Join me, Dr Mike T Nelson, on the Flex Diet Podcast as I explore the pros and cons of GLP-1 agonists like Wagovi and Ozempic with Dr. Chris Morrissey, a fitness professional and general surgeon. Dr. Morrissey shares his unique insights on the benefits and potential risks of these medications, along with his top recommendations for optimizing results and mitigating risks.
We also discuss the challenges of training in extreme heat, sharing personal experiences and tips for acclimatization, and compare notes on how our bodies adapt to varying temperatures, with a preference for cold-weather training.
-
(0:00:00) – Medications and Training in the Heat
- (0:09:04) – Physician Training and GLP-1 Agonists
- (0:14:17) – Medications and Gallbladder Issues
- (0:22:52) – Appendicitis, Intestinal Issues, and Medications
- (0:35:30) – Risk and Consequences of Medications
- (0:40:25) – Potential Consequences of Weight-Loss Medications
- (0:52:22) – Monitoring Progress and Motivation Through Data
- (0:56:53) – Concerts and Music Talk
- Tecton Life Ketone drink! Use code DRMIKE to save 20%.
- Dr. Mike’s Fitness Insider Newsletter: Sign up for free here.
Flex Diet Podcast Episodes You May Enjoy:
-
Episode 140: 3 Common Health Procedures You Need To Know About with Dr Chris Morrissey
- Episode 263: Lifestyle, Longevity, and the Future of GLP-1 Agonist Use in Wellness with Christa Rymal
Connect with Chris:
Rock on!

Dr. Mike T Nelson
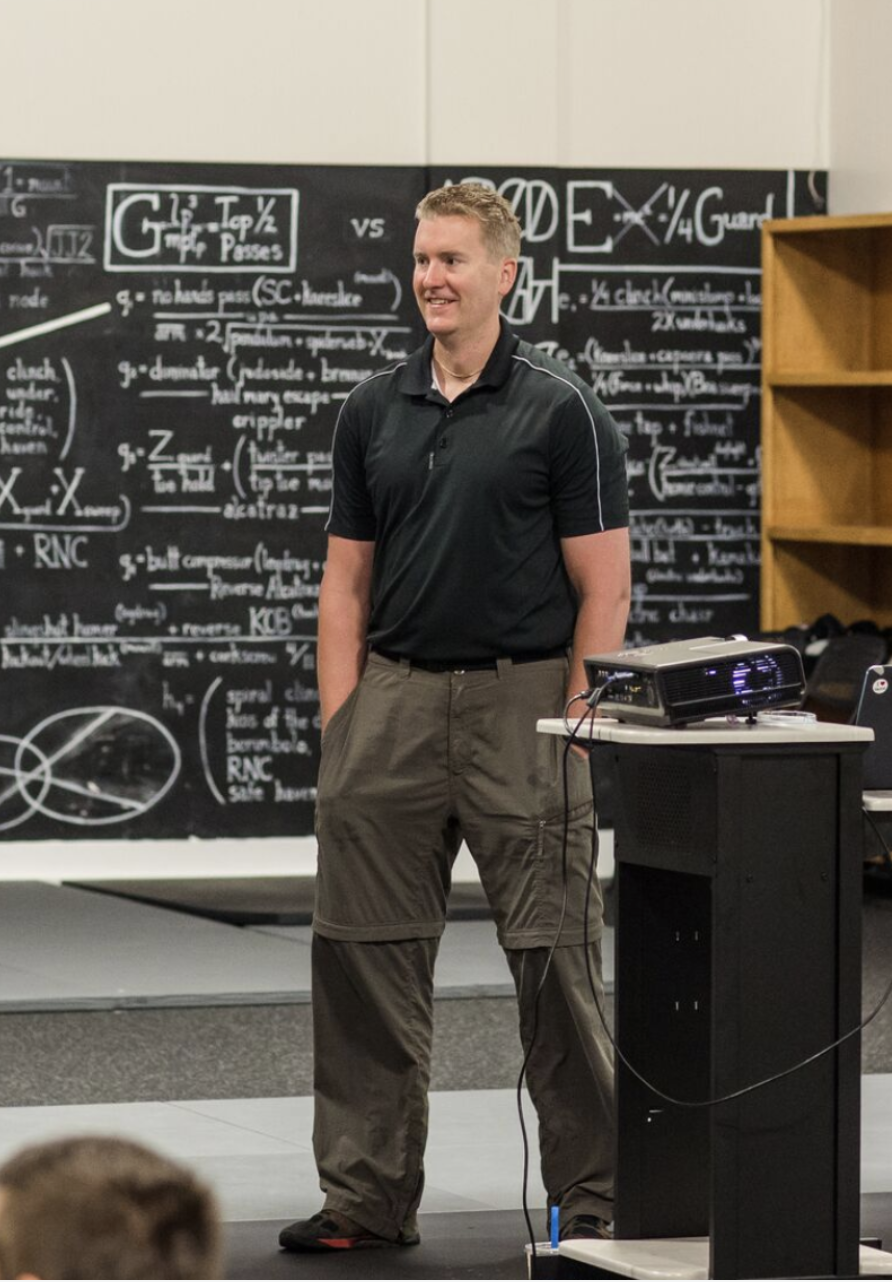
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
[00:00:00] Dr Mike T Nelson: Hey there. Welcome back to the Flex Diet Podcast. On this podcast, we talk all about things to improve body composition, increase performance, add more muscle, do it all without destroying your health, any flexible framework. Today on the podcast, we’ve got Dr. Chris Morrisey, and we’re talking all about GLP one agonists such as Wegovy, Ozempic, et cetera.
And what are some of the pros and the cons from Dr. Chris, who is also a fitness professional and a general surgeon, in addition to a whole bunch of other stuff that he’s doing. So he has a very unique perspective on these medications. I’ll also link to an episode we did with my good friend, Dr. Christa Rimel.
Dr. Morrissey has been on the podcast before, so we’ll link to that also. I think you’ll enjoy this conversation as we talk about some of the pros, some of the cons, what are the risks that he has seen. I also give my public service a plug for what people should do if they’re having symptoms. Go to the hospital, basically get it checked out.
But I think you’ll enjoy this episode. And today we’ve got a sponsorship from Tecton. If you’re looking for something to help with energy, and I especially have been using it in the past with fasting. I find that having one of them in the afternoon during the middle of a longer fast for body comp purposes, when I’m really focusing on body comp, I still do and work up to some longer fasts that I talk about in the flex diet certification.
And I find by adding some ketones, it really helps with this transition. Especially when I’m transitioning back into those longer fasts. So if you’re looking for an exogenous ketone that is an ester form, which means that it’s able to raise your blood levels of ketones higher, check this out. I am biased because I am a scientific advisor there and an ambassador for them, but the taste is actually quite good.
If you’ve tried any of the other exogenous ketones on the market, you know that they do not taste very good at all. Some of the salts can be okay, but they generally don’t get your ketone levels very high. And now there’s also products on the market that are just the free form BHB or beta hydroxybutyrate, and I’m not convinced that those really make it past the gut.
Maybe they have some effect, but right now I’m not really convinced. So as of now, the best form is the ketone ester, which is the form Tecton uses. They bind the BHB, which is the molecule of the ketone itself to glycerol. And that enables it to get past digestion and into the bloodstream where it can be used.
So check them out at the link below. Also include a code where you can save 20%. And then also we’ve got the Flex4 here. Go to MikeTNelson. com forward slash F L E X number four. And in this episode, I asked Dr. Morrissey what his top four recommendations are for people who are using these GLP 1 agonist drugs.
What are some things they should watch out for and things that will allow them to mitigate some of the risks and also improve their results. So you can find that at the link below. That exclusive audio is only at the link, and that also signs you up to the Daily Fitness Insider Newsletter, where you get all sorts of other great information delivered directly to your inbox.
So enjoy this episode with Dr. Chris Morrissey.
[00:03:52] Dr Mike T Nelson: Welcome to the podcast, Doc. How are you doing? Good, man. How are you doing? Good. We were just chatting before we hit record and we’re both complaining about how hot it is to train in the garage when it’s super hot
[00:04:02] Dr Chris Morrissey: out. Yes. Down in Kansas, it’s 100 degrees today, so it’s miserable in the garage. Yeah. Do you find
[00:04:10] Dr Mike T Nelson: that It takes about one to two, two and a half weeks to get used to it.
This baffled me forever. Cause I kept looking back at my notes. Cause I’ve been turning in primarily my garage price now for 14, 14 years. And it took me five years to realize this. And I, one day I looked back and I’m like, Hey, wait a minute. It’s almost like this time of the year. I started thinking like, what the heck’s going on?
Was it travel? No. And so I went back and I historically looked at the temperatures around that time and the humidity. And I realized I’m like, Oh, so the years it would go, probably somewhere where you are, low to moderate temperature, then you get these spikes of sustained days that are hot would just crush me.
And then after a while, you get a little bit more used to it. I wouldn’t say it’s never fun, but it seemed to even out after that.
[00:04:58] Dr Chris Morrissey: Yeah, for sure. Cause like Kansas, it changes all the time. So like July, actually July hasn’t been that bad. It had been the seventies and eighties. Yeah. For a couple of weeks and then this entire week, it’s been 100 and it just sucks.
Cause it just feels like the air is heavy. I went out for a run the other day and I’m like, Oh, it’s fine. And then I swear it climbed 80 degrees. I know it didn’t, but I got done. I couldn’t breathe. And I hadn’t ran that hard. It was just a zone two run, but. And then I looked and I was like, holy shit, it’s 100 degrees out.
This is stupid to even be out here running because it wasn’t that bad when I started. But, yeah it destroys me. I’m much more of a cold. I’d rather layer up and go to the gym and have the barbell be cold than it is. It doesn’t get as cold as Minnesota. But I would much rather train in the cold than the heat, so.
[00:05:40] Dr Mike T Nelson: Yeah, the other part that always kicked my ass, too, is when we would go to Costa Rica. And a couple times I went down there in December and June, which are a little bit warmer. And the time we went down there in June, it was, June was ridiculously hot. And it hadn’t quite got that warm in Minnesota yet.
So, you go from hey, oh, it’s nice and cool here, not bad. To holy shit!
[00:06:02] Dr Chris Morrissey: Yeah, for sure. I’ve never been down there, but I’m sure it can be pretty dang hot.
[00:06:06] Dr Mike T Nelson: Yeah, it’s not bad. Not bad though overall to, complain about going to Costa Rica because of the heat so Yeah, awesome well I wanted to have you on to talk about some of the new crazy medications and Because of your position there as a doctor like some of the things that you’ve seen obviously I’ll link to the podcast We had my good friend dr.
Krista Rimel on here She’s a nurse and has worked with these medications for quite some time, especially with diabetic populations. So she had a very nice perspective over many years. But for people who may not know you, just give us the brief. Background of what you do and then what you’ve been seeing and we’ll go from there.
[00:06:49] Dr Chris Morrissey: Sure So, i’ve been on here once before it’s been quite a while though But yeah, it was a while back. We’ll link to that one too. Yeah, it’s been I don’t know a couple years now probably but My name is chris morrissey. I’m a general surgeon down in winfield, kansas, which It’s about three hours southwest of kansas city and about 45 minutes southeast of wichita And I work in a 25 bed critical access hospital, so not a very big place, but we kind of service a big area.
I’ve been down here for 12 years. I did residency up in Grand Blake, Michigan then moved back to Kansas. I originally, I was born and raised in northwest Kansas. I’m married and I’ve got nine kids, ages ranging from almost 30 down to eight. So there’s always something going on at my house. I can imagine.
Is that just like a zoo? No offense. No. It’s a, it’s controlled chaos. It’s different. I got five boys still at home that are going to be a freshman down to the third grade. So, it’s always something I, I can’t, I wouldn’t change it. I love it. Some days are a little more frustrating than others and boys are very Creative and they fight and just do dumb things sometimes, but they’re great kids.
They like hanging out in the gym with me when I go out to the garage gym. So I have the lucky thing about that, that they’ll come out and train with me. And I’ve been training in my garage for probably six years now built up a garage gym over the last six, seven years or so. But and then, I also have a personal training side hustle.
I don’t have a ton of clients, but I do that on the side just cause I like it. I also teach osteopathic manipulation at the new osteopathic. medical school in Wichita. So I do a lot of, spinal manipulation, I’ve taken some RPR classes, which I love. So I try to incorporate all that into my practice as well.
So, and are you technically a D O is that
[00:08:22] Dr Mike T Nelson: correct?
[00:08:23] Dr Chris Morrissey: Or are you
[00:08:24] Dr Mike T Nelson: Did both? I always forget on that.
[00:08:25] Dr Chris Morrissey: So, yeah, I’m a D O. So Dr. Vastyavati. So we learned spinal manipulation in medical school. So we do, Everything MDs do, we take the same boards same classes, but then we learn spinal manipulation on top of it.
I did an extra fellowship. So I took a year off of school and just did that for a year. So I, I probably would say 15 percent of my practice is manipulation. So I have people come to me just for that. More often than not I do it on family and people I work with, Hey, can you crack my neck?
Sure. Things like that. So, but it’s awesome. It’s a good adjunct to what I do. I’m not going to fix someone’s gallbladder. By doing OMM, but I can help with post op pain and can do some other stuff with that So
[00:09:03] Dr Mike T Nelson: cool as a side note, why do you think more? Physicians are not trained in that.
I understand that it’s a whole I don’t want to say different branch of medicine But it’s a whole different thought process that goes into it but it seems like obviously you have to know what you’re doing, but because physicians have a background in anatomy and physiology and all the medical stuff they take it to me, it doesn’t seem like it would take that much longer to learn it and to get halfway decent at it to help a fair amount of people, especially when you’ve invested that much.
Time and effort into the background, but maybe I’m an incorrect on that.
[00:09:40] Dr Chris Morrissey: No for sure. We usually on average have about, Oh, probably a couple hours of lecture a week and a couple hours of lab a week. So I think it’s about 200 hours of extra just hands on, touching people, doing different things, we, as we do the cracking, we do like soft tissue, muscle energy.
Type of things do a lot of articulatory things, but, and there’s way more DO schools. Now, when I started, there was only about 20. And I bet there’s at least 40 to 50 DO schools now. So there’s actually more, more osteopathic physicians than there ever were probably. But it gets overwhelming and it’s one of those things.
Some people think it’s woo and they doesn’t think it works. I don’t know. There’s people that have different reasons for not doing it, but I would say the stats that I saw last is between eight and 10 percent of all osteopaths actually use it, which I think is sad because it’s something that we can do and some people just don’t feel comfortable.
Some people, depending on what practice they do, they just don’t have time to do it. I just make time and it’s one of those things where It’s like biochem. If you don’t study it, you don’t get it. So you just have to practice outside of class and people, some people just don’t want to, they just want to focus on their grades and they do the calculation med school game of well, this is only worth 3 percent of my grade.
I’m just going to tank this so I can do good in my physiology test or whatever. You know what I mean? So it’s. It’s just different ideas of what, but to me, yeah, I wish everybody did it. Cause it’s just a great thing, but I’m biased, so,
[00:11:01] Dr Mike T Nelson: yeah, it seems like in Canada and Europe, it’s a little bit different.
Like I know some, osteopathic physicians up here that’s literally all they do. And they subspecialty within school where in the U S it sounds like it’s becoming more popular, which I think is good.
[00:11:19] Dr Chris Morrissey: Yeah. And actually, I don’t know about all of Europe, but I know like in England, like if you’re an osteopath, you’re equated to a chiropractor.
You’re not, you can’t practice medicine. You can only do hands on stuff. Whereas in, in the United States, like there’s cardiothoracic surgeons that are DOs and, so you can be any type of physician you want. It’s just a different credentialing, but yeah, in Europe and stuff, you can only, you’re only a bone cracker.
You don’t, I don’t think you can do much else other than that. So. Got it.
[00:11:45] Dr Mike T Nelson: Yeah. And then. Yeah. So tell us more what you’ve seen in your, my little air quotes here your day job regarding the, just in general, what do I do? Yeah. This is a background. What does an average day look like?
[00:11:57] Dr Chris Morrissey: Yeah, sure. So, I so like Monday I’m in the office all day. So basically you’ll see patients at either. Maybe need surgery or they’re there for a follow up or they’re just having big abdominal pain or something So I see people in the office anywhere between 20 to 25 people a day and then I’m in my I have a wound clinic that I’m medical director of also So I see a bunch of different wounds venous insufficiency ulcers arterial diabetics surgical wounds spider bites, whatever then I do a lot of endoscopies, so I do a lot of colonoscopies and a lot of upperscopes.
That’s kind of part of the more common thing that I do. And then I do, acute appendicitis, take out gallbladders. bowel resections do again, a lot of wounds, a lot of abscesses, a lot of skin cancer removals. Kind of bread and butter general surgery is what they call that. So, I don’t do like pancreas or liver.
I don’t do thyroids anymore. I don’t do breast cause we don’t have all the imaging things available to us. So just in the abdominal box minus. The big scary organs, I guess you could say, is what I do. So, and then yeah, then I go teach two half days a week at the medical school, teach a manipulation to first and second year students.
And right now I just school just started back up. So I’m also a preceptor. So the third year students on their rotations come and shadow me for surgery. So I have two medical students with me, actually, I got three right now that they just come and hang out with me and do stuff. So.
[00:13:15] Dr Mike T Nelson: Very cool. Yeah.
And related to the GLP 1 agonist what have you seen from your perspective from, I would say, just anything really, since you have such a wide background?
[00:13:27] Dr Chris Morrissey: Yeah. So, I want to start off by saying, I don’t hate GLP ones. I’m not a complete anti, wacko that I think they’re the worst thing ever, but, cause I really enjoyed the podcast with Krista, is that her name?
Yeah. I really enjoyed that. It was great. And I’ve seen it, been very helpful for people, but for what I do for a living one of the biggest things it does is it severely slows down gastric motility. So basically it makes your stomach so it doesn’t empty. So thus the reason some of the, one of the reasons people lose weight is they just, they feel full and they don’t feel hungry and they don’t eat.
Another thing that it does, it also, makes, the beta cells in the pancreas more sensitive to insulin so they can actually utilize it better. They can also it slows down hepatic gluconeogenesis, so it stops your liver from making new energy. And plus it also, so that’s, Kind of the way that it makes the insulin work better and that people lose weight.
But then the bad thing about that is, for one, so if you come in with acute appendicitis, and you’re on a higher dose of the GLP 1s, then your stomach is so full, huge risk of aspiration pneumonia. After you, once you go to sleep to get intubated for surgery you can’t really, you just can’t have a stomach full of food.
So that makes it a lot riskier for that. Typically, if you come in for a a scheduled case, you have to stop it for at least a week. Some places make you stop it for two weeks. Oh, wow. So that’s pretty long. Yeah, it is. It’s crazy. But, and it’s because I’ve scoped a few people that. We’re still on it and I get in their stomach and they’re just huge and distended and full of food.
So I’ve seen it, firsthand going inside their stomach and saying, Oh my God, there’s food that’s been there for two or three days or something. So that’s one thing that it does. And so we make them stop it. That way it just reduces the risk of that. One of the other mechanisms that it does is so.
I don’t know if you want me to get into the how the gallbladder works and do all that. So your gallbladder is just a big sack that just stores bile, right? So bile is made in the liver. One of the biggest things that it does is it helps break down food that’s higher in fat and also higher in protein.
So, on a normal day. Your gallbladder is full, then you’re, you eat a meal, then from the duodenum, you get a little messenger called CCK or cholecystokinin. So it basically sends a signal to the gallbladder saying, hey, we got a bunch of food here, we need to break it down. So the gallbladder squeezes, a bunch of bile dumps out, starts breaking up the food, and you go about your day, so that’s all fine.
If your gallbladder isn’t working, if you have what’s called biliary dyskinesia, where basically, instead of the gallbladder squeezing, it’s just coughs or like quivers and it doesn’t really do its job. Then you can get bloating, nausea, vomiting, upper abdominal pain, feeling full.
So that’s just the gallbladder itself if it doesn’t work very well. So there’s a test that we can do. So if you’re suspecting gallbladder disease, the first thing we do is an ultrasound, look to see if you have stones in the gallbladder, looking to see if the wall is thick, like indicating an acute inflammation or infection, look to see if the common bile duct is dilated.
Then if that’s normal, but you see still think the gallbladder has a problem. You do what’s called a HIDA scan, which is a nuclear med test. And basically it’s you, they inject you with some dye. It goes up into your biliary tree, lights up the gallbladder, lights up the liver, and then they give you synthetic CCK and they calculate your ejection fraction or how well that your gallbladder squeezes and empties.
And so for whatever reason, the normal number they picked is 35%. So anything greater than 35 percent is considered normal function. Okay. But if it’s less than 35%, then that means your gallbladder doesn’t work well. So in that case, typically we’d recommend gallbladder removal. If you’re having symptoms But the, so back to the GLP 1s, so one of the things that they also do is it blunts CCK from being released.
So then your gallbladder is actually sitting there static and not doing its job. And then they’ve seen over time of people that if they have biliary stasis, meaning the bile is just sitting there not flowing, increases the risk of gallstone formation. So, If it’s making your gallbladder sluggish, it’s making your stomach sluggish, it’s making some of the biliary system not work very well, then my theory is that it’s causing more gallstone formation.
So some of these people I’ve been seeing more gallbladder surgeries, people that are needing their gallbladder out, I’m like, oh yeah, a lot of them are on Ozempic or we’re going to be here at Menjaro. So, now I don’t think anybody gets scans or whatever before to prove that they had gallstones before they may have had them before, but it just makes it more sluggish and make it not work very well.
So I’ve been seeing that. Another thing I’ve seen is in the last six months, we’ve admitted six people alone with pancreatitis and the only common ground I’ve seen in them is they’re all on one of those medications. There’s a long list of causes of pancreatitis. The most common is gallstones or alcohol.
If you go on a big drinker binge, or if you have a lot of gallstones, they can cause, because what happens is, Stone sneaks out of the gallbladder, plugs up the pancreatic duct, gets that angry, then it causes pancreatitis. But these new medications have been shown to do that. All the people that I, because I did a very thorough history and there weren’t any meds that would cause it other than the either Wagovi or Menjaro or Zempik.
They had no gallstones. They weren’t drinkers. They weren’t smokers. They didn’t get bit by scorpion. They, they have all these weird things that can cause pancreatitis. So none of them had it. So again, I’m just postulating. I don’t have 100 percent proof that it was that, but I’m seeing that and, like I said, we have a 25 bed hospital.
So I don’t have the patient population of New York, Chicago, all these big places that may be seeing more of it. I don’t know. And
[00:18:49] Dr Mike T Nelson: pancreatitis can be pretty nasty too, correct?
[00:18:52] Dr Chris Morrissey: Yeah, people can die from it. There’s an old score we used to use called Ranson’s criteria. So basically it’s like a prediction of morbidity, mortality.
It looks at age, how high your blood glucose is like AST, LDH, and then it’s like calcium levels and all that stuff. You gotta do this calculation and the higher the number. the more deadly it can be. But yeah, you can die from pancreatitis. It can be bad news. So, but yeah, I’ve just seen that, since like January, December or January and, only half a year.
And so again, I might be wrong, but I have no other proof, but that was the only thing that to me that I could show that was the cause was that. So, I don’t know. As a
[00:19:30] Dr Mike T Nelson: side note, what are some of the symptoms of pancreatitis? I feel like I need to do a little public service announcement because most guys will put up with horrendous like pain in their gut and not go in and you just need to go in.
Absolutely. It comes better
[00:19:45] Dr Chris Morrissey: from you than me. Yeah, no, for sure. So, so one of the things is you either get like metabagastric pain. So, there’s like kind of three, if you want to nerd out and go back to embryology, there’s three embryologic pain zones of your gut. There’s like the mid pigastric region, the peri umbilical, which is around your belly button, and then the suprapubic, which is above your bladder, and then From embryology, the way the gut develops, you have your foregut, your midgut and your hindgut, people may or may not remember that from biology or anatomy, but so in the foregut, basically it’s going to be esophagus, liver, stomach, gallbladder, pancreas, duodenum, So if you have pain up here, then that can be any of those organs.
So you got to sift through and figure out what the cause is. Midip, or the parambilical is going to be your midgut, which is all your small bowel, your appendix, and the majority of your colon. And then the suprapubic area is your hindgut, which is basically. descending colon sigmoid and upper rectum part.
So based up where they, they’ll have vague abdominal pain right here. And it just feels like someone took a spike and shoved it straight through, right out through their back. That’s the, a big hallmark of that nausea, vomiting, anytime they eat, they just feel sick. They feel bloated.
It’s just horrible pain. So that’s and again, it can be more than pancreatitis, but that’s the main thing. And then, based off history and physical, we’ll order the appropriate imaging, either cat scan or ultrasound and lab work. And then if you get diagnosed with pancreatitis, the big treatment for that.
Number one, remove the offending source. So if it’s gallstones, take the gallbladder out before they go home. Alcohol, you quit drinking medications, you stop the medications and then basically fluids, don’t let them eat or drink and just hurry up and wait for the pain to get better. But it can take a few days.
It can be. It can be in the ICU if it’s really bad, and just flooding them with fluids for days sometimes, so.
[00:21:28] Dr Mike T Nelson: While we’re doing our side note little public service announcement explain where the appendix is, on which side, and Because I think, I’ve had a couple people, not recently, but have had pain in their side and I’m like, isn’t that the side where your appendix is?
Like I think you should go get it checked out. Right. So,
[00:21:47] Dr Chris Morrissey: almost always the appendix is on the right side.
[00:21:50] Dr Mike T Nelson: Right. I know there’s some weird stuff like, even cardiac stuff you can, I saw a case once of dextrocardia where the whole cardiac system was literally flipped and backwards, so to speak.
So, there’s obviously weird. anatomy stuff that can happen.
[00:22:04] Dr Chris Morrissey: Yeah, for sure. So one up from that, it’s called total situs and versus when all of your organs are flipped. So I saw one case of that in residency. It was a 16 year old kid came in with appendicitis, but he had left lower quadrant pain.
And so I looked at his cat scan and we were like, is the patient upside down? Everything’s backwards. And then you’re like, Oh, they’ve got that. So when we went in the abdomen and yeah the livers on the left, the spleens on the right, like everything is mirrored. image and flipped so unless you have that or just one of the other yeah super rare i don’t know less than point something percent The other thing, if you have what’s called a mid gut volvulus, where basically as you’re developing in utero, all your guts herniate up to the belly button and they twist around and they go back inside and then they take up shop where they’re supposed to be.
Sometimes they get inside and they get twisted some, but they don’t go where they’re supposed to be. So all of your small intestines is clear on the right side of your body and your entire colon’s on the left. So instead of the colon framing the abdomen, the colon is all. Over on the left. And so your appendix can be in the left, lower quadrant to seeing that twice.
Otherwise almost always the pains in the right, lower quadrant. So usually it’ll start in the belly button and be just vague and then migrate down to the right, lower quadrant. Get really sharp hurts going over bumps. You have to hunch over to walk depending on where the appendix is located.
So yeah, if it’s right side of pain, like on, it depends on where it is. If it’s on the side that can be like kidney stone or, it could be pancreatitis too, just depends, but. But yeah, right lower quadrant, almost always appendicitis, so, for sure.
[00:23:32] Dr Mike T Nelson: And my last little public service announcement too is that I’ve known two people in the last You’re who all of a sudden had like abdominal pain and went in and I guess part of, I don’t know if it was, I think it was a small intestine, but maybe it was a large intestine got actually twisted and started putting off the blood flow to it.
And both of them had like emergency surgery. Luckily, they both went in like right away when they had just debilitating pain and they were okay. But. That was it. None of them had symptoms beforehand. They’re just walking around all of a sudden they’re like, well, it’s bizarre too, but that
[00:24:07] Dr Chris Morrissey: is, that’s pretty rare too.
Your, your GI tract is one long tube, right? Starts in your mouth and it exits at your anus. And as your bowels are moving, it’s just like a plate of spaghetti. The small intestines in the middle are always moving. And sometimes it just takes the perfect storm of it. Kinks weird.
Things a different way weird blood supplies cut off and then it just gets all swollen and then blood can’t get in blood can’t get out and then the tissue starts to die. On average, you say if you shut off blood supply to something you have about six hours to get in and relieve the obstruction, whatever it is, if there’s a if there’s a clot blocking off the blood flow, if the guts twisted after that, you start having tissue necrosis and the tissue starts to die.
And then you might have to do, depending on how much is involved, a bowery section, take out part of the small bowel, take out part of the colon. And there’s a little side note on that is you can completely live without your colon. You don’t need your colon at all. So if you get a little bit removed or all of it removed you can live without that, but you can’t live without your small bowel.
So if you get so much of your small bowel taken out, you get what’s called short bowel syndrome, where you basically can’t absorb anything. And you’re like on chronic TPN, which is IV nutrition for life. Cause you can’t sustain, you can’t do anything cause you have no nutrients to do anything with it. So, so that’s a big deal.
So some people think. If you lose your colon, Oh my God, it’s terrible. It’s well, it is, you’ll just have diarrhea, but you can live without your colon. So,
[00:25:23] Dr Mike T Nelson: yeah, people may remember John Meadows, rest in peace. So I miss John a lot, but he didn’t have a large colon for many years. And he, obviously had some digestive issues, he was.
It was okay. Otherwise, so yeah Not something that’s high on my list, but definitely something you can still get by with. Yes Keep it if you can
[00:25:44] Dr Chris Morrissey: but
[00:25:44] Dr Mike T Nelson: if you have to get rid of it, it’s not the end of the world Well, thank you for the public service. Oh sure there because I had one case. Oh god, this is probably 11 12 years ago a client texted me And said they were having, lower right abdominal pain.
What should I do? And I’m like, don’t call me. Go to the ER. What are you doing? Texting me, right? That’s fun. Was it appendicitis? I think it was actually. Yeah. Yeah. So luckily they went in. I’m just like, Oh God. Yeah. So you have any medical emergencies, like just go in, get it checked out. Yes, do the thing.
Especially. Most people know when they’re having really bad pain, right? It’s not oh, this might be just a little bit of indigestion. Most of the time you know, and it’s still astonishing to me that some people are like, Oh, it’ll pass. I’m like, bro, you’ve had like blinding pain for six hours now.
That’s just, I don’t know what it is. I’m not a doctor. It’s not normal, but for God’s sakes, get it looked at. Right.
[00:26:45] Dr Chris Morrissey: Yes, for sure. Some people, they go to the ER too much. Some people, every little thing they go in, but yeah, it’s sometimes you get all ends of the spectrum, or someone’s had this growth go for 13 years, and they come in, and it’s like this ginormous thing they want removed, and whatever, so it’s weird what people will put up with sometimes, so.
Yeah, check out my goiter. Yeah.
[00:27:03] Dr Mike T Nelson: Exactly. For sure. Well, back to our topic on hand here. Yeah. Is there any screening that are done for these drugs? I’ve heard everything across the board. I have some friends who are physicians who prescribe them, who seem to be pretty, I would say, good about, who should use them, who should not, describing the pros, describing the cons.
But then, I know of, it seems Clinic spas popping up all over creation where they’re just being handed out. And now I think one of them, I can’t remember an early one is off patent. So you may be able to find it on certain scrupulous, non scrupulous websites. And it just seems like me. It’s all across the board in terms of, Hey, here you go.
Or let’s actually have a discussion about this. Here’s the pros. Here’s the cons. It seems to be all across the board from what I’ve seen on my end.
[00:27:57] Dr Chris Morrissey: Yeah, so I think if physicians are doing it more often than not, and I don’t know a lot of physician friends that are prescribing it, but they usually do a pretty good job at, you want to just do, obviously complete history physical exam.
One of the big red flags is it can lead to medullary thyroid cancer. So if you have a family history of thyroid cancer or. If you have enlarged thyroid or any other symptoms like that, then you may want to be, have second thoughts about maybe prescribing that for people like that. There’s some endocrine like immune syndromes, which is, multiple endocrine neoplasias where they can get different tumors in different places.
So people like that should probably not have it. And again, I don’t prescribe these. I’m just saying what I know. Otherwise, you should get some blood work. Just normal, like complete blood count, checking electrolytes, liver numbers, kidney numbers just to start with to get a baseline.
And then probably, I don’t know what the algorithm is. I know they start off usually 12 and a half units on most of these. Most of them, almost all of them are weekly injection. I think Menjaro’s daily, but I want to Ozempic, I think are weekly. So they’ll start off at 12 and a half and they slowly ramp up.
And, interestingly, I just listened to You’re reposting a podcast. Dr. Andy Galpin and Yeah, I just listened to that and they mentioned it and I think it was Yeah, I think you shot it back in 2021. So some of it was new. It was interesting timing that we were talking about this, but they were talking about it too.
But yeah, you definitely want to get into one of the biggest things you’d want to get a baseline as a hemoglobin a one C, which is like your three month long blood sugar average. And then, cause most of the time, if you’re using it for diabetes, they’re going to be high. And so then you want to recheck that at probably three month intervals, also checking liver numbers and kidney numbers, making sure those are all in check.
And then just check in with them, every so often, again, I would probably do it maybe one month in just to see how things are going. And then probably the three month and a six month, six month mark. And I’ve heard protocols about people will cycle on and off of them. You’d be on it for six months and then you go off of it for a short period of time and then go back on them again.
Yeah. I don’t have, again, I don’t have long term data on that because I don’t prescribe it, but but there’s a lot of places that pop up that you just give it out just because it’s cash, and there’s no follow up, there’s no anything, and that just, that’s one of the things I have problem with for sure.
[00:30:10] Dr Mike T Nelson: Yeah, that, that bugs me with just about anything. It’s yes, especially any medication drug, there is going to be pros and cons. There’s nothing that’s side effect free. Christ, you can die from hyponatremia from drinking too much freaking water. Like you have to try pretty hard to do it, but unfortunately people have done it.
So even water is not without its risks. So do your homework. If you’re going to a physician who is just Hey, here you go, you’ll be fine. Ask some questions, maybe go to a different physician. I wouldn’t say Google that unless you’re trying to Google questions to ask your actual physician. I wouldn’t trust Google for medical advice at all. But it just seems like people want to believe that there, there is no pons to anything. It’s all just pros and I get it. Like I tell people like, just listen to any pharmaceutical commercial. Like it’s all happy. It sounds wonderful. And then if there’s a laundry list of side effects that are most of the commercial.
Again, doesn’t mean that it’s not beneficial. It doesn’t mean that some people can’t benefit from it, but there’s going to be some risks involved too. And so work with someone to make an educated decision instead of, well, I just need to lose 10 pounds. So I’m just going to do this for a couple of weeks.
Probably not the best idea. No, not the best idea. And then also, from a risk perspective, I’m just trying to think. So I won’t say who, but a friend of mine is a nurse anesthetist and she’s seen some surgeries that they’ve actually even had to put out because they go through the list, they ask him, Hey, are you on any medications?
You’re on anything? No. And sometimes they don’t find out till they’re wheeling the person back. Or like you said, sometimes they don’t find out till they’re actually in there. So I guess my last little public service thing here, I feel like I’m lecturing on people, is no, tell your physician and people in the hospital setting like what the hell you’re actually doing.
They’re not going to arrest you, they’re not going to be mad at you, they’re not going to hopefully give you a lecture for an hour about your decisions, but For God’s sakes, tell them what the hell’s going on. It’s my last little public service.
[00:32:29] Dr Chris Morrissey: Yeah. And to counter that is, I’ve started asking in my office, every person, are you on any medicines?
Like I’ll ask about blood thinners. And I asked about GLP ones, just on everybody, colonoscopy, gallbladder surgery, whatever, because some people look at those medicines as supplements. Right. So, you look at their med list and I always, are you still on all these meds and I’ll list them off and then.
I’ll say, are you on any blood thinners? Any aspirin, Plavix, Coumadin, Xeralta or anything? No. And then are you on any of those new weight loss medicines like Wigovi or Manjaro? Oh yeah. I’m on Nozempic. I’m like, okay, so that’s not on your list. And then I have to tell them. Why this important for him to know, but at our place.
So I usually have my nurse, we’ll go in and room the patient and ask some questions. So she always asks. Then I sent a medical student in to do the interview, to get them practice. I make them ask. And so there’s two times of them to tell them. Then I go in and then the day before a surgery are one of our nurses from the hospital calls and they’ll ask anesthesia, asks the day of, and then sometimes it’ll get through to They say no to my nurse, no to my student, no to me, no to the nurse.
The day of surgery they’ll be like, oh yeah, I’m a Plavix to the CRNA. Well, yeah, duh. And it’s well, did you stop it? No, no one told me. It’s four people ask you and you said no every time until the day of surgery. So that happens too. But yeah, there’s, I had a lady I was set up to do an upper scope on, and I asked her about medications, nothing.
The day of, they’re like, we’re cancelling your scope. I’m like, why? Oh, she’s on Ozempic. I was like, didn’t tell me that, and I asked her. You know what I mean? So it’s some people just have no clue what their medicines they’re on. They’re just like, oh, you should have that information. I’m like, well, I do, but I want to make sure that’s right.
Cause sometimes meds change or take them or whatever. So, so yeah it’s a lot of, Hey, help me help you. And yeah I, we do a really good job at asking multiple times and still miss things, I’m sure. But
[00:34:16] Dr Mike T Nelson: yeah. Do you think there’s some variability, like all things between patients in terms of transit time?
Like you may have some people, like you were saying, it seems like they’re pushing out. longer now to potentially accommodate maybe some of those people who are on a higher dose or maybe they’re just Weird hyper responders to it, perhaps.
[00:34:39] Dr Chris Morrissey: Yeah, I think that’s part of it. And, in some people, if they’ve, if they’re really bad diabetics and they can get diabetic gastropathy, where basically their stomach is slow to empty anyway, because of the nerve damage from diabetes.
And so those people may have severely slow emptying times, but we don’t do like a gastric emptying study to see how slow their stomach is beforehand. And so, yeah, I think some comorbidities definitely can make it. Challenging to know how far out. So in general, we just do a week for everybody unless there’s another reason why we have to make it longer.
But but that’s what we’re doing at our hospital, I think, because we get nurse and ethicist students from KU and they rotate with the CRNAs here. And I think they said at KU they do two weeks of the GOP ones. And so, It just depends on where, the protocols are. But on average, I want to say it’s a week here.
So
[00:35:29] Dr Mike T Nelson: what do they do in the case of if someone needs an emergency surgery? Do you just have to work around it at that point and just deal with the lesser of two evils?
[00:35:38] Dr Chris Morrissey: Yeah. So basically, if they have a perfect appendicitis and they have to have an operation, we basically say, Hey, look, you’re on this medication, whether it’s blood thinner, whether it’s you know, Ozympic or whatever, like this is going to make the surgical procedure a little more risky because of this.
And just letting you know that. So if you do end up with aspiration pneumonia, that doesn’t mean we’re just like, have a free pass and do what we want, but we’re just like, Hey, just so you know, because of this you have a higher risk of having this done to you just so you’re aware. For where we’re at, if it’s going to be too risky, like if they’re on three blood thinners and we have a very limited blood bank in my hospital, we don’t have platelets to give if we need to give them platelets.
So sometimes we’ll just ship people out. If it’s too risky and they have to go somewhere else. But yeah, if it’s an emergency, they will die. It’s well, you gotta, again, lesser of two evils and just hope everything goes well. So. Yeah.
[00:36:26] Dr Mike T Nelson: And I think some blood thinners you can reverse in emergency circumstances, but I don’t know of anything that you could.
Reverse any of the GLP ones. You’re just, it is what it is at that point.
[00:36:37] Dr Chris Morrissey: Yeah. To my knowledge, there’s no reversal agent. It’s just, you have to leave it out of your system. And so, six hours is not going to get it out of their system. You’re just stuck dealing with it for sure. So,
[00:36:47] Dr Mike T Nelson: and shifting gears a little bit as obviously you do stuff in the fitness area too, and you have a background with medicine what are your thoughts about from a fitness side?
Some of the risks of. These drugs and i’m thinking more in terms of like habits and in some of the original trials We’ve showed people have had a lean body mass loss and things of that nature.
[00:37:08] Dr Chris Morrissey: Yeah, so It’s a great question because I was wanting to talk about this too. There’s a lot of people around here that are on them.
And you can always tell they get a lot of proximal muscle wasting. So like their shoulders, thighs you can, they just look, they almost look atrophied to me. They’ll, their face looks slimmer and, they’re definitely have lost weight. Their clothes are, different sizes, but you can just tell that they have just a lot of muscle wasting.
And my theory is they just, you’re in a catabolic state all the time. And so you’re not taking in fuel. So let’s just start taking away muscle, like people that are, in third world countries that are starving and they get all catechetic or people that are anorexic, you just start tapping into what fuels you have in your body.
And so I think it’s a big problem. And this is a big reason why I’m against these medicines. For weight loss is because most people aren’t going to They just want the easy button, because you know by nature everyone’s we’re all lazy, right? I mean i’m not saying only people on ozempic are lazy.
Like we’re all lazy We want to do the easy way out your body
[00:38:05] Dr Mike T Nelson: is programmed for efficiency. That’s just how we’re programmed.
[00:38:09] Dr Chris Morrissey: Yeah Absolutely. And conserve energy when you’re not doing anything and expend it for when you need it. But if you I have a problem with it because, all the people come to me, and I want to lose weight.
I want to do all this. I’m like, I, can you prescribe me Ozempic? I’m like, no, I don’t do that for one. I was like, if I will consider doing it for you, it’s you have to show me you’re committed to at least six months of sleep, nutrition, movement, doing all these things, resistance training.
And then if you’re proven, because the medicine doesn’t shift your mindset, it’s not a. You’re not changing habits. You’re just like injecting and can eat still whatever you want. So, that’s why I have a big problem with it. And so I feel that if people are on it, they should be being sent to someone that does personal training, or if the person that prescribes it can do it just so you don’t get the muscle wasting.
Cause I don’t know. I feel if you’re tapping into muscle stores, then if the people are older, maybe they’re getting more osteoporosis, maybe. We’ve seen the bone density increase from resistance training is awesome. So if you’re not resistance training, I think you’re robbing yourself of all of your fuels in your body.
And so, I have a big problem with that, that people don’t want to, but if they’re like, 800 pounds and they just barely can move. I would be for that, say, Hey, this is what our plan is going to be. Maybe give it to him to get them a jumpstart, put them on an off cycle, make them start exercising when they can move better and then they can go back on it.
But they got to show to me, you should show commitment and you’re willing to change instead of just I just want a shot and go to Sonic and whatever,
[00:39:31] Dr Mike T Nelson: do you think people will choose to stay on these medications? I’ve heard that there’s some early literature showing that the average time, I think was six months.
I haven’t. Read that yet. That was from a friend of mine. But do you think people will just choose to stay on because my fear is exactly what you said, bob whose butt looks like a couch cushion Oh, I heard I can just get on old zemp. I can lose weight and on one hand It boggles my mind that we actually have medications that are that Effective that we’re actually worried about crushing your appetite too much If you would have came to me like three years ago and said, you know We’re going to have these new drugs.
They’re literally going to crush people’s appetite so much that they’re going to have all these kind of wasting conditions from it. I would have said, no, you’re crazy. That was, appetite is so redundant and need for energy, all this stuff. And holy crap, like that’s where we’re at now. But do you think people will choose to stay on them?
Because my guess is. They’ll go off. They haven’t made any lifestyle changes. They haven’t really learned anything about what to do differently. Jocker, they’ll probably gain weight because they’re going to eat more. And then maybe they just decide to go back on again. And they’re on this kind of weird yo type thing, but they’re potentially losing a lot more lean body mass as they’re doing it and becoming less functional.
[00:40:54] Dr Chris Morrissey: Yeah, for sure. I think they will. And I think they’ll just, see the results of. That they’ve lost weight so now they’re happy and oh my god, this is awesome. And then they go off it and they a cyclical depression cycle of like I said, binge eating and then they’ll go back on it to lose weight and then over time are they going to be losing a lot more lean muscle mass, like you said, so I feel the people that don’t want to do any lifestyle changes, they’ll just keep doing it as long as people will give it to them, and if they, if the clinic they go to quits doing it, they’ll go find somebody different up the road cause you could, I’m sure you can find anything, anybody to do anything if you keep looking hard enough, so, yeah, I foresee that being a big problem.
And it seems like, my short career as a physician, I’ve been out of residency for 12 years. So I, I’ve been a doctor for 17 years. It seems like every drug that comes out that is awesome, then they pull it later because it has all these problems. So that’s just my prediction. Huh? I was thinking of Fen Phen.
I was thinking of Fen Phen and Vioxx, the big anti inflammatory drug back in the day. Like every drug that’s like the best thing since sliced bread, it always, ends up getting pulled and or you’ll see every other commercial of lawsuits for being on their medication causing problems. So that’s just my prediction.
I’m probably wrong, but it just seems if it’s too good to be true, it usually is. And so, and and also too, I’ve read that they’re, we’re having trouble getting it because so many people are using it for weight loss. And then the people that are diabetics that really need it, can’t get it, or That we’re price gouging so bad because I think in the U.
S., I think an average month is like 1, 500 and then in Europe you can get it for 110 or something. Yeah, I don’t understand that. The U. S. market is just crushing it with price inflation and it’s one more thing that we’re having go wrong here. So, yeah.
[00:42:32] Dr Mike T Nelson: If you were in charge of, say, these drugs and somebody came to you and said, Okay, let’s throw the psychology out the window for now, which again, is a huge topic.
But just based on the physiology and they said, okay, you’re in charge, people are going to request these drugs. What would be your requirements if you were to prescribe them in a perfect world just based on physiology? Are we doing it for weight loss for primarily for weight loss? Because I think that’s, obviously.
Diabetes is a whole sub issue but I think the weight loss is where I’m more concerned because it’s people not necessarily, yes, it’s a medical condition, but I think there’s this huge oncoming flood of people who also just want to lose 10 to 30 pounds.
[00:43:27] Dr Chris Morrissey: Yeah, for sure. So what I would do is I would probably treat them like any of my, either regular, like regular patients or personal training clients, I have this big intake form and make them fill out, goals, what have you tried before, what’s your eating habits, what’s your sleep like, what have you done before, and then I would lay out an algorithm I would calculate based off ideal body weight, not their actual body weight of what their macros need to be, I would set up a nutrition plan, I would set up, mandatory, at least.
Walking five days a week and maybe two days a week to start off with some sort of resistance training, just even getting a gallon of milk and kettlebell swings or curls or something. So I would make them do that. I would make them do weekly check ins. And if we’re in a perfect world where I can do whatever I want and they’ll comply, I wouldn’t give their medication until they show me, either video evidence or a step counter, send me your ORA ring data, send me your, your Garmin data and to show that you’re actually putting in the work and then you can have, here’s your medication to make them compliant because otherwise they’ll just do it.
They’re like, yeah, whatever, just go to an injection. Oh yeah, it worked out. Yeah, I had that go. Oh, it was great. And. Yeah I just, that’s what I would do to ensure compliance because again, I’m for these drugs for the right reason. And, but I, you have to have everything else dialed in just like everybody else says, to make things work, just sleep, nutrition habits, and just, I’m, I got some of my philosophy from you, but I’ve always been big and low and slow, to say, okay, let’s change this one thing.
Let’s just get, start walking. If you don’t do anything else to start walking. Six days a week. And once you’ve done that for three weeks, then we’ll move it up to let’s look at your protein intake or whatever they can do, cause I’m a big believer and that’s helped. A lot of my people that I train is instead of having, okay, you have 10 things to fix by tomorrow.
Cause then they won’t do it. It’s just seems to be the best way to do things. So that’s, that’d be my perfect world thing to do. So nice.
[00:45:10] Dr Mike T Nelson: Do you think there is some other, I wouldn’t say really a side effect, but maybe some other effect on muscle mass directly from these medications, or do you think that they are such a potent anorexic that they’re just crushing appetite so much that Most of the population who is using them are not going to be resistance training or not really going to be consuming much protein.
[00:45:37] Dr Chris Morrissey: I think from what I’m, from what I know, and I haven’t done a deep dive into the nuances of it, but from what I’ve read to me, that just makes sense that it’s just from sheer malnutrition from not eating. I don’t think it’s a, I don’t think the medicines are actually like breaking down your muscle itself.
I think it’s just. Your body needs fuel and I think your body’s doing it. That’s again. That’s my theory I might can be completely wrong but that’s just what I think the problem is you just because again you’re getting big and bloated and distended and You know your hunger mechanism shuts off and you’re like, oh we don’t need to eat and then we start mobilizing that You know secreting more insulin and getting more insulin in the tissue You start burning more fat and then you run out of fat So now you got to go to the muscles or whatever.
So that’s what I think it Is that so
[00:46:20] Dr Mike T Nelson: yeah, I had the idea which this probably wouldn’t work and I definitely couldn’t make any claims on it, but Someone, I’m sure, will do this, and maybe it’s already out there, of the ozempic supplement, and it’s basically just essential amino acids. And all you do is you just mix them in water, because people, even taking protein sometimes for these people can be very difficult.
And even a protein shake, which isn’t really that much, in some cases I’ve seen anecdotally can be too much. Yeah, so I would make it just literally freeform essential amino acids that are like Water and you have to consume it three times per day again. Is this an ideal situation? No, but someone’s probably gonna do that and it probably Would be helpful to some degree versus nothing.
What are your thoughts?
[00:47:12] Dr Chris Morrissey: Yeah, I mean I would think something’s better than nothing, but it’s hard when If you’re like super, you’re like, I am not hungry at all. I don’t know if you’re trying to do in a bulk, and it’s I don’t want to eat anymore. I’m tired of eating, but then making yourself eat, you just probably aren’t going to do it.
So I could just see people being like, if you can’t get them to get up and walk, I don’t think they’re going to force themselves to be like, Oh, I got to drink this stuff again. I’m just not going to do it. You know what I mean? I think it would be helpful. I think some is better than none, but I still don’t think.
Globally, it would probably help much. I’m sure if you’re selling a supplement, yes, you’re going to make these claims that it’s going to, so keep your muscle mass and do all these things. But. I just don’t see a lot of people doing that just because you don’t feel like doing anything. So
[00:47:54] Dr Mike T Nelson: my other thought was that the pharma solution, at least for guys, will just be TRT replacement because like pharmaceuticals tend to think of the solution is always another pharmaceutical.
Oh, so what other pharmaceuticals do we have that are massively anti catabolic, at least in, in men, women’s a whole separate issue. Oh, testosterone. So I just have this weird vision of TRT, ozempia clinics, like popping up everywhere for guys.
[00:48:23] Dr Chris Morrissey: Oh yeah, especially when people are doing like the pellets, they’ll probably start doing more of the pellet stuff just to, sustain, well all that stuff.
And I looked into doing some of that and cause I’m a medical director of a med spa too. And we were looking at, longevity things. And I got on some like endocrinology message boards and went down a couple of rabbit holes and they’re seeing so many things, so many more disease processes than they’ve ever seen before.
Just because of the hormone replacement things when they’re just running just clinics to make money. If you have a true problem, that’s a different story, but I think most of the, I would say a lot of the people that are getting it, the, Oh, I got low test, it’s Probably don’t you just want to legally obtain anabolic steroids and get them in pellet form or whatever but yeah, I just like I don’t want any part of that because It just seemed like it was a just a whole bunch of problems that are evolving that I don’t want to be a part of so
[00:49:12] Dr Mike T Nelson: was that more with the pellets or was that with people going probably above the Physiologic range with testosterone.
[00:49:20] Dr Chris Morrissey: They weren’t like specifying of what they were seeing. It was just in general I was just like because I think I googled I don’t know Endocrinology message boards with hormone replacement. And then I got all these chats with people. I wasn’t like physically chatting, but just all the, Oh, I’m seeing way more.
Thyroid cancers now i’m seeing all these weird metabolic problems and all this and I think the common theme was people being On trt and again not hating on that either. But I just you know Sometimes I think people that are just doing it to do it that aren’t really Don’t slow down and try to calculate what they need and it’s oh, this is the algorithm This is what we’re going to do.
I think that’s where we get into trouble. So yeah, I don’t I didn’t see them specify pellets versus the actual injections or whatever. So i’m not really sure
[00:50:02] Dr Mike T Nelson: Yeah, I feel like Whenever I get that question, I spend most of my time trying to talk guys out of it because it’s usually never the question that I get that’s the person that’s done their homework that probably is legitimately low or they’re getting older, whatever it’s the 28 year old whose testosterone is like 350 and you’re like, bro, you sleep four and a half hours a night, you’re trying to train two hours a day, you’re stressed out of your mind, like You’re chronically under eating, like you barely get enough protein.
Your micronutrition is a disaster. That’s Hey, yeah, I I get it. Like your testosterone was low. That’s not really a
[00:50:38] Dr Chris Morrissey: shocker. Right. And so I feel that’s the same way with the Ozympic. It’s just well, I don’t want to change my stuff. I just want to take this thing and get, so I can feel better and do whatever.
So it’s kinda, it’s a similar theme of, I want to do less work and get more, Things out of it is what it comes down to. I think
[00:50:58] Dr Mike T Nelson: I heard a statistic and I don’t know if this is actually true or not, but I think this class of medications are the most successful pharmaceuticals ever, I believe, like I think total.
Gross was close to a trillion dollars. I think I don’t know if that’s Yeah, glp ones.
[00:51:18] Dr Chris Morrissey: I think I saw that it was like either last I think last year it was like the maybe it was like I don’t know if it’s ever but it was the highest grossing Sales last year. I know for sure but I ever I don’t know. Maybe not ever but
[00:51:31] Dr Mike T Nelson: maybe it was last year is what I was thinking
[00:51:32] Dr Chris Morrissey: yeah, I saw that the other day just because There’s so many clinics popping up, and there’s a couple, there’s people in my town that do it.
There’s people two towns over that do it. And they’re just having so many clients because people are just coming in. They. Charge them 600 bucks. They get a screening of some sort and their first injection and they’re out the door and then they’re getting like 60, 70 new people a week. So yeah, they’re definitely handing it out, whether it’s all needed or whatever is a different story.
But yeah, I would a hundred percent believe that.
[00:52:03] Dr Mike T Nelson: My next thought then, if I was trying to be super optimistic, maybe people are looking for performance enhancement more than ever before, like longevity is becoming a more. popular thing. And on a good day, I keep thinking, well, maybe some of these people will be more vested in their health.
And maybe if they lose some weight, maybe that’s what they need to kickstart their healthy habits and they can exercise more. Maybe they’ll hire a trainer and they’ll do all the wonderful stuff. And then on days I feel really negative, I’m like, no one’s going to have them do that. They’re just going to take drugs.
[00:52:42] Dr Chris Morrissey: I like the optimism in the first thing. I think the second statement’s a little more accurate because, obesity is higher than it’s ever been before. And so, that I just think it’s because, we eat crappy food and we don’t move and social media and screens have killed a lot of things.
You’re seeing, I know when I was a kid, there was only like a couple obese kids and now it seems like they’re everywhere. And the fact that we’re getting softer as a society, it’s, I think there’s just this huge. conundrum that we’re just feeding into the wheel that we’re not helping things.
But yeah, I really feel that, in theory you would think that people would be like, oh, I’ll lose weight, then I’ll start working out. But it’s I lost 50 pounds, I didn’t do anything. Why would I do that? I don’t want to go to gym. I don’t want to do like this extra step. I’ll just, Keep taking these shots, so, it’s the easiest way out for sure.
[00:53:26] Dr Mike T Nelson: Yeah, my negative days, that’s what I keep thinking is that humans are so programmed for efficiency. And when something works, it’s easy to, I think, sweep the costs under the rug. So one of the little things I had on my checklist is if you’re prescribing ozempic, like you have to do DEXA scans on all your patients.
Yeah. Yeah. Right. So you have to physically show them, okay, here’s where you started. Hey, this is great. Like you lost 20 percent body fat. Oh, by the way, 40 percent of that was lean body mass. Like to me, it should be some type of requirement that you should inform people of what’s actually going on in their physiology.
[00:54:11] Dr Chris Morrissey: Yeah, for sure. And you might tell people that don’t work out, that they don’t care about their losing muscle mass. Well, I don’t want to get big. I can see them doing that and they don’t care, but they. They don’t realize that how much how important that is for, just well being that It’s just like I don’t care.
Whatever. It’s weights weight, it doesn’t matter So yeah, I think that’s that’d be a great idea is the dexa scan thing for sure So because I
[00:54:33] Dr Mike T Nelson: think there’s something empowering about seeing your own data versus somebody telling you what’s going to happen or what even did happen like I use this hrv all the time.
Like I used to have before the hrv Oh my god, I don’t know how many Discussions about stress I would have with people And now I’m just like, Hey, look at this. And it’s a little, thing that shows their stress going off a cliff. I just graph it and send them a picture and go, what do you think’s going on?
And they’re like, Oh my God, I didn’t realize I was that stressed. And from the outside, it’s easier to see them when you’re experiencing it. So I think using data, hopefully in something like that might be useful to better inform people again, about what are the pros and what are the cons.
[00:55:18] Dr Chris Morrissey: Oh yeah, absolutely.
I’m huge on, if I have personal training clients, I make them do measurements of arms, hips, thighs, and then weight and then they weigh every week and then I have them do it again after three months and do a little maxing out depending on if it’s weight or just body weight stuff.
But just to show them, cause they may say, Oh, I don’t think I’m doing anything. It’s You’ve lost like 25 pounds in three months and your lifts have gone up and all this so they just don’t see it because they just look at themselves every day and they don’t feel different but it’s so you can objectively show them that yeah you made huge improvements and just like with the weight loss thing you know yeah before and after pictures or DEXA scans or calipers or whatever you want to use at least to show them they’re making progress and hey this is how we need to tweak this and always you know, changing, that’s okay.
Let’s start adding more resistance training because you’re starting to lose more body mass or whatever. And then if they decide they don’t want to do that, then to me, if it was my patient, be like, all right, well, you can go find a different provider if you’re not going to put in the extra work, because I don’t want to just give you meds to do nothing.
So, yeah.
[00:56:15] Dr Mike T Nelson: Awesome. Yeah. And last question, unrelated any good music you’ve been listening to? Side note, did you see Gojira at the Olympics, which is pretty phenomenal. I did not
[00:56:26] Dr Chris Morrissey: see that, I had to watch it
[00:56:27] Dr Mike T Nelson: on video, so.
[00:56:28] Dr Chris Morrissey: I haven’t seen that, but but I heard that they were there and I heard it was awesome.
Yeah, lately I’ve been on a deathcore kick, so I’ve been doing like Slaughter to Prevail. Oh yeah. Upon a Burning Body, Skinless. So that’s been my, I don’t know, last two or three months. That’s been on my, my go to. I’ll just get on Apple music and hit one of those stations and just listen to that all the time.
So that’s what I’ve been, that’s been my jam lately. So
[00:56:52] Dr Mike T Nelson: yeah, the guest vocals he did on the what was it? I want to say it was a falling in reverse with tech nine. The, I can’t remember Ronald was the name of the song.
[00:57:03] Dr Chris Morrissey: Yeah, I heard that. That was one of
[00:57:06] Dr Mike T Nelson: my new favorites. And the new. body song with a lot of the clean vocals and stuff in it.
I think it’s a ghost. That’s one of my new favorite songs. It’s just such an awesome song.
[00:57:16] Dr Chris Morrissey: I don’t know if I’ve listened to that one yet, but I’ll have to, all the early stuff is
[00:57:19] Dr Mike T Nelson: great too.
[00:57:21] Dr Chris Morrissey: I just, those are some, they sound similar. I know they’re different, but I’m not as good at like back in the day, I can tell you album.
Artist song, but nowadays I just don’t care as much. And so I just hit one of their, I’ll just put shuffle and I just listen to them. And so I don’t, I couldn’t tell you, Oh, this is on this album. I can do that with Iron Maiden, Slayer, Pantera, all that from back in the day. But all the new stuff, I just like the sound.
So I don’t, I couldn’t tell you what’s on what, but there’s some really good ones though that I’ve heard lately. So
[00:57:49] Dr Mike T Nelson: nice.
[00:57:50] Dr Chris Morrissey: Yeah, for
[00:57:51] Dr Mike T Nelson: sure. What about you? Oh man the new Mushroomhead sounds interesting. I’ve only heard two tracks so far. We’re going to see Metallica coming up here in a couple weeks with Five Finger Death Punch and Pantera.
Really? That’s gonna be pretty awesome. My god. Yeah, I’m so excited. I did get tickets to see Lorna Shore. They’re headlining at the Fillmore, which is a very small venue. And I was so bummed because initially tickets went on sale and they sold out like instantly and basically a bunch of scalpers bought most of the tickets.
And so the battle was actually super cool. So they were able to acquire some more tickets. So they tried to release them in more random, sporadic stints to prevent people from scalping them because they were reselling them for 450 a ticket. I was like, what? I’m like, I’m not paying that. No, I got tickets to see them.
They’re playing with like a no Sonia Suga bog and a Kublai Khan. And there’s two other bands that are too. It’s already pretty good. The new Kublai Khan is actually really good. If you haven’t really checked that out. Yeah, they’re pretty good. I’ve listened
[00:58:53] Dr Chris Morrissey: to Kublai Khan. I don’t know if I’ve heard the new one yet, but that’s cool.
I don’t go to concerts that much. I just, we get some good stuff here, but I saw falling in reverse. I think it was two years ago. I saw Xem Papa Roach, and Hollywood Undead. That was a good show. Yeah, it was good. And then the one before that, I think I saw Godsmack and Hailstorm. They were really good.
But yeah, I just don’t get to go to shows much. We don’t get much down. Closest thing is probably big shows would be Kansas City. I just don’t get away to go, so. Yeah.
[00:59:24] Dr Mike T Nelson: That’s understandable. Yeah. Awesome. So where can people find out more about you? Best website. And I know you’ve got some cool wrist wraps and all sorts of stuff going on.
[00:59:33] Dr Chris Morrissey: Yeah, for sure. So, I’m on Instagram I try to put out a little videos about every day. How’s that going? It’s okay. Bad time. The only reason I did that was just to get a different audience for marketing my wrist wrap product that I created. That is the only reason I am not a Social media person, but yeah, I’m on TOK.
Both of them are the Morrissey movement 33. And I do have a website, my fitness company is called M nine maximum performance. So in my next performance. com and then my wrist straps that I created therefore track so you can leave on your wristwatch, but you give you still give you good support for.
And so those are on Amazon. I launched back in March and I’ve sold 111 as of today. Oh, that’s actually
[01:00:18] Dr Mike T Nelson: pretty
[01:00:18] Dr Chris Morrissey: good for
[01:00:18] Dr Mike T Nelson: just launching on
[01:00:19] Dr Chris Morrissey: Amazon. Yeah, it’s not too bad. I have a TikTok shop. No one’s bought it. I think I’ve sold one thing off there once. So I have 200 sitting in my house. If anybody wants to buy my TikTok shop, I’ll, Ship them to you from my house, but yeah, it’s going good.
So, I’ve I’m just slowly building the business. I got a guy that I’m working with. It’s making ads for me and doing the Amazon tweak things. I don’t know. Think about, so sales are slowly starting to go up and then I’ll release a couple other products, hopefully by next year, once these take off. So all focused around split route designs.
You can keep your watch on and track your heart rate and your reps and all that stuff. So. Cool. And how do they find that on Amazon? What do they look for? So you can either do just M9 maximum performance. You can do split wrist straps and you should be able to find them. There’s, I’m the only, that’s the only one on the market actually.
So there’s that I was first to market on that, which I was excited about. But but yeah, so you can get them on there. They’re 29. 99 for on sale there. So, that’s what we had a little prime day sale, but that’s over with. So only had probably seven or eight sales on prime day, which wasn’t bad.
[01:01:18] Dr Mike T Nelson: Well, it’s not bad though.
[01:01:19] Dr Chris Morrissey: Yeah, for sure.
[01:01:21] Dr Mike T Nelson: Cool. Awesome. Well, thank you so much for all your time here. I’d encourage everyone to check out all the great stuff you’ve got going on. I know you’ve got a lot of stuff on Instagram, a fair amount, and appreciate all the good info and thank you for sharing all your knowledge here.
Really appreciate it. You bet. Thanks a lot. Awesome. Thank you, sir. You bet. Thank you.
Good.
Thank you so much for listening to the podcast, we really appreciate it. Big thanks to Tekton, make sure to check them out if you’re looking for a tasty ketone ester. Highly recommend you check them out. Yes, I am biased because I’m an ambassador and scientific advisor to them.
We’ve got some great studies that are underway, a lot of work in the background to show that I believe this form of the ketone molecule is better, and you’ll notice right away that it doesn’t taste horrible. It actually tastes pretty good. Again, everybody’s tastes are gonna be a little bit different, but Overall, I actually quite enjoy it, which I can’t really say that much about any other ketone ester.
And then also check out the Flex four. Go to miketnelson.com/flex4 four for my top four things I got from Dr. Chris Morrisey about the use of GP one Agonist also puts you on to the Daily Fitness Insider Newsletter. And if you find someone who might enjoy this podcast, please forward it to them or share it on the old social media.
Make sure to tag me so I can say a big thank you. And if you have time to tickle the old algorithms, give us some stars, whatever you feel were appropriate, or if you can even leave a review, those go a huge way to help the podcast move up in the rankings and keep us getting wonderful guests that we can bring to you.
Thank you so much for listening to the podcast as always. Really appreciate it. Talk to all of you next week.
This podcast is for informational purposes only. The podcast is not intended as a substitute for professional medical advice, diagnosis, or treatment. You should not use the information on the podcast for diagnosing or treating a health problem or disease or prescribing any medication or other treatment.
Always seek the advice of your physician or other qualified health provider before taking any medication. Or nutritional supplement. And with any questions you may have regarding a medical condition, never disregard professional medical advice or delay in seeking it because of something you have heard on this or any other podcast reliance on the podcast is solely at your own risk information provided on the podcast does not create a doctor patient relationship between you and any of the health professionals affiliated with our podcast.
Information and statements regarding dietary supplements are not intended to diagnose, treat, cure, or prevent any disease. Opinions of guests are their own, and this podcast does not endorse or accept responsibility for statements made by guests. This podcast does not make any representations or warranties about guest qualifications or credibility.
Individuals on this podcast may have a direct or indirect financial interest in products or services referred to therein. If you think you have a medical problem, consult a licensed physician.






Leave A Comment