Join me, Dr. Mike T. Nelson, on the Flex Diet Podcast this week with Dr. Jonathan Chung, an expert in chiropractic neurology and upper cervical care, to explore the intricate world of breathwork. This episode dives deep into the neurology of breathing, heart rate variability (HRV), and recovery techniques.
Learn about various breathing practices, including HRV biofeedback, resonance frequency breathing, and the Wim Hof method, and discover how they can improve cognitive and physical performance, manage anxiety, and enhance CO2 tolerance.
Dr. Chung also shares his personal journey and practical advice on selecting breathwork methods tailored to individual needs, emphasizing the balance between parasympathetic and sympathetic responses. We touch on advanced topics like hypoxia training, hyperbaric oxygen therapy (HBOT), and their applications in clinical and athletic settings.
Sponsors:
- Tecton Life Ketone drink! https://tectonlife.com/ DRMIKE to save 20%
- Dr. Mike’s Fitness Insider Newsletter: Sign up for free here.
Flex 4: Dr Chung’s top 4 breathwork takeaways
Episode Chapters:
-
00:29 Guest Introduction: Dr. Jonathan Chung
- 01:08 Promotions and Announcements
- 02:11 Deep Dive into Breathing and HRV
- 04:59 Dr. Chong’s Personal Health Journey
- 10:17 Breathwork Techniques and Benefits
- 17:23 Advanced Breathwork and Clinical Applications
- 27:04 Exploring Hypoxic Training
- 30:56 Exploring Hyperoxia and Hypoxia Training
- 33:23 Hyperbaric Oxygen Therapy: Clinical vs. Athletic Use
- 38:10 CO2 Tolerance and Breathwork Techniques
- 42:23 Breathwork for Anxiety and Performance
- 48:59 Advanced Breathwork Practices and Applications
- 53:19 Final Thoughts and Recommendations
Flex Diet Podcast Episodes You May Enjoy:
-
Episode 215: Breathing, Heart Rate, and HRV: An Interview with Dr. Scotty Butcher, The Strength Jedi
-
Episode 245: Breath, Endurance, and the Art of Athletic Longevity with Bo Sandoval
Connect with Dr Chung:
Get In Touch with Dr Mike:
Rock on!

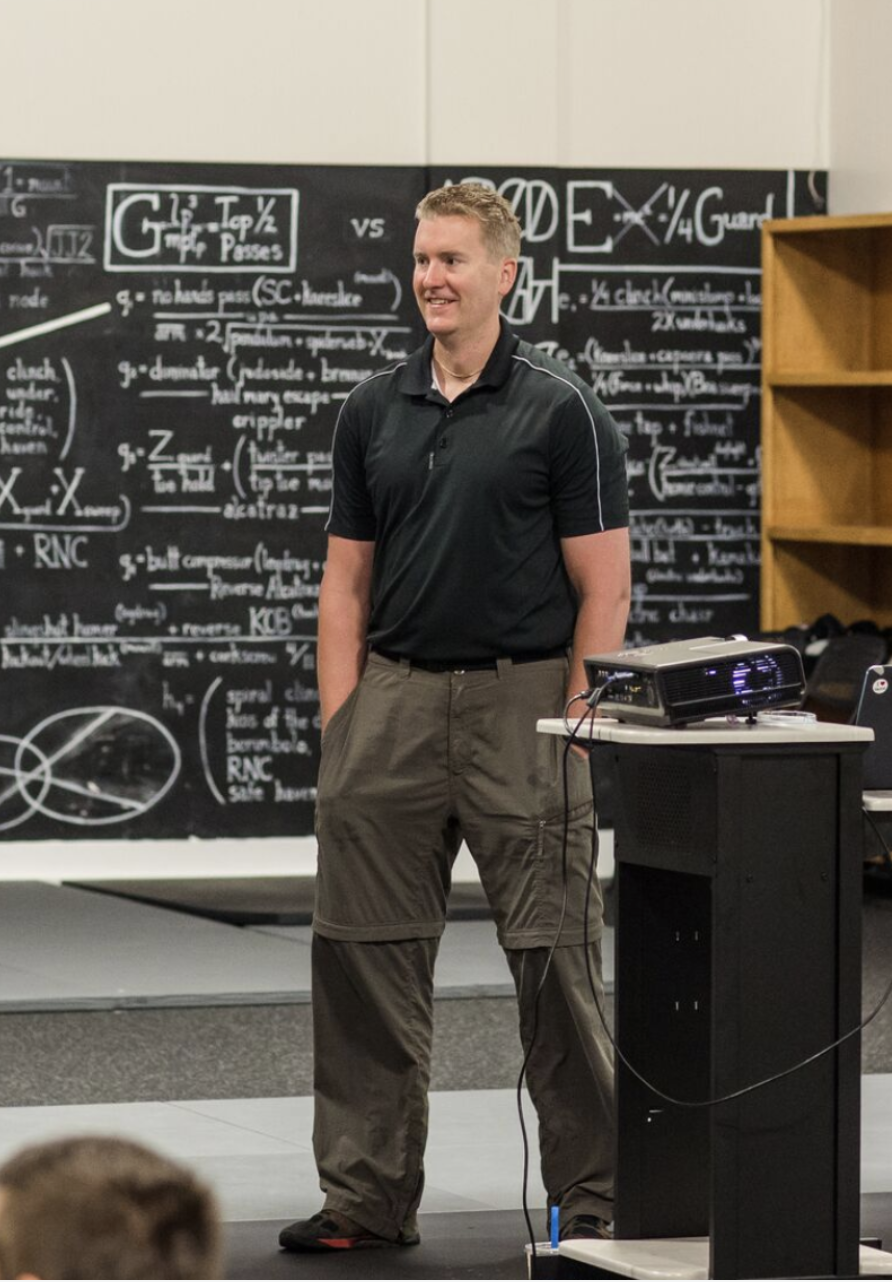
Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
[00:00:00] Hey, what’s going on? Dr. Mike T. Nelson here. Welcome back to the Flex Diet Podcast. And on this podcast, we talk about all things to increase muscle performance, improve body composition, and do it all without destroying your health in the process. You can tell my voice is a little bit trashed right now.
[00:00:21] I’ve been doing a ton of presentations for the Carrick Institute here, and I’ve Slowly recovering my voice again. So today on the podcast, speaking of the Carrick Institute I am an associate professor there. They do a lot of great functional neurology, clinical neurology stuff. We’ve got my buddy from there, Dr.
[00:00:41] Jonathan Chong, and we’re talking all about the neurology of breathing. And this is going to be great. You can find him on Instagram as the anti fragile Cairo. So. Perfect name there. We’ll put a link to his coursework through the Carrick Institute. Again, I am a faculty there, but I don’t make any money off of the course, but I would highly recommend you check it out.
[00:01:06] It’s really, really good. And speaking of coursework, we still have the PhysFlex certification is open. If you want to know about how to increase your body’s ability to recover, be more anti fragile, everything from pH changes. temp changes, expanded fuels, ketones, lactate, breathing, all that kind of stuff.
[00:01:29] You can go to the link below and you can still get in up until this coming Monday night at midnight Pacific Standard Time, which is October 21st, 2024. If you are interested, go there now. Right now, this is the last time it’s going to be open this year. It will be open again, probably Q2 of next year.
[00:01:52] The FlexiDiet cert will open again in January of next year. So this is your last chance for this coming year to go to the link below. And if you have any questions, hit me up and enjoy this great chat here about all things breathing. How does it affect your nervous system? We talk a little bit about heart rate variability.
[00:02:16] Hopefully you listened to the great podcast we did with Joel Jameson on HRV. And the good doctor here gives us a very nice breathing tip you can use also for recovery. The one thing I will plug is that after a heavy training session, whatever you can do to get back to a parasympathetic state, while the research on there is split and we don’t have a ton of direct research I do believe from talking to him, my good buddy Dr.
[00:02:47] Andy Galpin, Ben Pekulski, a lot of these other guys, that getting back to a parasympathetic state as soon as you can after training, I do find is very beneficial. I’ve seen better HRV scores in myself the next day and my clients. And so you can use some of these breathing techniques here as a way to do that also.
[00:03:09] And again, we go way deep on this in the PhysFlexCert also. And he’s got a great course here through the Carrick Institute also with a link to that below. So enjoy this wide ranging talk about the neurology of breathing and much more with Dr. Jonathan Chung.
[00:03:30] [00:03:30] Dr Mike T Nelson: Welcome back to the podcast.
[00:03:32] How are you today, doctor?
[00:03:34] Dr Jonathan Chung: I’m doing great. Mike, how’s it going?
[00:03:36] Dr Mike T Nelson: Good. Good. I thought today would be a cool topic would be the neurology of breathing. And obviously you work at your own clinic there. So just give us the, kind of the 30 second overview of what you do. And then also you have an entire course for the Carrick Institute.
[00:03:54] That’s more around respiration and different aspects of neurology also that we’ll get into.
[00:04:00] Dr Jonathan Chung: Yeah, so I’m a chiropractor by training. I’m an upper cervical chiropractor and I also do chiropractic neurology. So a lot of my practice is focused in on treating neurological conditions, mainly with a big focus on vestibular disorders traumatic brain injury.
[00:04:15] I also see a lot of dysautonomia. So, the dysautonomia aspect was one of the big reasons why I had been really into heart rate variability and really getting into breath work. But my path into breath work and taking it more seriously actually came a lot out of some of my own personal experience after recovering from pretty significant abdominal surgery a few years back.
[00:04:39] Dr Mike T Nelson: Very cool. And where is your clinic located for people who might be local listening to this?
[00:04:45] Dr Jonathan Chung: I’m in the West Palm Beach area, so I’m in a little suburb town called Wellington, the kind of horse country, so we see a lot of equestrians, so we get a lot of equestrians that follow up horses and have some issues related to that.
[00:04:58] Dr Mike T Nelson: Got it. And just tell us a little bit more about what you had with the abdominal stuff and how that kind of parlayed into your deep dive into breathing.
[00:05:08] Dr Jonathan Chung: Yeah, so pretty much since I was a teenager, it had. Random bouts of pretty severe abdominal pain, so I would have these attacks of stomach pain that would last, for hours, and then it would just spontaneously go away, like originally thought it was just like acute gastritis.
[00:05:26] Because it was happening pretty infrequently, like maybe once or twice a year, it would happen. About five or six years ago, the frequency of these stomach attacks were happening more frequently. So I started getting them once every few months. And then in 2022, it got to a point where I was getting affected by it about once per month.
[00:05:46] So once a month, I would just be completely wiped out for a day. And it had even happened once when I was taking the pain reset course at the Carrick Institute, and that was a particularly bad one, and the following month after that, I had the worst stomach pain I had ever had, and I’d been seeing a GI doctor and a GI surgeon.
[00:06:07] And they couldn’t find anything on MRIs or CT scans. And my GI doc was pretty convinced that I had bowel obstruction somewhere, but she couldn’t find any evidence of that on imaging. And there was this little tiny little lesion on my appendix called a mucocele. And they didn’t think that it was causing my abdominal pain, they thought that there was a risk factor for having a ruptured appendix.
[00:06:35] So I said, at a certain point, you may want to consider getting this out. While we take it out, then we may want to consider just doing exploratory surgery and just see, assess the rest of your bowel to see if there’s anything that could be causing your stomach pain. And on that last episode, the pain was so bad that my doctor was just like, listen, why don’t we just go in, let’s take the appendix out.
[00:06:56] We’ll do an exploratory surgery while we’re in there and see what’s going on. And I just had a breaking point was, all right, let’s just go ahead and do it. So they went in, they did the surgery. When they took the appendix out, they actually found that there was within just the mucofield, it was actually a tumor that was wrapped around by distal small bowel and wrapped around by cecum.
[00:07:17] So they pretty much did an ileo psychotomy where they took off like, Two or three inches of my bowels and so getting back up, I woke up thinking that I was going to, leave the hospital that day for an appendix surgery. Said, well, no, we did a full open surgery on you. You’re going to be in here for three or four days.
[00:07:37] So obviously with that, like I’m on pretty heavy IV antibiotics during that time period. I was happy with I was able to recover and bounce back pretty quickly. So I left the hospital in three days. And during that time period the first time in my life since I’d been, pretty active in my teenage years playing baseball, playing sports, where the doctor’s like, all right, well, you can’t really exercise for at least the next four to six weeks while you recover from this.
[00:08:03] Wow I’d never been, like, forced to not exercise for that length of time before, so during that phase, I was like, alright, what are things that I can do, and one of the things that they did encourage people to do, not necessarily for autonomic reasons, but just for physical activity and pneumonia prevention is like, they encourage people to do breathwork while they’re in the hospital.
[00:08:25] So I started to do breathwork practices and I would do it for, five or six minutes while I was in the hospital. But then I’d read about HRV biofeedback breathing and I’d read about, all these different types of yogic breathing techniques. So I decided I would substitute a lot of the time that I would spend exercising and replace it.
[00:08:45] At least in some way with breathwork training So there were days when I was recovering from surgery where I would spend 15 20 minutes just doing resonance frequency breathing for that 15 to 20 minutes at a time and one of the cool things that I saw during that time period was like my hrv from an rmssd level was At the time that before I had surgery was consistently about 80 85 or so
[00:09:10] That’s pretty
[00:09:11] Dr Jonathan Chung: good Yeah, it was really good.
[00:09:13] But before then, when I was in my twenties, before I had kids, I was consistently at about a hundred or so. And during this time period where I was recovering from my surgery after four weeks of, dedicated rest time and recovery and doing the breath work, I actually was past my previous baseline.
[00:09:29] I was back into 100 RMSSD pretty consistently when I was doing the breath work practice on a daily basis. Daily basis wow this is something that like, this is like an untapped thing. I just never really dug fully into that kind of led me down this rabbit hole, really exploring a lot of the neuroscience and a lot of clinical evidence for breathwork practices.
[00:09:52] Dr Mike T Nelson: Awesome. I was going to make a joke about you leaving Dr. Adams course early, but it sounds like you had a valid reason to walk out of the pain reset course.
[00:10:02] Dr Jonathan Chung: Yeah. And that one, I was keeled over for mainly the the last day I was just like, I was completely wiped out. I was in that hoodie and I just covered my face with the hoodie while I was trying to bear through it.
[00:10:17] Dr Mike T Nelson: So can you explain what resonant breathing is for people? And I’m just curious, do you use technology for it? Is it like a heart math type thing or tell us more about what that specific technique is?
[00:10:30] Dr Jonathan Chung: Yeah, so resonance frequency breathing is a breathwork concept and technique that is based on trying to synchronize your cardiac and respiratory rhythms.
[00:10:42] And a lot of evidence suggests that the respiratory frequency syncs with your baroreflex and some of the other neurologic aspects that contribute to breathing at a frequency of four and a half to six and a half breaths, six and a half breaths per minute. And Using tools like heart math, you could actually measure what your ideal resident frequency is, and it’s usually going to be somewhere in that range.
[00:11:10] When I’m educating patients, you’re usually going to target about six breaths per minute. It might be a little bit faster. It might maybe a little bit slower than that, but that’s the target that we’re looking at. If you want to use technology for it heart math is a great one that has, had market share for.
[00:11:27] That type of thing for a while, but the tool that I used was the HRV for biofeedback app which is made by Marco Altini and the who created HRV for training. So I was using that basically to set my resonance frequency, which mine was right at that six breaths per minute mark. And that’s the rate that I’ll take it and that’s where I find works pretty well for many of the patients that I recommended for and they’ll hover right around that six breaths per minute rate.
[00:11:57] Dr Mike T Nelson: And I haven’t seen Marco’s program on that. Obviously I’ve seen his other stuff. He did a lot of great stuff with HRV. He’s been doing it for quite a while. Like I said, the app HRV for training, which was one of the first ones to use the camera app, which I know early on, I was pretty hypercritical of, but to his credit, like he’s done the work on it and published a bunch of cool research and everything else on it, which is awesome to see.
[00:12:20] Is it similar to the heart math, like the heart math one you had, I think it was using the ear clip and it would tell you breathe faster, slower, and you had this little kind of oscillating thing you’re trying to get between. So if you’re using his app, how exactly does that work? And then if you don’t use an app, how would you know what your breath rate should be?
[00:12:40] Or do you just go with six breaths per minute?
[00:12:43] Dr Jonathan Chung: So with his app there are, there’s a couple of settings on the app. There will be a setting where you could like just test your HRV and find your baseline. And then they have the option to change the breath rate and you can measure what your HRV at those different breath paces are.
[00:12:57] It’s a little bit less intuitive than something like HeartMath, but it’s there if you don’t want to buy extra technology for it, then you can just use your camera phone and you can use that as a way to figure out what your resonance frequency is going to be. And for basic purposes for most people I identify, are these people kind of tech savvy and they are going to use tech in a way that is advantageous for them and it’s going to encourage them to do the breadth work and that will encourage them to get the app.
[00:13:26] If I sense that someone might be a little bit, they’ll read too much into the numbers, they’ll get hyper focused on that instead of trying to get what the overarching benefit is, then I’ll actually say, there’s apps for this, but I actually discourage you from using an app. And I’m just going to say, let’s target six breaths per minute for the time being.
[00:13:45] And we could just find a breath pace that feels the most comfortable for you. And we’ll try and pace that’s maybe a little bit faster. We might try and pace that’s a little bit slower. We just want to find that happy spot where you feel the best at that pace. And then whatever that is, then we’ll do that one and we’ll recommend that one for you when you’re trying to do some of the breathwork practice at home.
[00:14:07] So that’s how I guide patients from a clinical perspective when I don’t really want them using the technology, but I know there’s some people, myself included, where I’m positively motivated by, hitting a specific score or being motivated by technology. So if it’s someone like me, then I’m going to encourage them to get the app because Provide that extra layer of accountability that’s helpful for them to actually get the work done.
[00:14:29] But if I see someone is one of the things we’ll see nowadays is people get way too attached to their sleep score. People get way too attached to their recovery scores and without really good reason. So if I see someone that shows elements of that, those personality traits, I’ll discourage them from doing that and try to get them to into it, what feels best for them.
[00:14:49] Dr Mike T Nelson: And if they’re doing it on their own without technology, do you just have them count like in their head? Do you have them try to look at a timer of any sort or you just don’t want them to use any technology at all and just count and get close?
[00:15:03] Dr Jonathan Chung: just counting it close. So I just want them to just count in their head and go based off that.
[00:15:09] And I’ll just set a timer for them. If I’m working with them in the office, then I’ll have a timer. So I’m monitoring while they’re going through that. I’ll provide them like some guided affirmations and things like that to just go through their head while they’re doing it. So if there’s someone that, they get a little bit restless without Some kind of background noise, and I’ll talk them through some of these things if they are fine with silence, and I’ll just have them just, get into some of these interoceptive practices where they’re just really counting their breath and monitoring their heart rate and I’ll tell them, give them guidance on like when you every time that you take a breath in, you may feel that your heart rate is speeding up a little bit.
[00:15:46] And every time you hold that breath out, especially once you hold it a little bit longer than feels a little bit comfortable, you may actually feel that your heart rate actually slows down a bit. I just want them to feel what’s going on inside of their body while they’re going through that practice as a way to encourage the use of some of these interoceptive circuits inside of the brain.
[00:16:07] Dr Mike T Nelson: Have you recorded a script at all for that? That’d be interesting if you had a like kind of what the Huberman did with the NSDR yoga nidra of Hey, here’s a five minute script. Here’s a 10 minute script. Here’s a 20 minute script. Someone just puts it on and listens to it with your kind of, different cues as they’re going through it.
[00:16:28] Dr Jonathan Chung: I haven’t done that, but that’d be something interesting, but together I’m usually just, treating it like I’m having a conversation with the patient while I’m going through it. So. Every patient I end up doing a little bit differently, but there’s probably mechanics of it that I can probably record if I need to do
[00:16:43] Dr Mike T Nelson: Yeah I think they’ll become interesting because I know that’s one of the and I still have this issue of doing some breath work without any sort of cueing it’s easy to veer off into so if I’m doing like a Zen style meditation where you’re just going to sit and stare at a tree and that type of thing outside, you’re monitoring your thoughts, but you’re trying not to be attached to your thoughts.
[00:17:06] And it’s still, even after how many years of doing this, it’s still very easy to realize, Oh, I just spent the last two minutes like following all these rabbit trails down and Oh, no, back on task. Yeah, sure.
[00:17:18] Dr Jonathan Chung: Yeah, no, I think that would be that’d be something interesting. I could try to put something together on that.
[00:17:23] But that actually brings up another interesting thing that I did some comparison on breathwork versus a lot of these mindfulness practices is, I find that going through breathwork, it takes the judgment that people mindfulness practice. There’s specific subset to the population that it.
[00:17:42] Mindfulness practices actually worsen their anxiety and giving them something where it’s just like there’s no specific right target that they’re trying to hit. When you’re going through breathwork practice, all you’re just trying to do is breathe at a slower pace and have a general guideline of what pace that, might work best for you, and stick to that general guideline.
[00:18:03] There’s no hard rules for it. There’s nothing specific that you should be feeling. You’re not trying to search for enlightenment on this. You’re just trying to, activate circuits of your parasympathetic nervous system, and let that go. Calm down any sense of like hyperactivity or anxiety, anxious, anxiousness or things along those lines.
[00:18:25] Dr Mike T Nelson: Have you noticed a, like, how many minutes per day where you see more of a benefit? So I did the HeartMath stuff for, oh, probably quite a while in the past. And what I noticed is, there seemed to be, this is anecdotal, a threshold between 10 to 20 minutes per day that I noticed more of a benefit on my HRV overall.
[00:18:49] Like I didn’t know it’s a little bit benefit in terms of my state, if I just did it for, three to five minutes, but at least in my experience with a handful of clients, it seemed like the 10 to 20 minutes per day was that. Threshold, if they really were trying to increase their overall HRV or trying to make that baseline more on the parasympathetic side of you notice a general, like timeframe, just like if we were to do zone two training, right?
[00:19:15] We know Oh, I did 10 minutes of zone two today. I’m like, Hey that’s better than, no minutes or five minutes, it’s one of those things where you just, you have to accumulate time doing it to see a bigger payoff.
[00:19:26] Dr Jonathan Chung: Yeah, I have seen that. So from if we’re just talking about HRV benefits, I would say like hitting that 10 to 15 minute threshold is probably most important for that.
[00:19:36] But then I think there is the there’s this idea of what are the clinical benefits of doing a behavior versus what are the physiologic biomarker benefits of doing a behavior? And especially when we’re talking about the clinical population, we care about what are the clinical benefits. And for those patients, It’s to think that just hitting an area of about five minutes is enough to have some of these benefits when it comes to nervous system regulation, reducing feelings of anxiety, things along those lines.
[00:20:08] So I will generally give patients a goal of trying to just get five minutes per day. I would rather you get five minutes per day. And have that frequency of hitting that five minutes per day most days of the week, then trying to hit a more difficult goal of 15 minutes per day, which may have a more therapeutic HRV benefit.
[00:20:28] But if you’re not willing to get to that threshold frequency frequently enough where you’re just not going to do it. Then there’s no benefit at all. So I would almost rather just focus in on the clinical benefit for my population of patients on to just get five minutes to get it done so that they feel the benefit of, hey, every time I allocate this time to just regulate my nervous system, I feel better.
[00:20:55] And for those people, like that’s the end goal for them anyway. And maybe for someone that, is looking for that 1 percent benefit and performance yeah, maybe there is. An added benefit of hitting some of these HRV goals so that, it might improve their physical recovery from training in the margins.
[00:21:13] So we might consider that for that subpopulation, but from a clinical standpoint, where we’re talking about, people where. anxiousness and anxiety and their sympathetic nervous system is so revved up that it’s like affecting their quality of life, then I’ll just say, Hey, let’s hit five minutes.
[00:21:30] If you can do more awesome, then do more, but at minimum, try to hit five minutes per day and don’t feel bad if you miss a day, but if you miss a day, just get onto it the next day and just use this as a tool so that any time that you’re feeling some of these. Anxiety feelings start to come up, even just taking that one moment to just take a long extended breath out and feel some of the anxiety slide off of your shoulders when you’re taking that long extended breath out, just gives them this positive feedback like, Oh, I can control my state by controlling my breathing because if that’s the only thing that they got out of that training.
[00:22:08] And I’m happy with that because it gives them this agency that, Oh, I can control my mood. I can control my state with just a quick manipulation of my breath.
[00:22:17] Dr Mike T Nelson: Awesome. And you mentioned a longer exhale. So when you’re doing this particular technique, do you have them bias the inhale and exhale is the same amount of time?
[00:22:26] And if not, do you want to talk a little bit about. How like respiratory sinus arrhythmia, how our breathing is also coupled to heart rate.
[00:22:35] Dr Jonathan Chung: Yeah, absolutely. So if my patients can tolerate it well, I will encourage them to spend a little bit longer exhale. So I will set a target of Now, if we’re going for a one breath cycle, taking 10 seconds, and I will usually encourage them to go through a four second inhale and a six second exhale as my general target.
[00:22:55] Some, for some people it’s just too uncomfortable for that patient to get to that longer exhale. So if they can’t tolerate that, it’s like, all right, let’s do a five and five and let’s see how you deal with that. And if just that longer breath cycles too long in general, then okay, let’s just try a four and four and let’s see how you could tolerate a four and four breath cycle.
[00:23:13] So a lot of it is We’re working with what the patient is capable of doing depending on what their state of their nervous system is and what they could tolerate it. And then we’ll treat it like a lab and find what makes them feel the most comfortable without driving up some of their underlying anxiety.
[00:23:28] And I tell them not to over focus on hitting set numbers. Let’s focus first on what feels good and then As things feel good, then we can start to play around with what’s technically ideal based on your heart rate variability measurements and what we know from the literature, which is going to be in that six breaths per minute cycle.
[00:23:48] Dr Mike T Nelson: Got it. And what was the second
[00:23:50] Dr Jonathan Chung: part of that question? Yeah, just
[00:23:51] Dr Mike T Nelson: explain for people who are new RSA or respiratory sinus arrhythmia, and that we can modify the state of our nervous system by just changing inhale versus exhale and duration of time spent there.
[00:24:03] Dr Jonathan Chung: Oh, yeah, for sure. So respiratory sinus arrhythmia.
[00:24:05] So people have a negative connotation around the word arrhythmia because they think of like aphid and, heart rate rhythm issues. But humans or mammals have a natural interruption to their normal heart rhythms that is actually linked to the respiratory cycle. And based on things like the amount of stretch that happens inside of the walls of your chest and just from the movement of some of the tissues that go on when you’re going through a breath cycle and triggers responses in your nervous system that could actually modify your heart rate just from changing the pace of your breath.
[00:24:43] From a general standpoint And inhale is generally associated with an increase in heart rate or a sympathetic response and exhale, especially when you take a longer duration of exhale is associated with a more parasympathetic and vagal response. So when we spend a little bit more time on that exhalation phase to a certain point, you’re able to get a more, a stronger parasympathetic reaction with a longer exhale, usually targeting that 6 to 7 second exhale period.
[00:25:13] And I know some people will do breath trainings where they’re like trying to, hold their breath out for as long as possible. There’s certainly going to be a point of declining benefits from that in terms of like parasympathetic responses. But there is, does seem to be a positive association with HRV and parasympathetic responses when you’re extending that exhalation phase just a little bit.
[00:25:36] Dr Mike T Nelson: What other type of breath techniques have you found useful with your population there?
[00:25:43] Dr Jonathan Chung: So depending on what type of activities that we’re going to be doing, so if I know a patient is wanting to prepare their bodies to actually do work, we might actually do some of the Wim Hof kind of hyperventilation style breathwork patterns.
[00:25:59] So if someone is going to get their body and mind just physically ready for competition, there is some evidence that suggests that. The faster paced breathing styles can seem to improve things like cognitive reaction time and attention and focus. So we’ll do a little bit of that Wim Hof breathing style when people want to get a little bit more cognitively focused or cognitively engaged before we do a specific task.
[00:26:24] And we might spend just a couple minutes doing something like that. We might just do breath hold training for people that want to do things that can prove their CO2 tolerance because they were just looking for any type of advantage that they’re going to have and like a physical performance standpoint, or maybe if they’re dealing with anxiety, they’re doing a slow paced breath work, but they just want to find a way to just increase the resilience.
[00:26:48] Maybe that increased resiliency just comes from breathing. Having better tolerance, the amount of carbon dioxide that’s in their bloodstream. So we’ll do some CO2 tolerance testing for them and seeing if that is something that might benefit them. So those are some other things that we had played around in our office.
[00:27:04] Um, there’s other aspects in the literature that I’m curious about that I haven’t really explored quite yet, but I’m looking at some of the training that people will do where they’re breathing hypoxic air and doing some physical training with that. That’s something that I think is very interesting.
[00:27:21] And there’s some compelling training. Studies being done that it seems to improve aspects of neuroplasticity and clinical population, like patients with spinal cord injury or patients with post stroke injury, or doing these hypoxic air breath breathing techniques seems to improve neuroplasticity in a way that helps them improve rehab outcomes.
[00:27:43] So I think that’s another interesting phase that I may consider bringing into the office one day, but haven’t quite explored, done it quite yet.
[00:27:52] Dr Mike T Nelson: On the last one is that kind of, there’s one company, I think it’s called live O2 where you could do alternating periods of higher oxygen and lower oxygen.
[00:28:01] Is it a line that hypoxic? Pathway and this would be during exercise. Is that correct?
[00:28:07] Dr Jonathan Chung: Yeah, so there’s Bicycling systems now where they’ll give you like this big setup that you attach to a face mask And yeah, you can do some training with hypoxic air And that’s something that like I said, I haven’t done yet But it’s something that i’ve been curious about and I just haven’t pulled the trigger on Doing that system because I just don’t have the space for it right now, but it’s something that has my curiosity The would love to talk to more people that are doing it and seeing what type of results they’re getting with it.
[00:28:36] Dr Mike T Nelson: Yeah, I know Kyle Dietz at the University of Minnesota has a couple of those setups and I was asking him about it the other day and he said for certain, high level athletes he’s found it’s been super useful. Because I know in the past I’ve been probably hyper critical of some of those systems because it, as you said, they’re becoming more and more researched in that area, but it’s still very.
[00:29:01] Not really sure what’s going on because the question I always wonder is about transfer, at least from athletics, does it actually transfer to the field because there’s So when I did the physiologic flexibility course, they have a whole section on oxygen and CO2. And I ended up pulling, God, I don’t know how many studies I read on hyperoxia and hypooxia and just trying to see, is there something there we could really use?
[00:29:26] Like for CO2 tolerance, I definitely think there is. You can look at apnea tables, things of that nature. But the, I don’t even know if I ended up putting this in the course or not, but for changes, I couldn’t find a whole lot. And then my thought process, let me be curious what you think on this, is that most of those are not done at pressure.
[00:29:47] So we may be able to give you, if you see on the NFL, like people on the sidelines breathing pure oxygen. Well that’s not really necessarily at a higher pressure, they just increase the amount of oxygen in there. And so there’s some old studies where they actually did it at pressure. So they took Like basically what the looks like a large kind of iron cylinder They had a bike in there and they would lock people in here and then you can change because it’s in a cylinder You could change pressure like relative to altitude So for people listening you go to higher altitude The reason it’s an issue mainly is because the partial pressure of oxygen is so much lower and they did studies with hyperoxia at pressure hypoxia Low pressures and the interesting one I found was And the hyperoxia condition with pressure when they were in the container doing exercise, they did actually see a performance increase in exercise, right, because you can drive more oxygen into the tissue.
[00:30:47] What was crazy though is when they took those same athletes out and retested them the next day in a normal oxia condition in the lab. There was no improvement. Yeah. So I’ve often wondered, these are obviously just acute studies. I couldn’t find much for chronic studies, but do you think there are benefits to training with hyperoxia and hypoxia?
[00:31:12] And would you necessarily have to do that at pressure or not?
[00:31:18] Dr Jonathan Chung: I think there’s a potential for benefit but the question would probably more along the lines of like how much benefit can you get for the amount of Set up and work right to try to achieve that benefit I don’t know if it would be worthwhile and I think pressure does likely make a big difference especially in the hyperoxia type of condition because you know That is one of the important driving forces that You know, can drive oxygen to the tissues.
[00:31:43] So when you’re missing one of those elements, then, you might be, wasting some time and energy on something that could be allocated to another form of training that could probably provide a better physiological stimulus and get better investment for your time. From the hypoxia standpoint, I don’t think we know enough about it, especially for that athletic performance standpoint.
[00:32:08] Because a lot of the literature that is supportive of it is really in the clinical populations of these pretty significantly impaired patients. Where you can do something small to them physiologically and get a disproportionate clinical outcome that them because their baseline is so low that anything that you do that changes creates some type of physiological change.
[00:32:33] The magnitude of that change is going to be a lot bigger. But if you’re taking, trying to take that same principle and apply it to someone that is super highly trained, what’s the magnitude of benefit they’re going to get from that? Even at the best case scenario, it’s probably going to be fairly small because they’re already so physiologically fine tuned that whatever benefit that would be there, theoretically you might not even be able to spot it because they’re such high performers already.
[00:32:59] Dr Mike T Nelson: Yeah, that was my conclusion, too, is that I think there is still some benefit for hypoxia training, even in high level athletes. I can’t put my arms around exactly what that would look like other than maybe some CO2 tolerance stuff, which we’ll come back to in just a minute. Yeah, the hyperoxia I find fascinating, but there’s even less data on that.
[00:33:23] And related to that one, are you a fan of like HBOT or hyperbaric oxygen therapy? And if so, would that be more in a clinical, like a pathology type population? And do you think there’s any benefit for people who are higher level athletes?
[00:33:43] Dr Jonathan Chung: I am a fan of it in a clinical population. And it’s probably allowing the same lines and the same rationale is you’re taking people that their baseline has become so low, whether it’s from traumatic brain injury, like post COVID issues that any type of physiological stressor that is forcing the brain to go through some type of adaptation.
[00:34:03] You’re probably going to have a meaningful clinical benefit and a lot of those patients and specific subsets of those patients that will derive benefit and, it’s something I refer, like my TBI patients to get in some cases, especially like if we’ve hit a plateau in terms of neuro rehabilitation, then, that’s something that we might bring into the fold, especially for some of these cognitive types of symptoms that some of these patients do present with, I think there’s benefit that could be had from it I haven’t seen an athlete get, go through an HBOT protocol and say that things were a lot better for them because of HBOT, like they might feel better, but who knows if that feeling better was just a result of them having this dedicated time to just relax and sit in a chamber where they’re not going to be bothered by some of the other things that they have going on in their life, so it’s hard to disentangle those two things.
[00:34:55] And that type of population, so I think there is some physiological value for the clinical population, but for the athlete, I don’t know that benefits necessarily going to be there and certainly I haven’t really seen any data that suggested that is either.
[00:35:09] Dr Mike T Nelson: Yeah, that was my thought.
[00:35:10] I know Jeremy Schmo here in the Twin Cities has one and he’s found it, for his population of people he’s treating, he’s found it super beneficial and, other clinicians I’ve talked to have found something similar, but And maybe this study exists and I can’t find it. It’d be super cool to take a bunch of athletes, test them before stick them randomly one and HBOD one in the exact same looking thing, but not pressurize the oxygen, right?
[00:35:34] So you have a sham control and see, Hey, is there any real big difference? I can’t find that study. Maybe it exists, but I think it’d be interesting. Cause I, I have my doubts if there is in a healthy athletic population, going to be a huge transfer.
[00:35:50] Dr Jonathan Chung: Yeah, I would be in agreement with them. And for the same reason that we talked about before, like a healthy athletic population, like they’re probably so close to a maxed out performance benefit that like the end that you need to test to even identify a signal would probably have to be really high in order to identify some type of benefit.
[00:36:10] And if the end is that high how much clinical benefit is there or how much real world benefit is there going to be from that? So there’s probably nothing wrong with doing it, because I know some athletes will have their own personal soft chambers that they use, but, I would be hard pressed to see if there’s any actual performance benefit if you took them and randomized them into a sham group, like you said.
[00:36:33] Dr Mike T Nelson: Yeah, I know some athletes who have them and they swear that it’s super helpful, but like you said, if the effect size is pretty slow, pretty low, yeah, again, it might be beneficial. We just can’t detect it. And then you have to have such a massive population to detect such a small effect size.
[00:36:49] So I, I know some people for elite level athletics have made the argument that, well, there’s not much of a negative, they appear to be getting a little bit of a benefit from it even though there’s no literature, and, yeah, I think that could very well be true, but then I also get Crazy emails from people that are convinced they need to buy like an h bot and stick it in their house when They sleep six hours a night and they’re eating like an asshole.
[00:37:15] So it’s like just
[00:37:16] yeah
[00:37:17] Dr Mike T Nelson: Chill out maybe do some other breathwork or something first before you buy an h bot or To hire a professional chef to come in three times a week. So you eat better food, so it’s
[00:37:27] Dr Jonathan Chung: Yeah, like I’ll have people that ask me about it. They should like drop 15 grand on these Hell yeah And I’m just like, well, let’s ask a couple of questions.
[00:37:36] Are you getting 150 to 300 minutes of aerobic cardiovascular activity per week? No. It’s well, let’s pull on that thread first because we know that the upside of that is basically like limitless. And if we’re not hitting that mark. Then, this isn’t going to help you fill that gap any better.
[00:37:55] So let’s focus on like, how do we just get you hitting some of these physical activity guidelines better and just deriving the benefits on your cardiovascular system and on your brain just from hitting your physical activity guidelines.
[00:38:08] Dr Mike T Nelson: Yeah. You’re talking about CO2 tolerance. How would you define CO2 tolerance and do you have any baseline testing or anything that you could do to try to figure out if someone’s listening going, Hey, I wonder how my CO2 tolerance is or anything that they could do an at home test?
[00:38:27] Dr Jonathan Chung: Yeah, sure. So CO2 tolerance is this idea that when people think that they are out of breath, a lot of people associate that feeling of air hunger with the idea that their body doesn’t have enough oxygen. But the reality is, a lot of times when we have this urgent desire to take a breath, it’s actually because the amount of carbon dioxide in our blood.
[00:38:48] is high. And when we have elevated levels of carbon dioxide, it triggers all these receptors, these chemoreceptors in our brainstem to try to take a breath. Because if you just did a simple experiment and you took a pulse ox and put it on your finger, you could hold your breath. For a couple minutes and your oxygen percentage actually doesn’t really go down that much at all.
[00:39:12] So the thing that is making you want to breathe is actually the buildup of carbon dioxide from the metabolic processes that are going inside of your body. And that’s what makes you want to take that breath. And one of the things that has been popularized by like free divers, so free divers, they basically, swim to deep depths, and which basically means that they have to train themselves to hold their breath for a long time and hold their breath under, pretty hard and strenuous pressure.
[00:39:41] So this idea of CO2 tolerance, meaning you’re training your brain to get used to having elevated levels of carbon dioxide. Inside of your bloodstream and just like how you can train your brain to tolerate spinning if you’re a figure skater You can train your brain to tolerate any wide range of a physiological stimulants You can train your brain to tolerate these elevated levels of carbon dioxide And one of the ways that we developed is through these CO2 tables or O2 tables that have been developed for activities like freediving.
[00:40:14] I don’t have it offhand, but the table that I’ve used for baseline has been through some of Brian McKenzie’s. work. So I know he’s been advocating heavily for a lot of these different breathwork practices. He talks about the different gears of breathing when it comes to training athletes and doing things of that nature.
[00:40:33] So that’s the that’s the one that I think sets a good baseline, which you basically, take a few breaths out and then you go for a maximum breath hold, see how long you can hold your breath. And that kind of becomes your baseline. And then you could set and adjust your CO2 tables, which is basically just a training program which Like from a training standpoint, it’s just like progressively loading, how long you can do some of your breath holds versus how long you can do your breath holds with a shorter break versus longer breaks and just adjusting.
[00:41:05] Your reps and your sets and your volume based on any type of training that you might do from like a physical training standpoint. So you could get a lot more details, I think, from Brian McKenzie’s website and things of that nature, but his is a template that I’ve gone off of when. I’m advocating that type of stuff for my patients.
[00:41:23] Dr Mike T Nelson: Very cool. Yeah. I’ve used a lot of Brian’s stuff from shift adapt. They have a great course, the art of breath. I think they’re still teaching that. Yeah, a lot of great stuff. I think they still have it on their website. Like I use their nasal exhale test. So you sit quietly first thing in the morning, take a few breaths, and then take a big breath in, and then see how long you can do a slow nasal exhale, and depending upon the times, that’ll put you in an area of, hey, your CO2 tolerance is good or bad or horrible.
[00:41:54] Yeah, so I’ve been using other athletes now probably Maybe four years now i’d use patrick mckenzie’s bolt test before that But I found too many athletes just cheat their ass off on it And I don’t think I got very accurate numbers from it, but it can work. Yeah And have you noticed that the CO2 tolerances in the clinical population are much worse or does it depend upon the issue or what have you noticed on the more pathology side?
[00:42:23] Dr Jonathan Chung: Definitely if a patient has higher levels of anxiety, their CO2 tolerance is going to be worse. And I think those are the populations that could benefit the most from improving their CO2 tolerance. And a lot of it just is I think a lot of it is almost like a form of exposure therapy where.
[00:42:39] That feeling of breathlessness is going to trigger a lot of the same neural circuitry that people get when they become anxious, that air hunger, that sense of needing to take the next breath, like it’s probably revving up a lot of the limbic circuits inside of the brain and giving them a safe way to experience some of those feelings, I think is probably part of the rationale for, how people could get a training stimulus from doing a CO2 tolerance.
[00:43:07] Type of approach to that where you’re triggering some of these limbic circuits inside of the brain that make you feel fearful and anxious, and you’re giving someone exposure towards these feelings of fearfulness and anxiousness, but it’s something that they have full control over. Cause one of the problems with anxiety is like people feel something is completely out of their control.
[00:43:29] And that’s what drives a lot of these feelings. But if you could give them an anxiety inducing stimulus that they do have, A strong sense of control over and that’s one window that people can pull upon in order to try to train themselves out of that neurophysiology, so to speak.
[00:43:47] Dr Mike T Nelson: Yeah, it’s metal area is super interesting and shout out to Emily Hightower who’s on Brian McKenzie’s team there I work with her a little bit of rapid health optimization also And she’s got a lot of just really great stuff on the I’d say more the behavioral side of breath work and how it affects You know things like anxiety and everything else and yeah, that’s a super interesting Related to CO2 tolerance.
[00:44:13] So if someone’s listening and let’s say hypothetically their nasal exhale test is eh, not that good. They’re around like 20 seconds and they want to increase and improve their CO2 tolerance. What type of breath work would you have them do? And any particular time or frequency you would have them do that.
[00:44:34] Dr Jonathan Chung: So they’re not doing so hot in there. Like I’m going to probably take a point of breath holds that are pretty close to that little time period. So if it’s close to their max, yeah, pretty close to their back. So we might start off by doing some warmup sets where they’re doing breath holds for about 15 to 18 seconds at a time, give them about a minute to recover from each of those sets.
[00:44:59] And then maybe do it three to five times. And we’ll just have them do that for their first week, and then, the next time that they come in, we’ll retest it and see sometimes the neurological aspects of this can change rather quickly, so they might be able to go from 20 seconds to 30 to 45 seconds very quickly, just because things within the nervous system can sometimes change.
[00:45:25] Quite a bit. And once people like, and I think Freddy’s and Adam talk about this quite a bit and pain reset is like anytime that you’re trying to create a change in the neural circuit, especially in regards to pain, you’re just trying to create this window of opportunity where the patient believes that they could get better from the stimulus that you gave them.
[00:45:43] And once you open that window of opportunity, then the nervous system tended to follow pretty aggressively where it could actually make a very rapid change in a very short amount of time. Okay. So I’ll keep them pretty close to whatever their max is. And then when I retest in the week, if they show this large change pretty quickly, then we know that, all right, they weren’t necessarily at their physiological capacity.
[00:46:06] When we did that test, it was all a belief structure, belief system in their head that they couldn’t do it. And just having them expose themselves to it allowed them to start to feel out where their actual true physiological limits are. So we might aggressively start to try to get towards doing. One minute breath holds, and they might spend a longer time at that one minute breath hold, because now they actually realize what their actual true physiological limit is.
[00:46:32] And then we could start to move them towards, 90 seconds. People that are pretty darn good at it, they’ll start to approach three minutes. And at that point, they’re probably less in my clinical population. Those are the people that I’m working on, the more the performance side of things.
[00:46:46] So that’s what a a layout of something like that might look like for me.
[00:46:51] Dr Mike T Nelson: Awesome. You had mentioned some of the Wim Hof stuff beforehand too, or like a hyperventilation or superventilation method, and I think you’d also mentioned you’d only use it for a couple minutes beforehand, and my assumption with that is You want to ramp up the sympathetic nervous system a little bit, but you don’t want to exhale so much CO2 that you’re actually, impeding local tissue oxygenation, which people want to go far down that nerd rabbit hole.
[00:47:23] You look at the bore effect and basically you need local CO2 in order to have a proper oxygen exchange. Cause I made that mistake, God, many years ago where I thought, Oh, okay. So I can do a longer breath hold after doing Wim Hof. Cool. So I should do this before my 2K is on the rower and I’ll see this massive increase in performance because I don’t need as much air.
[00:47:50] And yeah, that didn’t work. Yeah,
[00:47:56] Dr Jonathan Chung: no, I would, I feel that way for if we’re trying to get a little bit of elevated sympathetic nervous system activity, then, I’m not trying to get them to go into a full, hard exhale for and blow out all their CO2 while they’re doing some of this work.
[00:48:11] We’re just trying to run the nervous system up just a little bit. and just using a little bit of that neurological stimulus to, get their sympathetic nervous system a little bit of a pre activation before they actually go into doing something that acquires a little bit of performance. So I know in the whim hop, or like you’re taking these really strong, aggressive exhales, I’ll just tell them to keep pretty close to what your normal exhale is, and just go through it at a kind of rapid pace.
[00:48:40] And then. We might only do one full round of that and then we’ll get the person to, do, a couple of rounds on the NSI after they’ve done it. So that might be. The way that we teach the person to engage their sympathetic nervous system before they start to take on a little bit of a cognitive demanding task.
[00:48:59] Dr Mike T Nelson: As we wrap up, is there any other breathing techniques that you’re like, Oh, we didn’t talk about this one. And I have to mention this one or any of your other Favorites, I know we’ll put a link down to the course and you’ve got a ton more information in there, too
[00:49:14] Dr Jonathan Chung: So those are the ones that I use on a daily basis at a clinical and population level I think going into the rabbit hole breathing.
[00:49:21] There’s all this really interesting stuff that happens with breath work some of it is like through mythological tales almost where you’re like We
[00:49:31] talked
[00:49:31] Dr Jonathan Chung: about yogis who have been able to do these pretty remarkable beats You And some of it involves so one example and kind of semi popular one, especially through the yoga community is like sumo, where people can use some of these breath styles to, try to elevate their body temperature.
[00:49:50] I think that is super interesting. But how much of it is due to visualization versus how much is due to breath work itself? It’s hard to say.
[00:49:58] Dr Mike T Nelson: So if you’ve ever done that for prolonged periods of time, it’s freaking hard. Yeah. Like it’s just not an easy thing to do. Yeah,
[00:50:08] Dr Jonathan Chung: for sure. So I think there’s a lot of cool stuff to like, look at from breathwork and knowing what actual, been under the microscope of the scientific method versus others that have just been passed down through the generations.
[00:50:22] There’s still work that can be done. That’s interesting. But I think when it comes to just the real day to day applications, I think it just comes down to, hey, there’s slow paced breathing to help generate a calming, more parasympathetic type effect. There’s more rapid pace, which gives you a mild sympathetic type training.
[00:50:40] And, then you could go down the rabbit hole of doing some of these breathwork practices that, people are using as a substitute for, psychedelic medication, psychedelic drugs, which, tells you how much you can manipulate your physiology just by changing the pace of your breath.
[00:50:57] So there’s a lot out there that is super interesting, but in terms of applying these things to a athletic and performance and, mental health. population. I think we hit most of the nuggets there. But there’s still a lot of interesting stuff that’s out there that’s probably worth exploring just depending on what your needs are.
[00:51:19] Dr Mike T Nelson: Yeah, there’s a whole practice. So it was in Stanlis Graf had the, it was one of the top LSD clinics for psychiatric use back in the fifties and into the sixties until it was made illegal.
[00:51:31] And
[00:51:31] Dr Mike T Nelson: then he ended up switching his whole practice to basically like a Wim Hof super ventilation, type.
[00:51:38] method and there’s a whole different things on more of a clinical side. People can go down that area too, which is fascinating.
[00:51:47] Dr Jonathan Chung: Yeah. Like I think it was the holotropic breathing. Holotropic
[00:51:50] Dr Mike T Nelson: breathing is the name. Yeah.
[00:51:52] Dr Jonathan Chung: Yeah. Some of the stories from that are wild. So we reviewed those, some of the history of that during the course.
[00:51:57] And if you’re interested in the course obviously it’s through the Carrick Institute, they have it’s a six or eight hour course where you break down a lot of the neurological circuits. If you want to nerd out on, some of the brainstem, frontal integration aspects that are involved with breathwork, then we go over a lot of that in the course.
[00:52:14] And then some of the history, like the history of breathwork practice is just pretty remarkable, even going down into oh, nasal breathing. So nasal breathing it probably gets a little bit hyped up in terms of people exaggerating some of its benefits, but there is some pretty cool science on the way that breathing in through the nose helps to synchronize a lot of the neurological pathways in the brain versus breathing through the mouth, and how there’s an evolutionary context through it where mammals were previously we experienced the world through our noses, And we still have remnants of that, and part of being able to maximize the synchronization and what’s the correct word for it entrainment of our brain, that taking these inhales through the nose actually magnifies the effect of entrainment and probably helps facilitate plasticity when people are trying to do a breathwork practice or doing any type of task that might involve some cognitive depth to it.
[00:53:17] Dr Mike T Nelson: Excellent.
[00:53:18] Awesome. Well, thank you so much. I really appreciate it and tell people where they can find you online and remind people again where your clinic’s located if they’re around the area down there.
[00:53:30] Dr Jonathan Chung: Sure thing. So I’m pretty active on Instagram and Twitter. My handle is at Dr. Jonathan Chung. My practice is called Keystone Chiropractic and Neuroplasticity. We’re in Wellington, Florida, and you can follow a lot of the content we make about clinical neuroscience at Keystone Neuro, N E U R O.
[00:53:50] Dr Mike T Nelson: I really appreciate it. And we’ll definitely put a link to the awesome carrot course you have. That’s that goes even in more in depth on this below. Thank you so much. Really appreciate it. Thanks Mike.
[00:54:03] [00:54:03] Dr Mike T Nelson: Huge thanks to John for coming on the podcast and discussing all the great clinical work that he’s doing. If you are in the Florida area down there, make sure to check him out in person. Also check out his course the Neuroscience of Breathwork through the Carrick Institute. Again, I don’t have any disclosures on that course, but I am an associate professor with the Carrick Institute.
[00:54:26] And if you want to know how breathing affects pH, temperature changes, expanded fuels from lactate to ketones, just do overall. make you a much more resilient, anti fragile person and have record recovery, then check out the Physiologic Flexibility Certification. It is open right now as of this recording until Monday night, October 21st at midnight Pacific Standard Time.
[00:54:55] There’ll be a link down below. You’ll be able to check that out and anything else I can do, please hit me up. Thank you so much for listening. We really appreciate it. You got more great stuff coming at you next week. Once again, take care.
[00:55:09] Personally, I don’t care for puppets much. I don’t find them believable. I don’t believe you!
[00:55:16] This podcast is for informational purposes only. The podcast is not intended as a substitute for professional medical advice, diagnosis, or treatment. You should not use the information on the podcast for diagnosing or treating a health problem or disease or prescribing any medication or other treatment.
[00:55:32] Always seek the advice of your physician or other qualified health provider before taking any medication. Or nutritional supplement. And with any questions you may have regarding a medical condition, never disregard professional medical advice or delay in seeking it because of something you have heard on this or any other podcast reliance on the podcast is solely at your own risk information provided on the podcast does not create a doctor patient relationship between you and any of the health professionals affiliated with our podcast.
[00:55:59] Information and statements regarding dietary supplements are not intended to diagnose, treat, cure, or prevent any disease. Opinions of guests are their own, and this podcast does not endorse or accept responsibility for statements made by guests. This podcast does not make any representations or warranties about guest qualifications or credibility.
[00:56:17] Individuals on this podcast may have a direct or indirect financial interest in products or services referred to therein. If you think you have a medical problem, consult a licensed physician.






Leave A Comment