
Dr Patel: Yeah, if you go back to where, how mitochondria came into existence in, in sort of modern day cells. It was an event that happened 1.52 billion years ago. Where a primordial cell found itself next to a mitochondrial bacteria and the bacteria is like, oh, it looks cool.
So it decided to go inside that cell and the cell’s like, wow, I feel super energized. Right? And it didn’t let go of this. And it created this symbiotic relationship that started, and it really evolved to creating complexity in life and growth and all the things that we see today. So it was this infective thing from that initial stage, and so I don’t think they’ve ever lost that ability to move in and outta cells, and so I think this is how they’re seeing it.
I don’t, I haven’t, I can’t remember if I’ve seen a recent paper that’s looked at the dynamics of how you get mitochondria [00:18:00] to move from an extracellular space into the actual cell, but people have done labeling studies where they’ll, or they’ll take from a donor and label them with a green tag. And then they’ll look at cells and the ost see green things move into cells.
So I think they have that ability to transfer through the membrane.
Dr Mike T Nelson: Interesting. So would the theory then hopefully be maybe in the future if you have. Some sort of mi we can, give you a bunch of mitochondria to try to, pick up the function in that sort of damaged area of that cardiac system.
Dr Patel: Yeah, I think that’s where this work is headed. I think that’s what people want to try to do eventually.
Dr Mike T Nelson: And for athletes, would there eventually be, instead of blood doping, would there be like mitochondrial doping? Could they just
Dr Patel: possibly, right. Take in a
Dr Mike T Nelson: bunch of mitochondria would, do you think that would even.
Incur a performance improvement.
Dr Patel: It’s I guess that’s one of the things that, that, that is an open-ended thing, is [00:19:00] what’s the limiting feature in an endurance athlete? Is it their ability to get oxygen into their tissue? Is it their mitochondrial performance? Is it the mass of the muscle?
All of these things go into it. And I don’t know. I think mitochondria are one conduit to this. They are what make that energy. Right. And if you shove more into that same space, you may create a bigger powerhouse ultimately.
Dr Mike T Nelson: Yeah. And it might end up being similar to the research on VO two max.
Like you go back far enough in time, people are like, oh, it’s the holy grail of endurance performance. And then. Oh, it’s one of the factors. It’s not the factor.
Dr Patel: Yeah. I, and that’s where I think humans become really complicated is organisms get more and more complex. There’s just so many things that interplay together that ultimately feed into performance and everything else that happens,
Dr Mike T Nelson: yeah. So tell us about the test you have that can look at. Mitochondria and give us some information about what’s going on with them.
Dr Patel: Yeah, so the gold standard in this space has [00:20:00] always been a muscle biopsy, but who wants to have that done right? And it’s tough. If you wanna get it done, it’s hard to find a place to do it.
Dr Mike T Nelson: Yeah.
Dr Patel: So typically we do it as part of clinical trials on campus where we’ll have. Recruit subjects into a trial. They’ll come into the OR setting, their leg will be numbed with a local anesthetic and you take a giant needle, stick it into the, that muscle, you pull some of that muscle out, it comes to a lab like mine, and then we spend the next six hours I.
Excruciatingly looking at how the mitochondria are functioning in that tissue. We can do microscopy with electron microscopes to look at ultra structure and things like that. On a good week, we can do maybe six or seven of these in the lab. And so there’s really no way to scale or do anything commercial with this kind of thing.
So we’ve been trying to find in the lab for years is a way to, to generalize this to other things that you can capture easily from a human. And so we were involved in the NASA twin study where the twin went up into space for a year. Oh yeah. And the twin [00:21:00] on ground. And so UCSD was one of 10 sites that was selected.
The site PI was Brenda Rana. And Brenda and I are good friends and we were postdocs together in Paul Intel’s lab back in the day. And so she knew all the mitochondrial stuff we were doing, and one of the questions that NASA had was about mitochondrial functionality. And so she came to us and said, would you wanna be involved in this?
We’ve got some, could you come up with a way to, to look at mitochondrial function limitation? There was, we couldn’t get any tissue right, but we can get plasma at unique time points before flight. Every three months during flight and then unique time points after. The big question was, could you now use this plasma as a way to predict which organ would de sort of dysfunction at what specific time in flight?
So the idea came up with was that the plasma is a biochemical capture of who you are, right? So it’s got your exosomes, proteins, metabolites, all the things that you’re making as a consequence of your genetics, your mitochondria that are in all your cells except your red blood cells, your [00:22:00] microbiome. All of this is contributing to that nature of the plasma.
Typically what people will do right now is they’ll do the organic acid test as a way to, to track your mitochondrial functionality. So four factors that you pee out are supposed to indicate what your mitochondria doing globally in your body. I dunno if that’s a good indicator, but anyway,
Dr Mike T Nelson: I want to believe that test and take all the data and run to the bank with it.
But I. I don’t think it’s that direct. Yeah, I wanna believe it though. Yeah. I want it to be that simple. I
Dr Patel: would think. Right. So ours is simple, but it takes that to the next level. So we are not concerned with four factors that you’re changing. We’re concerned about your entire biochemistry. I.
And we captured it in that plasma. And so what we designed for NASA was basically a human on a plate. So we bought cells that represent every organ of the body from a commercial source, and we could put them on a plate. And then we essentially added the plasma to these cells to see how the cells would respond to that entire.
[00:23:00] Biochemical environment that individual creates at specific times during that intervention. And so we were able to predict unique changes in muscle dysfunction, immune dysfunction, endothelial dysfunction at specific time points based on that biochemistry. And so now you’re. Closer, right? So now you don’t have to do muscle biopsies.
You can go to Quest, LabCorp, get a blood draw, can be processed, shipped to the lab, you can do the study. So we have some scalability, but there’s still a barrier. Humans are naturally averse to going out and doing, interacting with other humans to give them stuff, right? And so we wanted to simplify this even more.
So we’ve miniaturized this to a blood card. So these bilayer a DX 100 cards essentially. That lots of companies use for collection of blood samples. You poke your finger, the kit comes to your house, you poke your finger with a lancet, four to six drops of blood on one of these windows, and the bilayer wicks the serum out into the second window.
The car dries. We’ve shown stability of that sample once it’s dried [00:24:00] to two months at room temperature. So basically we can capture sample from anywhere in the world. It comes to our facility. We punch the serum out, we reanimated in our buffer, and we essentially run the NASA type assay. The current, so the test is called the ME screen, so it’s a mitochondrial deficiency screen and the tagline for brace discovery is a healthier you begins with me, right?
And this concept that. Most people don’t think of a healthier use starting with mitochondria. ’cause there really hasn’t been a way to measure this. And so we think that this is really a new vital sign that we’ve developed that people will be able to access in this unique way, just like you would measure your blood pressure or other things.
We think your mitochondrial health is that important to get a sense of what it is. And so. We basically solubilize that serum. From that card, we put it onto a muscle cell, which becomes the core of what me screen is, and we can measure all kinds of parameters of mitochondrial function on this muscle cell.
We can look at baseline respiration. We can look to see how [00:25:00] efficient the mitochondria behaving with U Chemistry adapted to it. We can look at their potential to drive functionality. We can look to see if they’re using mitochondria or glycolysis to make energy. We can see if they’re making reactive oxygen species in a basal, in a stress state.
And then we’ve created a stable cell line that expresses a green tag only in mitochondria. And so the mitochondrial network in the cell, I. Lights up. So when we adopt your biochemistry to the cell, we can see if the mitochondria fusing, fizzing moving around, doing unique things to the network dynamics as well.
So with a few drops of blood, we can give you really deep insights reflective of what your mitochondria doing likely in your muscle cells from this simple assay that we run, right, functionality dysfunctionality, as well as some dynamics and structure information.
Dr Mike T Nelson: Oh, that, that’s super interesting.
Yeah, let’s dive a little bit deeper into some of the different functions there. Before I do that, [00:26:00] at some point, would this. Potentially as an offshoot, even be like a screen for different types of cancer or different things like that since you can we see them moving around and changing to, we have to sort, I know it’s consumer great thing, but Right.
Dr Patel: We have to draw the line somewhere, I think. It’s not a diagnostic yet. We can’t make any claims. It’s a wellness kind of test right now. Right. We are in the process of writing grants through SBIR and other mechanisms to then validate this as a possible diagnostic moving forward. The path is long and arduous to get through that process, but we think that there may be patterns that develop for cancer, for neurodegenerative diseases, for cardiovascular diseases.
We may see this ’cause a lot of these are tied to metabolic changes and bio changes in your blood. So,
Dr Mike T Nelson: yeah. Very cool. Yeah, so give us like, so if we do the thing, we bleed on the paper, we send it in, like what are some of the top things we’re looking at on there? So if someone isn’t real well versed in biochemistry or [00:27:00] mitochondrial function, they get the results back.
Yeah. Like what are some of the top things you can, yeah. So tell them about themselves. So the
Dr Patel: word that a lot of mitochondrias throw around is respiration, right? They call it right. Mitochondrial respiration. So what is that? Actually means, so they’re aspiring, your mitochondria are actually using that oxygen that comes into your body and they’re using it to create fuel at the end of the day through a biochemical reaction.
So there’s a bunch of proteins that sit on the mitochondria and the we can go. Deep into structure function kinds of things. So from the basic core point it looks like a bacteria. When you look at a bacteria, it’s got different membrane systems. So the mitochondria actually has unique membrane system where it has an outer membrane.
I. An inner membrane and a matrix in the inner membrane. There’s these proteins that sit in sequence and they create what’s called the electron transport chain. So they’re tra and scientists are stupid, dumb simple in terms of labeling and naming. So the ETC, the electron mean
Dr Mike T Nelson: fasting electrons don’t [00:28:00]
Dr Patel: right it.
It transfers electrons on a chain, essentially is what it’s. Doing. And so it’s bouncing around electrons and it’s using oxygen as one of these final electron acceptors and donor acceptor kinds of things. And at the end of the day, if everything is working perfectly, you’re making water and you make a ton of a TP in mitochondria.
Which then becomes available for the cell to use to grow and do all the things it needs to do. If there’s dysfunction, you’re actually using that oxygen to do the opposite end. You’re making a free radical, and so you’re making superoxide, hydroxyl, oxy nitrite, ’cause there’s lots of nitro oxide synthase in mitochondria, and you get that generated as well.
And this will then cause damage. And so in one organelle, you have either life or death controlled by this calculus of what happens to respiration. Moving oxygen and using that to make energy or non-energy, molecular fire essentially on the other extreme. And so that’s what the mitochondria are doing and what our test is looking at is we have a system that [00:29:00] constantly measures oxygen and it’s constantly measuring.
Extracellular rec, acidification old technology that Agilent ultimately acquired. And lots of labs use this, and so we’re able to measure in real time what the cell is doing in terms of using oxygen in mitochondria. And using glycolysis to make energy in a more, less efficient kind of way.
Right. And by integrating this, you can learn a lot about what that system is doing from a functional versus a dysfunctional endpoint. So one of the first things we look at is we have this cell cooking away, right? It’s consuming oxygen. We add your environment to the cell, and we look to see what the basal state of that cell does.
Does it start using more oxygen, less oxygen? And this becomes indicative of where your mitochondria are. In a perfect world, you want to be average on this first test. You don’t want to. Overstimulate mitochondria, you don’t wanna shut them down. What we see interestingly is that some individuals, a lot of biohackers tend to overstimulate [00:30:00] or either suppress mitochondrial function in this baseline setting.
And I think it’s just a consequence of either they’re exhausted in terms of their mitochondrial state, or they’ve just started and they’re over tweaking. Mitochondria to work more than they should the best. So they’re
Dr Mike T Nelson: kinda like whipping the poor little mitochondria. Getting to do more output. Yeah.
Just mean one of the things I think and work harder. Work harder.
Dr Patel: Yeah. One of the things I think that has been tried and true, proven in literature is the people that live longest. May not be the best way to do it, but it’s if you’re actually suppressing metabolism in a unique kind of way that you can live longer.
So caloric restriction is one of the only things that’s been shown in most organisms to cause longevity. Even in humans, it’s a horrible way to live. Right? Who wants to eat a thousand pounds? It’s miserable
Dr Mike T Nelson: because it was like. Pretty severe caloric restriction, I think. Right? Like 30, 40%
Dr Patel: calories a day, I think is what
Dr Mike T Nelson: Yeah.
Yeah. It
Dr Patel: came down to and what you’re essentially doing in that state is you’re shutting metabolism down. You’re going almost like we were talking about earlier, like a hibernated kind of state. Where your [00:31:00] mitochondria become this sort of non resilient thing, but they’re. Not making energy. If they’re not making energy and you shut them down, they’re also not making free radicals.
And so they’re basically just there to maintain a routine kind of thing that needs to get done. So the baseline respiration becomes a huge feature of this, right? Just the resting state of what the mitochondria doing. Then we start adding chemicals to the system to really. Stress and test the mitochondria in unique ways.
With your biochemistry adapted, we can look at the efficiency state, whether oxygen’s moving the way it should and stopping when it should. We can then uncouple the mitochondria and make them work as hard as they can to then see if your biochemistry supports this super rise in oxygen and consumption as a measure of what the reserve capacity you may have.
And then what we can look at is, again a baseline setting under just. Non-stress conditions. How are you making energy? Are you using mostly mitochondria or are you using glycolysis to cycle and make that a TP in your system? And we [00:32:00] see unique patterns, right? Elite athletes tend to use more mitochondria to make energy than glycolysis.
We see the general population tends to have an equal balance of both of them. And then we see individuals that may be energy compromised through diseases, chronic fatigue, other things. They prefer one or the other pathway and they really use this as a compensation and so we can toggle some things there as well in an individual.
And then that dysfunctional element, right, this fluorescence based assay that we’ve developed that looks at free radical generation. So we can actually look under basal conditions. When your environment is adapted to that cell, does it start to make free radicals or not? And then we stress the system.
And so the stressor is always the uncoupled mitochondria where there. They’re working, they’re exercise, right? They’re making as they’re moving as fast as they can, and we see if that ROS level goes up or down. And then we do the same thing for the network under basal and stress conditions as well. So it gives you a pretty cool picture of your mitochondria.
Dr Mike T Nelson: So it’s almost like [00:33:00] if I zoom all the way out and I look at, from an exercise physiology standpoint, you’re doing what we would do in the lab. Like you’re, like you get your rusty metabolic rate. How much energy just to hang out, like how much of that energy is from fat? How much of that is from carbohydrates?
If we stress you, we stress the shit outta you with exercise, what happens to your fuel changes, like how high of a stress level can you handle? How much oxygen can you run through the system? Is it similar to that but you’re looking at Yeah, essentially that mitochondria
Dr Patel: and we’re, and the way we’re basically adopting you is by capturing your biochemistry.
’cause that’s what your cells are seeing. Right. When you’re doing this in your own body, right? And so we think that it’s a really cool way to look at what’s possibly happening inside you when you go under those stress states as well.
Dr Mike T Nelson: And from that, do, is there recommendations people can do? Is this changeable with, attrition and exercise?
Do you give them Yeah. So we’ll give some direction, we’ll give
Dr Patel: you some suggestions. Yeah. And [00:34:00] this is one of the things that looking at mitochondria for all these years that we have been, one of the things we continue to see is that. There’s a probably a thousand plus ways of changing your mitochondria.
Dr Mike T Nelson: Sure.
Dr Patel: Fortunately, they just don’t work the same way in every individual, so for some individuals, time-restricted eating may be magical and it completely transforms their metabolic fate and state. Whereas for others. They’ve got other things that just preclude that from doing what it’s supposed to do. What we think the ME screen allows this to do, and I’ve jokingly called it the bullshit detector, right?
It allows you to now see all the things that you’re spending money on and all Yeah. Yeah. You’re investing your time and energy into are they actually moving the needle in terms of changing your energetics? And in the past the best way to do this, and we’ve talked to lots of providers and stuff.
How do you know? And they would be like we just ask people if they feel better, right. To see if their mitochondria are working better. I, that seems like a really low bar to, to test. Yeah. Right. And so [00:35:00] now there’s an objective way to do this and there’s. Thousands of products out there that claim mitochondrial changes in targetability and those sorts of things.
As a, as an NI can’t remember what the supplement was when we first were developing this test, we bought the most expensive supplement you could buy that says. This will improve your mitochondrial functionality. I had some postdocs take it for about a month in the lab and we did a pre-post test. It did absolutely nothing.
Right? Yeah. And so this will allow you to see and some things, like I said, will work for certain individuals and others won’t, and it would give you the power to figure out what’s actually optimized for your system and how to tweak it.
Dr Mike T Nelson: Oh, that, that’s what I thing. That’s so cool. And that’s one of the things I love about exercise physiology testing is again, you have testing.
Yeah. Like, hey, we do your baseline test. We give you this prescription or this thing you need to go do. You do the thing and then we shocker, we retest you. Right. Did the thing.
Dr Patel: Yeah.
Dr Mike T Nelson: Get you a better result. You’re paying me all this money for [00:36:00] Yeah. But you can look at it and see, was it actually moving the needle or not?
Yeah. Yeah.
Dr Patel: No. So we’ll see how it does. I think people are starting to get wind of this and I think it, it really, think about how much money most people spend on self-care and these kinds of things, especially if you have a chronic disease and other things that you’re working on, right? This would give you a way to, to really create a barometer to test that, a new vital, essentially,
Dr Mike T Nelson: what do we think like the plasticity of mitochondria is?
So if they come in, they do this test, I’m gonna do some type of intervention. Do you think it’s like a four week, eight week, couple months? Like what do you think that kind of time domain is? I
Dr Patel: think, I for most things, it’s not a, an instantaneous thing, right? Right. I think we’ve been looking for that and I think most people want that, but there isn’t.
But unfortunately there’s no magic bullet. In everything we’ve looked at, I think the average is about two to three months to get a change in functionality. And I think that’s probably the scale at which you wanna do. [00:37:00] ’cause anything you can do for a week, try to do it for two months or three months.
If you’re gonna peter out, I. Right. In most cases, after two weeks, your life’s gonna catch up with you and you’re gonna move on to other things. And so we really wanna have people, if they’re gonna engage in this, to do this every two or three months, where they really start to incorporate one thing into their routine to see how it’s impacting their mitochondrial function.
And if it’s working, then maintain that long term and then start stacking and adding things in. One of the things that I’ve been thinking about as a cell biologist is how do you fix mitochondria? And I think there’s a couple ways to think about it from a biological perspective. Most people we look at and most things in disease systems is I.
That the membrane starts to fall apart, right? Most people have really crappy membranes, which leads to chronic diseases and aging and other things. So at the first level, I think you have to replenish your lipids and lipid kinds of things that will make better membranes. Your plasma membrane has to be replenished your mitochondrial membranes [00:38:00] or nuclear membrane er.
Everything in your cell has a membrane structure that creates uniqueness to it and what we see in systems that are failing is that those membranes become. Less and less differentiating, right? And so you gotta rebuild that structure. So that I think is a core element to this, which is one of the things we suggest to a lot of people.
The second phase of this is once you’ve got the membranes in place, you gotta get rid of death dying decay in your cells, right? And this is really activating autophagy, autophagy pathways. They clear out all of the dead things that are accumulating space and energy in your system. Once you start getting rid of those, you can replenish with new mitochondria, with mitochondrial biogenesis and other things that create a resiliency to create more energy and utility.
The final thing is something that you battle from. The minute you’re conceived to the minute you die is how do you deal with the oxygen around you? Right? It’s life saving and preserving and maintaining, but at the same time it’s what’s killing you at the end of the day. [00:39:00] Right. It’s this constant load of oxygen that your biological systems have to adapt to.
If you go back to terrestrial animals and the rise from ocean into to land, what do you think was the biggest adaptation that allowed us to live on land with oxygen in the environment?
I don’t know, membrane cholesterol. So it turns out that really evolution of membrane cholesterol arcs almost identically with the appearance of terrestrial animals. Huh. And so the idea is that cholesterol actually binds and holds onto oxygen. And so I. This may be a conduit, really how you had this adaptation and some ideas around this is if you think about the largest density of cholesterol in a membrane structure in our bodies is in our lungs.
Right? In these endothelial and alveolar cells. You have a. Ton of cholesterol, and this is this conduit of exchange for air to, to body level cholesterol. The other interesting thing, [00:40:00] one of the first side effects of these early first generation statins. Was people would get cataracts.
Turns out the lens fiber in your eye has one of the highest densities of cholesterol in your body. So if you’re reducing that cholesterol, you’re actually creating some moments of oxidization, which then you can get these cataracts form. And so there is this interesting tie to membranes and oxygen and cholesterol and those kinds of things.
And so this is this constant battle, right? How do you handle oxygen in a living system where what you want it to do is make energy. But what it wants to do is make free radicals instead. Right? And so you gotta balance this. And so as you get older, as you get chronic diseases and other things, that calculus shifts more towards making reactive oxygen species than energy ultimately.
And so I think if you can balance lipids, the autophagy, autophagy. And this oxidant load, I think you could really master your mitochondria, but it’s not something that you can do overnight or an instant. Right. It’s something that really is a concerted process, I think that can take [00:41:00] months to, to ensue.
Dr Mike T Nelson: Yeah. And you go back to talking about oxygen. I keep thinking of the, when we started talking about with like preconditioning, yeah. Of at a basic level, like. Why does cardiovascular exercise seem to be very protective for the heart? Yeah. At some point it’s probably some level of preconditioning.
It’s a controlled decrease in the amount of oxygen the body goes, Ooh, ooh. Oh, we gotta find ways of upbringing in this. This crazy person might go do this again.
Dr Patel: Yep. And one of the things that most people don’t realize that are in that space is. It’s not you. You don’t really die from that ischemia if you’re reperfused, right?
If you get right, if you get long enough, if you get ischemia long enough, you will die, right? If you stop blood flow to the heart for that long, but it’s really reperfusion injury and reperfusion injury, what you’re doing is you’re. Flooding the system with oxygen and the mitochondria don’t know how to handle all of that oxygen.
And so the easy thing for them to do is make free radicals rather than energy at the end of the [00:42:00] day. Oh, and so this is what they think Preconditioning does, is it conditions the mitochondria to be able to handle that intense oxygen load they get during that reperfusion phase.
Dr Mike T Nelson: Do you think there’s any benefit then to, there’s like some of these systems like live O2 or I don’t have any financial disclosure with ’em of periods of hypoxic during exercise and periods of high levels of oxygen.
When I’ve looked at in the past. The data seems to be all over the place. Yeah. And then there’s, my buddy Caldis turned me onto some old Russian research that says, just giving people more oxygen wasn’t necessarily beneficial unless you could contain them in the high pressure environment.
Dr Patel: Yeah.
Dr Mike T Nelson: Giving them low oxygen, you just decrease performance so much that may not be the best thing.
So their result was. If you make them briefly hypoxic and then you give them hyperoxic that [00:43:00] it was the switching between the two. Supposedly was more beneficial.
Dr Patel: Possibly. We’re doing some studies. This is
Dr Mike T Nelson: like way out on a limb. I know.
Dr Patel: Yeah. We’re, we are actually doing some studies on campus to see if we can train, students to, to do hypoxic breathing.
And this would be a very simple hack, right? If you could learn and teach yourself to hold your breath for a minute and a half at a time, couple times a day, could this create a benefit? And there is some evidence. If you. If meditation has a lot of breath work components tied to it.
Dr Mike T Nelson: Yeah.
Dr Patel: And so breath work may be a huge relevant to, to activating these stress pathways, heat shock proteins, hypoxia, inducible factors, things like that completely change the dynamic of what your genes and proteins and other things are doing.
Dr Mike T Nelson: Yeah. And further down that pathway. I believe you’ve done some analysis of people doing meditation programs.
Correct. Looking at possible blood work changes.
Dr Patel: We have and I, you [00:44:00] see some phenomenal changes that happen in what have
Dr Mike T Nelson: you seen?
Dr Patel: Their blood completely transforms. Changes in their metabolites. Changes in exosomes, changes in lipids. We see brain level changes after meditation from the beginning of the week till the end of the week.
And this is just like a week long intervention. Like a Yeah. So this a high amount of. We have an exclusive thing we do with Joe Dispenza. So Joe and I have known each other now for about five years and Oh, cool. We started, he’s an amazing individual. He said, come in and look right and who Right.
Scientists to just come and look. Yeah.
Dr Mike T Nelson: That’s awesome. I’m like, Hey, that’s so cool, man.
Dr Patel: Yeah, no. And so we’ve been picking and poking and just. The things we’ve discovered are just absolutely amazing. And it’s really a process. I don’t think you can recreate it with other kinds of things, and they may be of interest in the future.
I think he’s masterfully created a week long event that combines all the right things to create a pre-post effect that we’re seeing in lots of individuals. And it’s not these small studies where you’re looking at [00:45:00] 10, 15 individuals. We’ve got data on probably seven, 8,000 people that we’ve looked at this.
Oh, wow. Yeah, it’s a lot of, that’s a lot of stuff.
Dr Mike T Nelson: If you were to speculate, what do you think are some of those things that if you were to kinda recreate the. The gourmet dinner? Like what would be some of the items you’d want to put in the list?
Dr Patel: In, in terms of the meditation or just in general?
Dr Mike T Nelson: Just in general, but even, I’d say in general, and then especially with regards to meditation.
Dr Patel: Yeah. I think I, I think there are ways that you can change without having to do a lot of, I. Exogenous things, right? The simple things we talk about and things that I struggle with, and you probably struggle with, eat, move, sleep. Those are three things that if everyone could do in an optimal kind of way, you get rid of a lot of things that we’re dealing with, right?
From a disease perspective. And it’s moving in the right way. It’s eating in the right way at the right times. And then it’s actually getting enough sleep where you’re shutting [00:46:00] things down and you’re letting that regenerative recuperative kind of thing happen. Most of us live a stressful life that just doesn’t allow for that.
Or allow for it an extended controlled kind of way. I think regimentation around this is really important and routine is critical. I talk to a lot of people, satin Panda and I collaborate on a bunch of studies around timers eating and you talk to individuals in this space and they’re like, oh yeah, I’m timers eating.
I’m like, I tell me what your window is. And like, oh, some days I started, I stopped eating at six and other days I, I’ve got work and I gotta go until nine. Like, then you’re not time eating ’cause you’re, yeah.
Dr Mike T Nelson: Yeah.
Dr Patel: That window around. Right? And so a regimen becomes really important to all of this.
And so that’s something I think that’s really important. Simple things that, that are f essentially free to do, right? You don’t have to pay anyone to do this, but it takes a lot of mental energy and time and individuality to be able to create this. The uniqueness I think of what Joe teaches you is this, and I think this is [00:47:00] where.
The simple things become very relevant is when you go through a week long event with Joe. I think what you learn to do is self-regulate and self-control. And so now that ability to eat, sleep and move become sort of key features and a lot of people start to live way more cleanly then if they weren’t doing that right.
This self-regulation process that you go through. And so I think they go hand in hand this idea of. Mind and body, I think really you gotta practice and learn from a master like Joe and then be able to apply it in this unique way to your life. So, and then there’s other things, right? There, there aren’t horrible supplements.
There’s some good supplements you can take as well. I couldn’t list them off right now, but there are certain things that will work for you and they’re really good products. That you can try and we’re starting to test some of these with me screen and we’ll see what comes out, at the end of the day, if they actually do what they say they’re gonna do.
So
Dr Mike T Nelson: yeah, that’s great. I. I [00:48:00] believe you’ve done some blood work and testing. I think it was looking at mitochondrial changes after a higher dose ayahuasca ceremony. Is that correct?
Dr Patel: We’ve been playing around with this one of our early collaborators when we launched me screen. Our CEO knew a guy who.
Run some retreats and we gave ’em some tests and we got some pre-post samples and we saw some really cool changes. But again, they’re acute changes I don’t think. Sure. There’s things you can maintain long term and this is supported by the literature. There’s lots of evidence and literature to suggest that these psychotropic agents create changes in metabolism.
There’s lots of evidence to suggest that diseases that tie to mental health disorders. Like PTSD psychiatric disorders, anxiety, depression, they have stuff to do with, they ultimately change mitochondrial functionality. And so it, it doesn’t take a rocket science to figure out the things that change those in a positive way.
You should see a positive change in mitochondrial biology. [00:49:00] And so we’re continuing to play around with this in a unique way. We’re trying to do an extended study where we look at some individuals, where we actually look at them weeks before they take their. Dose of ayahuasca to get a baseline assessment on that.
Dr Mike T Nelson: Yeah.
Dr Patel: And then do a lot of testing around ayahuasca during that ceremony phase. ’cause I think there is an acute and potentially a effect that lasts beyond the 24 48 hours that we’re seeing. And then we wanna see how long that effect lasts and ultimately goes away. Right. And looking at that long-term capture as well.
So we’ll see.
Dr Mike T Nelson: Do you think there’s something that might be unique to Ayahuasca or is it something more. Related to kind of psychedelic compounds in general, or who knows at this point?
Dr Patel: We don’t know, but I suspect that some of the things we see with the meditation work where it looks like the brains of these meditators look like they’re on psilocybin, right?
These psychedelic kinds of things. You can internally create that same environment that you can create through an exogenous thing. And then it [00:50:00] turns out, right, the thing I studied in grad school, these opioids. Turns out our bodies can make their own opioids. Right? There’s these in every so I guess the, a little more science in this, right?
Yeah. Opioids. Opioids belong to a class of proteins that, that ligand why? They bind in a in the body, a class of receptors called G-protein coupled receptors, right? These GPCRs or the serpentine receptors or these. Seven transmembrane receptors ’cause they go through the membrane seven times and so opioids as a ligand will bind to this receptor.
The receptor will change in unique way and certain things will get activated inside the cell or deactivated and stuff happens in order for a G protein coupled receptor to be de orphan and actually be named. You have to identify the endogenous ligand that binds to this receptor. So for a receptor to engage morphine, someone had to go and find the endogenous morphine that binds to this receptor, and then that became the mu opioid receptor.
And so our body naturally [00:51:00] makes this. And the other thing that’s unique about GP PCR is it’s the largest class of druggable receptors in our body. And so, if you can imagine it right now on the market, there’s about 2,500 drugs. That either directly or indirectly target a G-protein coupled receptor.
You can imagine these 2,500 drugs in one way target, something that you can naturally create yourself in your body, right? Through mind body approaches and other exposures and toxins and things that you can create yourself you can do this, right? And so this concept of this endogenous pharmacology becomes really important.
And so I think there’s ways to manage and manipulate this in human systems in unique ways. I.
Dr Mike T Nelson: Yeah, that’s super, super fascinating and different. In air quotes, natural call compounds will modulate it to, different degrees and yeah it’s a very complicated rabbit hole, but super interesting.
Dr Patel: Yeah, I think when there’s deregulation on some of these psychedelics with psilocybin being, you can test in cell models and things like that, I [00:52:00] think it’s gonna explode in terms of figuring out what they’re actually doing and how they’re doing it. Right now there’s just this taboo, I think in, we’re doing trials here on campus at UCST.
Yeah. On pain and psilocybin. I think there’s about 130 plus trials right now with psilocybin and then 50, 60 other trials with some of the other psychedelic agents. So it’s a hot space right now.
Dr Mike T Nelson: Yeah. And it’s always fascinating to me all the. The sort of pluripotent effects that they have too, from mind, body and Yeah and everything too.
And if people have ever used them, it is definitely an, I’ve done ayahuasca in Costa Rica a couple times and it was one hand fascinating to feel the effects firsthand. Because all the first ceremony I had, everything I had was very late. So I got to watch every single person go through their stuff before you know what happened to me.
Yeah. And it was fascinating to see the same set, the same setting, right. [00:53:00] Same location, relatively similar amount of dose, same source, and very dramatically different responses from everyone who was there too. Yeah. But yet at the end, having more, almost similarities than. Than not, so the internal experience of how it felt was I think a lot similar.
Yeah. But watching from the outside was very different at the same time. Interesting.
Dr Patel: Yeah.
Dr Mike T Nelson: Yeah. Awesome. And where can people find out more about the mitochondrial testing?
Dr Patel: I think you go to me screen.com and there’s some information there, and if you want to order the test, you can order it from there as well.
Dr Mike T Nelson: And so direct to consumer. Anybody can order the test then? Correct. Yeah.
Dr Patel: Anybody can order it. Yeah.
Dr Mike T Nelson: And one of the questions people have all the time is price. Is this something that hopefully as more people get involved in manufacturing everything else, like hopefully the price will be able to go down over time?
Yes.
Dr Patel: We, as we increase the consumer launch, the price will go down with time. And then the idea [00:54:00] would be to really if we’re gonna transform people’s mitochondrial health, it can’t be a once and done test, right? It’s something that you really need to do as a vital every couple months. And so we really want to bring that price down so people can start doing this as a routine part of their checkup of who and what they are.
So it’ll come down for sure. Yeah.
Dr Mike T Nelson: And it’d be great even if it just becomes just like getting blood work now. Yeah. Like, hey, I do my CBC, I do my CMP. Hey, I do my me screen. I see what’s going on with my mitochondria.
Dr Patel: Yeah. Yeah. Hopefully.
Dr Mike T Nelson: Yeah. Awesome. And then last question. What would be like your top, if someone says, just in general I wanna improve my mitochondria, what would be the top four things you would recommend them looking into or doing?
Dr Patel: Lipids, right? We talked about those three things. So lipids find some good lipids to, to take change a diet that has really good lipids. I tend to favor olive oil from Morocco, right? It’s got, it lives in a stressed, it grows in a stressed environment. And so those trees put a lot [00:55:00] of energy into making that fruit.
And if you look, it has one of the highest antioxidant contents in the world of all of them. And so then you hit sort of two things at one time. You get the antioxidant potential and you get that lipid component as well. Autophagy, autophagy, activators. There’s natural ways to do this. Hypoxic breathing is one way.
Intermittent fasting is another way. Try those things first and then move into. Supplements and things after that fact. I think one of our approaches is really how can you do this with diet, exercise initially and mind body approaches, and then if that doesn’t work, how do you move to taking things in exogenously ultimately?
And then the antioxidant thing. I think really balancing those antioxidants and mitigating this, your mitochondria need an oxidant environment for certain things. But there’s a critical balance, right? You’d need free radicals to signal, but once they hit above that threshold, they cut, start causing damage.
And so you gotta balance that aspect. And then the fourth thing would be [00:56:00] how do you find something that you can do more than two weeks, right? And continually do this as part of your routine, whatever that may be. And I think that’s the big challenge that all of us face.
Dr Mike T Nelson: Yeah. Awesome. Thank you so much for all your time, all your research.
That was great. Everything you’ve been doing really appreciate it. And where can people find out more about you? I know you’ve got a bunch of stuff on Instagram and other locations.
Dr Patel: Yeah, Instagram. I have to always look ’cause I don’t do very well with Instagram, so if you wanna find me on, we’ll find
Dr Mike T Nelson: it, we’ll put it in the show notes for sure.
All right,
Dr Patel: perfect. But yeah, Instagram is a good way to follow us. We put lots of facts about mitochondria and stuff on there. And we’ll share all things that are happening in the lab and at versa and in the meditation world. And everything that’s going on in my life gets posted on there. So you get to learn about that.
Dr Mike T Nelson: Awesome. Thank you so much. I really appreciate it. That has been great. Thank you once again. Yep. That was a lot of fun.
Thank you so much for listening. Really appreciate it. Big thanks to Dr. Patel for all of [00:57:00] his time here sharing all of his knowledge with us. If you enjoyed this podcast, please forward it to a friend or tag myself online so we can say thank you. Hit the old link, subscribe, download all the wonderful things that makes the algorithms nice and happy.
Thank you so much. We will talk to all of you next week.
A great little actress. Yep. And getting smaller all the time.
Speaker 2: This podcast is for informational purposes only. The podcast is not intended as a substitute for professional medical advice, diagnosis, or treatment. You should not use the information on the podcast for diagnosing or treating a health problem or disease, or prescribing any medication or other treatment.
Always seek the advice of your physician or other qualified health provider before taking any medication. Or nutritional supplement, and with any questions you may have regarding a medical condition, never disregard professional medical advice or delay in seeking it. Because of something you have heard on this or any other [00:58:00] podcast, reliance on the podcast is solely at your own risk.
Information provided on the podcast does not create a doctor patient relationship between you and any of the health professionals affiliated with our podcast. Information and statements regarding dietary supplements are not intended to diagnose, treat, cure, or prevent any disease. Opinions of guests are their own, and this podcast does not endorse or accept responsibility for statements made by guests.
This podcast does not make any representations or warranties about guest qualifications or credibility. Individuals on this podcast may have a direct or indirect financial interest in products or services referred to therein. If you think you have a medical problem, consult a licensed physician.




Leave A Comment