Join me, Dr Mike T Nelson, on this week’s episode of the Flex Diet Podcast as Dr. Catrina Fabian and I delve into comprehensive pelvic floor health. We discuss pelvic floor dysfunction, postpartum recovery, neuromuscular control, and the importance of functional muscle assessments.
Our discussion covers key topics like visceral massage, fascial connections, and the impact of jaw tension on pelvic health. Learn expert tips on breathing, hydration, stress management, and non-surgical treatment options and discover how to improve joint mobility, address overactive pelvic floor muscles, and enhance overall well-being.
Sponsors:
- Tecton Life Ketone drink! https://tectonlife.com/ DRMIKE to save 20%
- Dr. Mike’s Fitness Insider Newsletter: Sign up for free here.
Episode Chapters:
-
03:08 Welcome Dr. Catrina Fabian
- 04:32 Understanding Pelvic Floor Dysfunction
- 08:19 Core and Pelvic Floor Mechanics
- 16:42 Fascia and Its Role in Pelvic Health
- 31:40 Personal Injury Experience
- 32:06 Role of Physical Therapists
- 32:54 Visceral Massage Insights
- 36:25 Fascial Connections and Techniques
- 39:58 Breathing and Pelvic Floor Health
- 43:41 Scar Tissue and Microcurrent Therapy
- 47:10 Research and Clinical Practice
- 48:43 Practical Tips for Pelvic Health
- 54:55 Conclusion and Contact Information
Flex Diet Podcast Episodes You May Enjoy:
- Episode 267: Demystifying Women’s Fitness and Nutrition with Alli Fahrenbach
- Episode 224: Mastering Sports Psychology for Gym Success with Mona Pretorius
Connect with Dr. Catrina Fabian:
Get In Touch with Dr Mike:
Rock on!

Dr. Mike T Nelson
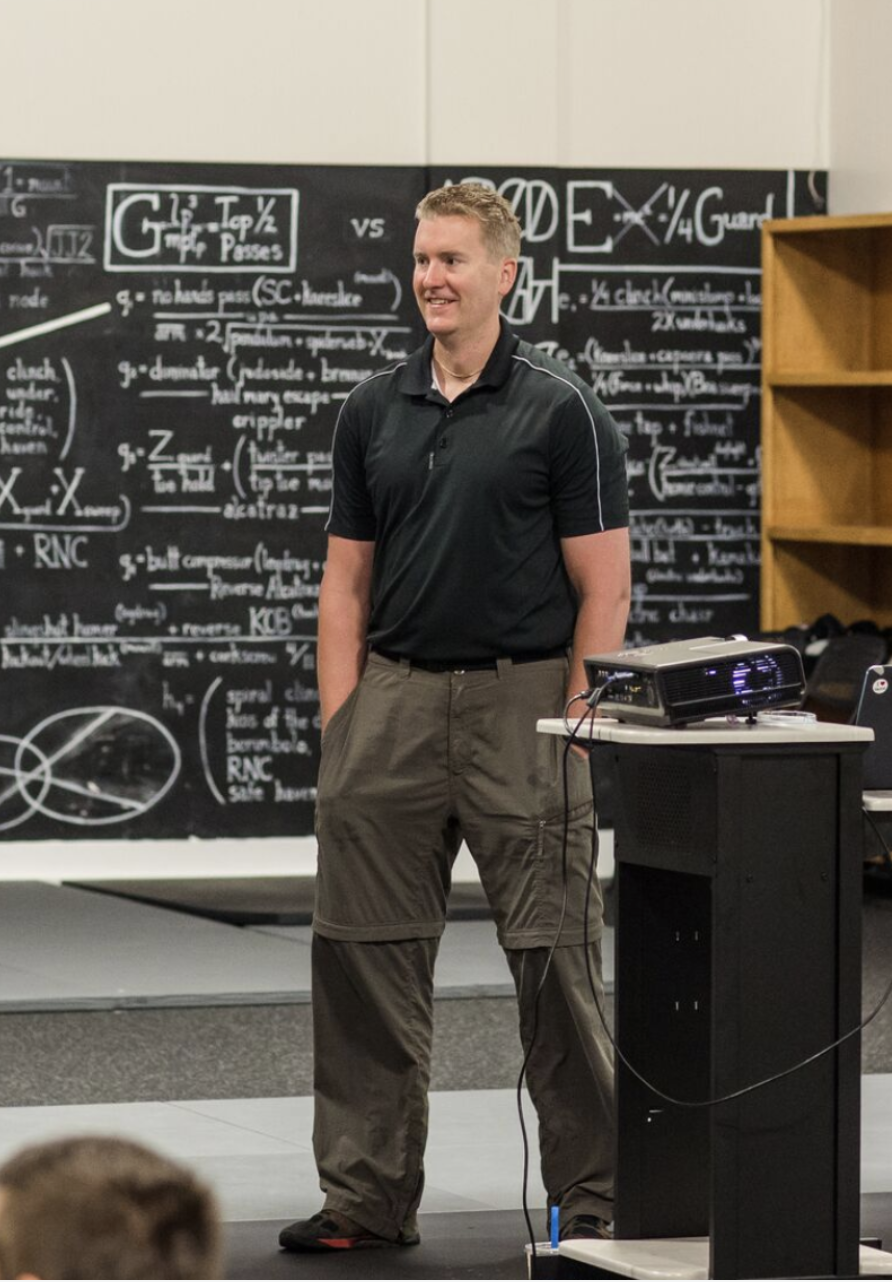
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
[00:00:00] Dr Mike T Nelson: Hey, what’s going on? It’s Dr. Mike T. Nelson here. Welcome back to the Flex Diet Podcast where we talk about all things to increase muscle performance, improve body composition and do all of it without destroying your health and the flexible framework. Today we’re talking all about the pelvic floor with our guest, Dr.
[00:00:26] Katrina Fabian. And this podcast will range from all things pelvic floor such as pelvic floor dysfunction. What is the role of the pelvic floor? Things such as visceral massage, how breathing is impacting this, the role of scars what are some things you should do to maintain pelvic health, and also things you might want to avoid.
[00:00:55] Looking at different breathing patterns, movement patterns, and much more. So super interesting, was awesome. We did get to meet Dr. Katrina and also Zach Couples again. Last time we were in Vegas which was amazing and really enjoyed this podcast. I think it’s one of these areas that I’ve noticed in my own practice a fair amount of people have.
[00:01:22] Some sort of pelvic floor issue, but it’s not really talked about a whole lot. And it’s one of those things that a lot of people just assume is normal. And in reality, it isn’t. This broadcast is brought to you by my newsletter. So if you enjoyed this podcast, definitely check out my newsletter. Go to MikeTNelson.
[00:01:45] com at the very top, there’ll be a newsletter button. You can click there. and subscribe to the fitness insider list for free and just send me a note there and I’ll send you a free gift also. We also have exogenous ketones by Tekton. I am a scientific advisor and an ambassador for them. So if you’re looking for something to help with, I’d say I find it best help with cognitive function even some performance stuff at a little bit higher dose, like right around two cans for myself.
[00:02:20] Check them out. It’s an exogenous ketone, so it is the BHB, so beta hydroxybutyrate molecule bonded to glycerol. And I like this especially if I’m trying to do more cognitive work later in the day. Definitely does seem to help with that. And it’s not a stimulant either, which is great. So you could literally drink this before you went to bed and not have any issues.
[00:02:48] And sometimes in a few cases we’ve had people report that it definitely helps their sleep too. So, check that out and enjoy this podcast on all things pelvic help, fascia, and much more with Dr. Katrina Fabian.
[00:03:07] [00:03:08] Dr Mike T Nelson: Welcome to the podcast. Dr. Katrina. How are you?
[00:03:11] Dr. Catrina Fabian: I’m great. Thank you. Well,
[00:03:13] Dr Mike T Nelson: yeah, it’s very nice to see you again We got to meet you for the first time in Vegas this past year, which was super fun
[00:03:21] Dr. Catrina Fabian: That was so fun. We had great Korean barbeque.
[00:03:24] Dr Mike T Nelson: Yeah, it was. It was a good time. Vegas was always fun.
[00:03:27] You guys are still enjoying it out there?
[00:03:30] Dr. Catrina Fabian: What’s that, sorry?
[00:03:31] Dr Mike T Nelson: Oh, you’re still enjoying Vegas?
[00:03:32] Dr. Catrina Fabian: Oh, yeah. It’s so fun. We’ve got new shows all the time. We’ve been to a couple comedy shows since, too. So there’s always something to do. It’s great.
[00:03:42] Dr Mike T Nelson: Have you been to the Spear yet? I keep hearing all these things about it.
[00:03:45] I didn’t, I haven’t been into it yet, but the more stories, and I saw part of the UFC that was there, and it just, yeah, it’s definitely on my list now.
[00:03:55] Dr. Catrina Fabian: Same, I know. Next time you’re here, we have to go, because we haven’t gone yet either, and it’s such a cool spectacle to see, you can see it from almost anywhere in the city, and so we just have to go inside.
[00:04:08] Dr Mike T Nelson: Yeah, cause last time it was relatively new and you could see it and it was weird, especially like in the evening, you look out your window, you’re like, Oh, it’s just, you don’t realize like how big it is just from the outside. It’s pretty wild.
[00:04:20] Dr. Catrina Fabian: Exactly. It’s crazy to live here where we walk the strip and everyone’s taking photos and videos of it.
[00:04:26] And to us, it’s a normal daily thing.
[00:04:28] Yeah.
[00:04:29] Dr. Catrina Fabian: So.
[00:04:31] Dr Mike T Nelson: Awesome. And today’s topic is more on pelvic floor issues, which is your specialty. And how did you get into working primarily with pelvic floor dysfunction? And we’ll explain how this shows up for different athletes and people who train.
[00:04:50] Because it’s, I wouldn’t say it’s super common, but I think it’s much more common than what people realize.
[00:04:57] Dr. Catrina Fabian: Yeah, that’s right. And that was part of the interest back when I was a student physical therapist, it was being exposed to pelvic floor dysfunction or hearing women at the gym talking about how they couldn’t do one move because they would leak and then learning that.
[00:05:12] Yeah. And then learning that physical therapists could actually do something about it. And so it was a lot of observing other physical therapists, listening to one speak at a big national conference, and then Really deciding that I wanted to do this.
[00:05:28] Dr Mike T Nelson: Very cool. What are, if people are listening and they’re wondering, huh, I wonder if I have some pelvic floor dysfunction, maybe I don’t know about it, obviously this isn’t a diagnosis, but what are some common things that people would report that, yeah, you probably want to get that checked out to see what’s going on.
[00:05:48] Dr. Catrina Fabian: Right. Yeah, so there are three umbrella things. areas that we screen for pelvic floor dysfunction, the first being bladder dysfunction. So it’s helpful to know what the norms are in order to know if you’re showing up with abnormal pelvic floor function. And so norms are being able to hold their bladder for two to four hours, not having to get up often at night.
[00:06:16] Disrupting your sleep. It’s holding in our urine and not leaking. It’s being able to jump and cough and sneeze without leaking. The second umbrella is going to be bowel dysfunction. So we also should be able to hold that, but also empty easily and normal regularity would be going anywhere from three times a day, all the way up to every three days.
[00:06:43] Thanks.
[00:06:43] Dr Mike T Nelson: Okay, so even up to every three days, it’s still normal.
[00:06:46] Dr. Catrina Fabian: Yes! So, I noticed That’s
[00:06:48] Dr Mike T Nelson: surprising.
[00:06:49] Dr. Catrina Fabian: Right? It sounds like constipation for a lot of people.
[00:06:51] Dr Mike T Nelson: Yeah.
[00:06:52] Dr. Catrina Fabian: That’s right. But the good thing to know there is that if that’s been someone’s normal for the majority of their life, that’s their normal and that is within normal as well.
[00:07:02] But if they go from two times a day to every three days, that, that would be considered constipation for them. Got
[00:07:09] Dr Mike T Nelson: it.
[00:07:09] Dr. Catrina Fabian: Yeah. And then sexual function is the third primary role that the pelvic floor muscles. play a role in and so normal sexual function includes being able to have intercourse without pain and Being able to tolerate pelvic exams or prostate exams without pain And having yeah, no, basically pain is the biggest issue that we see with sexual function
[00:07:39] Dr Mike T Nelson: and Will be some things that if people come into your office one that you can do and then two for The lifting population are there things that Maybe you should, I don’t want to say avoid, but be more cautious of it.
[00:07:57] I think like High pressure Valsalva maneuvers all the time, things of that nature.
[00:08:03] Dr. Catrina Fabian: Right, right. That is something I need to coach my patients with if they are heavy lifters. It’s, the Valsalva maneuver is great if you’re lifting at 80 percent of your max or greater. We should explain
[00:08:15] Dr Mike T Nelson: what that is too, by the way.
[00:08:16] That’s true. Just for people.
[00:08:17] Dr. Catrina Fabian: That’s very true. So, the Valsalva maneuver, it is holding, essentially holding our breath, closing the glottis, bracing the entire core to lift heavier. because of that more stable trunk. So it is a great tool to use with heavier loads, but to have awareness of the bottom part of the abdominal canister, which is the pelvic floor, is essential.
[00:08:48] So we need to be able to contract the pelvic floor muscles at the same time as engaging the entire abdominal canister if we are going to use a Valsalva maneuver. But besides that, if someone’s lifting weights that they can lift for several reps, they really should not be using that for the majority of their workout.
[00:09:11] That will create undue stress on the pelvic floor over time.
[00:09:17] Dr Mike T Nelson: Yeah, I feel like if you go to more, not to pick on CrossFit gyms, but even powerlifting gyms and other places, in general, I would say you see advanced lifters are much better graded tension where, yep, if it’s a true all out one rep max, like they’re pretty tense, but they know how much tension to dial up that’s appropriate for the lift where I think newer lifters, it’s wet spaghetti noodle or max tension.
[00:09:48] There isn’t really anything in between. That is so right. That is so right. So working with, for example, the postpartum population where that neuromuscular control is altered, it is a lot of, let’s bring that down by 50 percent or give me less than that, for sure. Would you agree that all things being equal, the lesser amount of tension you could do and still complete the lift and whatever we agree upon is good form, which is the whole probably different podcast and what good form is.
[00:10:26] But would you agree that’s probably better than just maximal tension to try and cover up other movement issues?
[00:10:36] Dr. Catrina Fabian: 100%. Yes. Because the stiffer we get, the less, the more movement constraints there are. And so it depends on how dynamic the movement is as well. And if we think about it, the pelvic floor should be moving like a trampoline in a way.
[00:10:56] So say someone is doing double unders. and their pelvic floor is completely stiff because they are holding such a stiff core. Every impact on the ground is going to be hitting, so to speak, hitting a stiff pelvic floor, and so the organs will also be hitting that pelvic floor. So to have some more flexibility and less stiffness will allow the pelvic floor to move, and the bladder on top for example.
[00:11:27] Preventing leakage. That is one thing that is eye opening for a lot of my patients because they think that to hold the entire time is what’s necessary to prevent leaking, but it’s definitely the opposite.
[00:11:41] Dr Mike T Nelson: Yeah, it seems like the common thing is, and it makes sense, that, oh, if I just hold more tension here, that’ll solve the problem, but from what you’re saying, it sounds like it may, one, not always work, and two, probably not the best solution.
[00:11:56] Strategy and three potential. They may not be helping them in the longterm.
[00:12:01] Dr. Catrina Fabian: Yes, 100%. And if you think about a great muscle contraction, there’s the eccentric portion and then the consent concentric portion, and that’s needed for the pelvic floor muscles as well. So we won’t get any lengthening if they are contracting the whole time throughout a movement.
[00:12:17] So, yes.
[00:12:20] Dr Mike T Nelson: What is the normal movement of the pelvic floor and you talked about the canister like do you want to explain? What are the components of the canister? And what is normal? Pelvic floor because it my guess is a lot of people may think that and this is unfortunately taught a lot of times in undergrad that everything’s Static it doesn’t move like you look at a lot of the pictures, but then as you advance you realize oh Nothing’s really static.
[00:12:47] Even the bones are slightly moving and all this like movement is actually going on.
[00:12:53] Dr. Catrina Fabian: Right. Okay. So we’ll, let’s break down the core. So we all know the rectus abdominis muscle, the six pack abs. That’s the very superficial, the most superficial abdominal muscle. Everyone knows the oblique muscles as well, so that’s the second layer behind the rectus abdominis.
[00:13:12] Then we also have the transverse abdominis, which goes from the front all the way around the sides. It’s long, it goes from the bottom of the sternum all the way down to the pubic bone, and then it connects through fascial tissue to the spine. Now, a lot of people tend to forget that we have the ceiling too, and the ceiling is the diaphragm.
[00:13:32] And then the floor is the pelvic floor muscles. And so these muscles go from the pubic bone in the front to the tailbone in the back, and then over to the ischial tuberosities. So really the floor of the pelvis. And so that’s the abdominal canister. And yes, you’re right. We forget that there’s a lot of movement with this.
[00:13:51] So, Normally, as we inhale, if we’re taking a nice inhale with good expansion, the diaphragm is moving downwards to allow the lungs to expand and fill with air. So the viscera, the organs underneath, are also moving downwards. And so we get a lengthening of the pelvic floor. And if the ribcages are moving outwards as well, and expanding forward and back, we also have expansion of the rectus abdominis, the obliques, and the transverse abdominis.
[00:14:23] And then as we exhale, everything comes back in together, like a balloon expanding, and then deflating again.
[00:14:30] Dr Mike T Nelson: Yeah, so it’s a very dynamic system, and then, some people may include muscles, in the back and everything else that go all around it, too, but I know some people don’t include those, but yeah.
[00:14:42] Dr. Catrina Fabian: Right, right. The Multifidi, those are, yes, those are great core stabilizers. But they’re so
[00:14:47] tiny!
[00:14:48] Dr. Catrina Fabian: They’re so tiny. The Rotatories yeah. And so for me, I’m like, I’m not really affecting the Multifidi unless I’m doing something very specific, like needling to them.
[00:14:58] Dr Mike T Nelson: Wasn’t that like a whole, I don’t want to blame Paul Hodges, but I think it was like a whole school of like physical therapy for a while.
[00:15:04] Wasn’t it to retrain the multifidus for your back pain? And I don’t know, a whole bunch of crazy stuff.
[00:15:10] Dr. Catrina Fabian: Yes, and it’s so funny because yes, we were taught that in school and then I injured my back in February And I was like, I’m just I just think it’s my multiple
[00:15:27] Dr Mike T Nelson: It’s wild when you do actual human dissection to how My visual representation was not really what I thought. I thought even the QL Quadratus Lumborum, you hear about all this stabilizing and all the stuff it’s doing. It’s like the size of my pinky. And again, we’re looking at probably detrained people, and I understand all of that.
[00:15:47] But I was surprised that a lot of the muscles I thought were main players, like the TVA, like transverse abdominus, I was always taught that Well, that’s like a corset around your core. So this is your main Stabilizer for your core and you know out of all the dissections I’ve done which is a fair amount.
[00:16:06] It is Ridiculously thin it’s hard to find in most people now granted. Maybe it’s atrophied away, etc I agree, but comparative even in the same person to the obliques and the erectus abdominis there’s No real difference in size, like the TVA is very small.
[00:16:24] Dr. Catrina Fabian: That is so cool that you’ve done several cadaver labs.
[00:16:28] Dr Mike T Nelson: Yeah, if anyone hasn’t done cadaver labs, I highly recommend it. It’s great.
[00:16:31] Dr. Catrina Fabian: Yes I know I’m in my fourth year of practice now and I want to go back and do a cadaver lab. I was able to during my doctor training, but I’m like, it’s time I want to do it again. And so, yeah, to separate the fascia, every, like everyone, like every physical therapist will say, everything is connected.
[00:16:48] So it is tough to separate the fascia layers and They are thin. So what the interest, the interesting thing and why pelvic floor therapists play, really dial in into the transverse abdominus often is that there’s actually a fascial connection from the transverse abdominus all the way into the pelvic floor.
[00:17:10] Yes. So, we, I think we do tend to. focus on it a bit more in the beginning if needed because it’s been shown that it, there is synergy between the levator ani, which are the pelvic floor muscles that do a kegel and the transverse abdominis. So really if one is lacking, we’re not getting the optimal amount of strength in the other one.
[00:17:33] So It’s for us, it’s important in that way, but then of course, like with no movement, are we ever working in isolation? So the obliques and the abdominis will have to come in as well. But to gain that coordination first, it’s often a first step for core rehab, abdominal rehab. post surgical postpartum.
[00:17:59] So, yeah.
[00:18:02] Dr Mike T Nelson: How much of that function do you think is, and it’s hard to differentiate these two because they happen all the time in one, you could argue cause of the other, but how much of it do you think is pressure changes versus muscular activation? And would you get at that by looking at positional differences, lying down, standing up versus gravity to try to figure that out?
[00:18:29] It’s been completely anecdotal. Again, I’m not a physical therapist, but I’ve seen some people have Weird stuff happen when they stand up, but we’re completely asymptomatic lying down. And we did just old school Kendall muscle testing. Like on a table, they tested pretty damn good for most things, but yet the second they stood up, it’s like, whoop, it’s back again.
[00:18:50] Yes.
[00:18:52] Dr. Catrina Fabian: This is awesome. Yeah, Dr. Mike, that’s a, an amazing question because traditionally pelvic floor therapists are testing the pelvic floor muscle strength with an internal assessment in hook line. So there’s no gravity, but we know down.
[00:19:09] Yeah,
[00:19:10] Dr. Catrina Fabian: right. Yes. Lying down hook line, but we know that if someone stands up.
[00:19:14] There is automatically more pressure on the pelvic floor, and because the pelvic floor muscles are a postural muscle, they do increase in activation. Or, they’re not able to withstand the pressure from gravity and the organs below, so. There is definitely a positional component, and that’s a great question.
[00:19:33] I, I think some of it, I think some of it is from muscle activation. I don’t know the percentage, but, we’ll, we get the real time feedback when we’re doing neuroreeducation, when someone is lying on their back, and say we’re doing an internal assessment as well, and cueing them to activate their transverse abdominis, and then feeling what their pelvic floor muscles are doing, but yeah, so I don’t know what the mix would be there, but it would be, Optimize, I think if someone was standing and then we were doing the same thing and which is like what public rehab therapists have pushed to do is get the person off the table and get them in a more functional position because that’s everything.
[00:20:14] Dr Mike T Nelson: Yeah, I think physical therapy, even I know chiropractors back in the day would always treat people lying down and some of the more progressive ones I know now will do it standing seated. The guy I go to does more functional, I guess you could say neurology, chiropractic, where I’ll have to look a certain way before he adjusts me in a standing position.
[00:20:35] And, just trying to get these things to transfer more to, real life. And that’s a, that’s a huge mistake I made early on. Like I, Tested a bunch of people on the table and they left. They said, Oh, I feel better. Yay. Woo hoo. And then they keep coming back. I’m like, why are you coming back?
[00:20:52] Like we’ve, we fixed all your issues. And it took me a while to realize, Oh, I should have them probably stand up, walk around, lay down, test them, standing, test them, seated, test them in different positions to see, did anything even transfer. And unfortunately, when I first started doing that, I realized, Oh, a lot of the stuff I did transfer at all.
[00:21:14] Dr. Catrina Fabian: It’s humbling moments like that. And it’s so funny because we know these things. It’s we coach for specificity or we, I know in our clients programs, but sometimes as clinicians, we need to remember Oh, what we’re doing also needs to have those components too. So specificity and standing, like we need to include that too.
[00:21:33] Yeah. And it’s been interesting too. I’ve taken so much continuing education this past year and. And I’m trying different techniques, but it’s interesting to just seeing the way someone activates, for example, their transverse abdominis in standing versus sideline. Like the sideline position is not something I mindfully assessed and coached, but now it is.
[00:21:56] And it’s very interesting to see the differences.
[00:22:00] Dr Mike T Nelson: Do you think that’s one obviously positional, but also just different pressures against gravity because they’re obviously rotated?
[00:22:08] Dr. Catrina Fabian: Right. It probably is that it might even be like that input to their side, maybe the manual pressure.
[00:22:14] Right. Or they are already used to activating their TA in sideline when they’re pushing themselves off a bed. I don’t know. Maybe, yeah, that is a movement pattern they’ve already established, but in standing they haven’t.
[00:22:31] Dr Mike T Nelson: Very cool.
[00:22:32] Dr. Catrina Fabian: Yeah,
[00:22:32] how we talked a little bit about fascia, and if you ever get the chance for people listening I think Tom Myers still teaches a course where you can do human dissection for a whole week I’ve done it three times now and it’s Pretty amazing because they use fresh tissue.
[00:22:49] So the tissue has never been embalmed. So a lot of the undergrad anatomy physiology work I did for many years was all embalmed tissue. And it was great. It’s definitely useful. Like you get to see a lot of stuff, but the first time doing fresh tissue, it was crazy to see, the color difference and to actually see the fascia because it sticks out in fresh tissue where embalmed tissue yeah if you’re really good you can find it and you know what you look for but everything turns this weird sort of grayish color and it all looks the same after a while and i was just shocked to be like oh everything’s connected to everything and you could clearly see where there was more fascia you could separate the layers so what role do you think Fascia plays in rehab, and can you do specific things to try to target the fascial system more than the muscular system?
[00:23:44] Or is it hard to even tease them out since they all work in concert together so much?
[00:23:50] Dr. Catrina Fabian: Oh, yes. If there’s, if there’s a group of physical therapists in a room and just one pelvic health physical therapist, they’re going to be the ones talking about fascia the most, usually. If we’re just generalizing.
[00:24:03] And that’s, yeah, and that’s because we do think about that a lot. For example, a lot of our patients have gone through abdominal surgeries, whether it was like an inguinal hernia surgery diastasis rectus abdominis surgery after abdominal separation or thinning of the linea alba. Or a hysterectomy, spinal surgery.
[00:24:25] Anyway, we know that scar tissue restrictions can happen. There, they, scar tissue does form after surgeries, but they may or may not. result in restrictions. Either way, we often use our hands, which is that’s a just a quick clinical way to do it. It’s I feel like fascia is tough to see in the research and the actual changes, but you probably know more about that.
[00:24:56] Dr Mike T Nelson: Yeah, there just isn’t as much research period from what I and again, I’m not an expert on pelvic floor stuff at all. But just in general, like I’d say fascial research has gone up a lot in the last 10 years, but I’d say even previous to 12 years ago, there were some, but not nearly as much as what we have now.
[00:25:14] Dr. Catrina Fabian: Okay. Right. Awesome. And it’s I just think it’s hard to prove those things. However, Oh,
[00:25:19] super hard. Right.
[00:25:21] Dr. Catrina Fabian: I know. And so, when I was a student, it was like one of those things where okay, I know fascia is a thing and I just have to trust that we can make changes to it. Anyway, now in clinical practice, I 100 percent know.
[00:25:32] So, sometimes someone will have a sharp shooting pain that’s random or with a certain movement. And oftentimes my mind will go to the fascia. What’s the fascia doing? Where are the restrictions? And then we do some myofascial decompression, and then it’s gone. Or even with peripheral neuropathy.
[00:25:50] That’s been an amazing tool. And just with cupping or hands on techniques. So, yes we’re trying to affect the fascia a lot, and there are a lot of courses, too, for specifically for pelvic floor pelvic health rehab therapists that deal with fascia and movement of the fascia of the viscera, and then specifically for the GI system or urinal genitourinary system.
[00:26:17] So, again, what is
[00:26:20] Dr Mike T Nelson: the fascial decompression technique do you do? And you mentioned It sounds like there’s one general technique and another one maybe on the superficial layer, maybe like on close to the skin and the fascial layer or the differences there.
[00:26:34] Dr. Catrina Fabian: So I usually, for me, it’s usually with cupping.
[00:26:37] I’ll feel with, I’ll feel with my hands, maybe picking up the fascia, trying to also get deeper in and lift and roll that way. But Usually I’m using cupping as a form of myofascial decompression, and so, or well, I should say myofascial decompression with cupping, especially because a lot of the times my patients won’t tolerate just pressure, sometimes that, yeah, produces too much pain, but they tolerate that decompression.
[00:27:08] Interesting. Yeah. But then we are also taught that just some deep pressure sustained for about a minute or more is going to result in fascial changes and bring more movement. And then if we’re talking about cupping, that actually brings like more hyaluronic acid to the area, which is moisture. And so there are lots of mechanisms.
[00:27:34] To it and so I think it’s just a matter of finding what the patient tolerates and then what makes sense to you So you can explain it as well to them
[00:27:44] Dr Mike T Nelson: Yeah, that’s the hard part. I one of the techniques I use once in a while is a fascial rolling technique I got from tom myers. It’s probably very similar to what you’re doing.
[00:27:52] You’re picking up the For people listening, the layer of the skin air quotes next to the fascia and you make this little wave with it and you’re trying to push this little wave across. So for people listening, like if you’ve ever worked on someone that all their tissue feels really stuck, like you apply a normal pressure and you can’t create any sheer movement.
[00:28:14] Like you can’t slide any of this tissue around and everything just feels. Dense and like a brick, there’s no fluidity to it at all. And I used to think all that stuff was like, ah, this is a bunch of woo. That doesn’t make any sense. And the thing that blew my mind is again, I was doing the course with Tom Myers.
[00:28:35] And I was in charge of doing the knee dissection. And so the first thing you do is you, we have the cadavers, they haven’t been embalmed. So you can do range of motion testing. We didn’t know any of the history of them. So we go through, we do a little range of motion assessment on them, put our little numbers up on the board.
[00:28:50] And I go to test the right knee. And I couldn’t barely get any movement in the knee at all. And I’m like, well, it’s an older person. Who knows what’s going on? And there’s probably disaster. Maybe they had a knee replaced and it went bad. Who knows? Didn’t see any scarring on the knee. Oh, whatever.
[00:29:05] And so the next thing we do is start taking off the layer of the skin. So get the layer of the skin off all the way around the knee. And I’m like, Oh, I’ll be a good little engineer scientist. I’ll test the range of motion again, not. Thinking anything’s going to happen. And I could literally bend and flex the entire knee.
[00:29:23] And I’m looking at it and I’m going, and I had someone else, check it beforehand too. And I’m like scratching my head going, what the hell is going on? And I’m thinking maybe she’s got some debris in her knee or something’s getting locked up that got unlocked. And so I asked Todd Garcia, one of the dissectors, I said, Hey man, I think I screwed something up.
[00:29:42] I think I cut something. I don’t know what I did, but the knee did not move at all. We removed the skin. The knee is like super fluid right now. He looks at me and he goes, yeah, that happens. And then just wanders off. I’m like, what do you mean this happens? I had Tom come over and he’s yeah, we’ve seen that in a few cases where You know, the hypothesis is that yes, your skin is stretchy.
[00:30:06] But if you think about movement, like you’re moving inside of this sack of skin, and then you have to have this sliding of all different movements and muscles. And one of the theories is that layer between the skin, the fascia, and that next layer down gets stuck. And that can actually cause like physical impediments to joint movement and stuff.
[00:30:26] I was like, Okay. I don’t know. Whatever. I’m still thinking I’m going to get into the knee and it’s going to be a disaster. And long story short, four days later, we opened up the entire knee. The knee was absolutely perfect. There was nothing in there. You could see no tears no, nothing at all.
[00:30:40] And so then I was like, Oh, maybe there is something to the skin rolling stuff.
[00:30:46] Dr. Catrina Fabian: Wow. That is so cool. Right? It’s so superficial. That’s so cool. I, it makes me think again of my back injury back in February that I thought, cause me being a hypochondriac,
[00:30:59] I
[00:31:01] thought it was muscle injury, I thought it was nerve involvement, my spine, something happened.
[00:31:07] But guess what? I did some weeks later, just some fascial work on myself and I’m great now, no issues back to 100%. And I’m like, Oh my gosh, time and time again, we see it.
[00:31:19] Dr Mike T Nelson: Yeah, and it’s so hard to tell though, because I’ve, I tweaked my back a long time ago, pretty bad after a strongman event. And I figured it was muscular cause I could still move through it till it started swelling up and it had all the signs.
[00:31:34] I didn’t have any numbness or anything, but Oh my God, that was painful. And by like day four, I was like lying on the couch doing nothing. And then I got worried and went in and had it looked at, which is good. And they said, I probably just strained it. And at the time I’m thinking, I just strained everything, could it hurt this bad?
[00:31:51] Are you sure? They did x rays, they did everything yeah, everything else is fine. And it took probably almost three weeks to get back to, quote unquote kind of normal movement again. But it’s a freaky thing because at the time it’s very hard to tell like what is actually really going on.
[00:32:05] Dr. Catrina Fabian: Right? And that’s our job as physical therapists, is to figure that out. And it is a daunting task often. But, I’m sure like with what you do too, the more tests we do, the more information. And so that helps. That helps a lot.
[00:32:26] Dr Mike T Nelson: And sometimes when it’s yourself, sometimes a little bit too much about what could go wrong.
[00:32:29] And that just makes it worse.
[00:32:32] Dr. Catrina Fabian: Exactly. It’s that we know too much for our own good. Yeah. Yes. But yet your
[00:32:38] ability to diagnose anything on yourself is usually just crap. So it’s like you, you have the information of all the things that could go wrong and your massive blind spots trying to figure it out yourself.
[00:32:48] So
[00:32:49] Dr. Catrina Fabian: right. Exactly. Exactly.
[00:32:53] Very cool. You’re welcome. Do you do a lot of visceral massage and work? I’m sure that’s going to depend on where they have pain and that type of thing. The one thing I noticed for breathing, you talked about that basically the insides, the gut area, your visceral area should slide up and down a couple of inches, correct?
[00:33:10] With normal breathing. And what I noticed in a lot of people whose breath breathing was just really bad, they Like their whole visceral area was just like, like stuck. Like it wasn’t going anywhere. So I felt like I was maybe helping with the ribcage stuff a little bit, but it wasn’t until I started doing a lot more visceral work that they actually got a lot better movement.
[00:33:30] And so then I was starting to think, I’m like, Huh, could we have the visceral area would just get stuck? And would it literally start impeding the diaphragm movement then? So like mechanically they don’t have as much space to go.
[00:33:45] Dr. Catrina Fabian: I don’t know.
[00:33:45] Dr Mike T Nelson: That’s just one of my wacky theories.
[00:33:47] Dr. Catrina Fabian: And I’m 100 percent on board with it, though, the way you think I’m like, yeah, that sounds about right.
[00:33:52] I’ve taken one course, and it was by Ramona Horden, who is one of the OG pelvic health therapists, pioneers in our field. Yes. Yes. And so that was a mobilization of the visceral fascia of the GI system. Oh, interesting. Yeah. And so I’ve used some of those techniques and it was really interesting when I started using them and like I could literally cause and then take away someone’s nausea.
[00:34:24] That was, Oh yeah, you definitely can poke in that area.
[00:34:27] What the techniques though, where I had one hand basically on the abdomen, and one, one hand up by the throat. And that was it. Oh,
[00:34:37] Dr Mike T Nelson: interesting. Huh. What’s the mechanism there?
[00:34:42] Dr. Catrina Fabian: I it was something about which I obviously haven’t used this technique in a while now, but it worked great, right?
[00:34:48] But it was something about slacking and then tensioning the fascia along the GI tract but more so The top part not the out not the outlet part
[00:34:59] Dr Mike T Nelson: Yeah, there’s another technique I got from, I think it was from Tom, which was, again, who knows if any of this stuff is really actually going on or not, but I’ve used it a few times where if they feel like they’re really stuck in the mid chest area is to have them have their mouth open, bring their head as far back as they can, assuming they don’t have any restrictions, no dizziness, whatever.
[00:35:23] And then when their head is all the way back to slowly close their jaw. And the thought process is you’re moving your head, but you’re leaving your jaw slack. And then when you close your jaw, you’re pulling up on all this fascia and everything that’s connected to all of those structures. And if people do it, you can definitely feel tension in your neck, but you can feel some weird movement like really deep too, which is interesting.
[00:35:50] Dr. Catrina Fabian: Wow. Yeah. So is the key for something like that to go very slowly, just like if we were doing hands on fashion work? Great.
[00:35:58] Dr Mike T Nelson: So it’s a way of doing it on yourself. And you would start pretty slow. And it definitely feels weird. And I’ve used it on a few people, even myself sometimes. And it definitely seems to help again.
[00:36:09] Who knows what the hell it’s doing, but it definitely feels like it’s moving some structures in that area that are. Almost impossible to probably reach in other areas because of the ribcage and everything else is going on and you know That’s probably for good reason too
[00:36:23] Dr. Catrina Fabian: I know. Yeah, it’s crazy. We even think about the fascial connection between the tongue and the pelvic floor and how, yeah, in utero, we all came from one cord of fascia and then it extended.
[00:36:39] And inform the GI system, for example. So like we clinically we see a connection between TMJ or temporal mandibular joint dysfunction because of tight muscles around the jaw, maybe poor tongue position, restricted tongue movement, and overactive pelvic floor muscles. So those muscles are also presenting with increased tone.
[00:37:00] So it’s Everything can be connected and sometimes it’s not, but often I have, I’ve worked with people for overactive pelvic floor muscles and got those muscles to calm down. And then they tell me later on you know what, I used to have jaw pain and now I don’t anymore. Awesome. Cool. I now I need, now I know to like screen for that as well.
[00:37:23] So.
[00:37:24] Dr Mike T Nelson: Do you find then, it’s a two way street, so working on the jaw, the palate, the tongue, that area has a benefit to pelvic floor area?
[00:37:35] Dr. Catrina Fabian: Yes, I do think so. And so. Like I’ve seen some singers or like wind instrumentalists who are always like breathing in a certain way or using their mouth in a certain way, and then they’re coming with very similar patterns in their pelvic floor.
[00:37:50] And so we also know that the, our whole core is a bringing it back to the abdominal canister, like it is a pressurized system. And so if we are Cutting off all pressure up top. We know that more pressure has to go. It has to exit downwards, right? Exactly and oftentimes it’s going to go through the weakest link
[00:38:17] And
[00:38:19] so in that way, yes addressing fascial restrictions or overactive muscles Can affect much, much down, down the chain.
[00:38:32] Yeah.
[00:38:33] Dr Mike T Nelson: Yeah. That’s super interesting. I know Ron Hroska from PRI had some theories about the different, and Zach’s probably talked to you about this too, that the different structures and the different domes, like the dome of the roof of the mouth kind of mirrors the diaphragm, which mirrors the pelvic floor and kind of all the different connections and things of that nature, which is fascinating.
[00:38:53] Interesting. Interesting.
[00:38:53] Dr. Catrina Fabian: You know what, it is fascinating and it wasn’t until I met Zach that and his colleagues and that I knew about PRA. So I had no idea what PRA was through schooling and my clinical practice and the more I learn about people who have learned through PRA, I’m like, oh, this has influenced a lot of pelvic health practice.
[00:39:15] Dr Mike T Nelson: Oh, I’m sure.
[00:39:17] Dr. Catrina Fabian: Yeah. So, I think of one gal, a amazing Sarah Duvall. She is also a leader in our field. And she’s, I know she’s taken several courses on PRA. And she’s one of those awesome people who lists all of her influences and PRs at the top, to see, where she’s gotten her training and so she’s got an amazing course out for the postpartum and pregnancy population, so, but.
[00:39:46] Dr Mike T Nelson: Very cool. I think I’m in one of her videos in one of her courses somewhere from an interview, so. Awesome. Small world.
[00:39:56] Dr. Catrina Fabian: That’s so cool.
[00:39:57] Dr Mike T Nelson: Related to the. The PRI in breathing, do you, we talked briefly about breathing, but do you find that if people have pelvic floor issues that they probably have some breathing stuff going on too, which again, I could say that probably about most people walking around also, but just because as you mentioned, the diaphragm is that top of the canister.
[00:40:18] That’s what’s controlling some of the pressure, which is going to get transmitted down through and into the pelvic floor.
[00:40:24] Dr. Catrina Fabian: Oh yes. So, we, yeah, I’m constantly assessing someone’s breathing with different movements, just at rest, with a deep breath, and that’s often one of the very first things I work on with someone, because we know that it affects the pelvic floor, and the expansion of the ribcage, and all the core muscles, so, yes, a lot of times we’ll see like paradoxical breathing, where there’s As someone is inhaling they’re actually sucking in their abdomen and their chest is puffing out.
[00:40:57] Yeah, that’s weird
[00:40:58] Dr. Catrina Fabian: huh. And so finding the right cues to get that to calm down and just have them breathe with a good expansion everywhere, a 360 degree expansion is often one of the first steps.
[00:41:13] Do you teach people belly breathing at all? I know if you get into breathing, there’s this huge debate about, Oh, well, all these people are, breathing more from their upper chest.
[00:41:23] That’s why their neck is everything tight. And then they should, you breathe into their stomach and then the other group of people are like, no, that’s like even more dysfunctional and they need rib cage expansion. And we’re, what are your thoughts along those lines?
[00:41:37] Dr. Catrina Fabian: Okay. So I never call it belly breathing anymore, because if someone thinks of belly breathing, they’re probably only going to expand their lower abdomen on an inhale.
[00:41:51] I now only call it 360 degree breathing, 360 degree breathing. I say it all the time all day. And that is getting an expansion at the front of the chest, on the sides of the ribcage, and the back posteriorly, in addition to the belly. And so, that helps people think about breathing the correct way a bit more.
[00:42:16] And so, yes, no, no belly breathing anymore. More 360 degree breathing.
[00:42:22] Dr Mike T Nelson: Yeah, I like the cue a lot better. I actually switched, because for a while I would have people do belly breathing and then I started seeing people coming in who were told they could only do belly breathing and their ribcage was like, like not moving at all.
[00:42:35] And I’m like, well, this isn’t better. This is like not good either.
[00:42:38] Dr. Catrina Fabian: Right. Exactly. We don’t want to replace one dysfunction with another.
[00:42:43] Dr Mike T Nelson: Yeah, and you’d ask them like, well, are you consciously trying to do this or what’s going on? And they’re like, I was told belly breathing is better. And yeah, so I, I understand the, I’m okay with it now as long as I know it’s a progression and then not like the end goal.
[00:43:02] But yeah, I like the 360 degree. Much better.
[00:43:06] Dr. Catrina Fabian: Yeah, and you’re right. It has its time in place. If someone has always called it belly breathing But they are doing what we want the 360 degree expansion then okay, we can call it belly breathing. Yeah, fine, whatever,
[00:43:16] Dr Mike T Nelson: I don’t give a crap what you call it.
[00:43:17] Right, yes, exactly.
[00:43:19] Dr. Catrina Fabian: Or if they don’t know how to expand the belly because maybe it is so restricted with scar tissue or something then okay Sure, we might do some directed breathing into that area and direct the air into specific parts
[00:43:34] Dr Mike T Nelson: Do you find, you mentioned scars from like inguinal surgery and C section. I’ve just noticed over the years that Any midline scar sometimes causes really weird stuff to happen, and I don’t know why. So any sternal scar, and obviously I have one from open heart surgery when I was four and a half, so I have a huge scar c section scar, so my little intake list of when everything else is weird and I can’t figure shit out I go back and I use a dolphin, which is more of a microcurrent, treat the scar, and then go back and do literally the same thing that I just did to them before.
[00:44:12] And 90 percent of the time it works again. I don’t know why that is, or if you’ve seen that, or if you have any thoughts of what’s actually going on. Cause we know scar tissue is different, it’s not bad, like it is a good process to hold you back together. And I’ve seen other people have massive scars and no issues at all.
[00:44:33] Dr. Catrina Fabian: Right. Well, I’m curious, is that similar? I don’t know if you know what an alpha stim is, but it sounds similar because that’s also a microcurrent.
[00:44:42] Dr Mike T Nelson: Oh, it might be very similar.
[00:44:43] Dr. Catrina Fabian: Yeah, and so there are two, yeah, two pros. Two handheld
[00:44:46] Dr Mike T Nelson: devices, pass a little current back and forth.
[00:44:49] Dr. Catrina Fabian: Yeah.
[00:44:49] Dr Mike T Nelson: Yeah. Probably very similar.
[00:44:51] Yeah. Yeah.
[00:44:52] Dr. Catrina Fabian: Cool. Yeah. So I have I’ve done that on a scar and then just feeling it before and after it’s completely different. And then the patient can, yeah. And they’re like, Oh, I move so much better now. Or my abdomen feels looser.
[00:45:04] Yeah.
[00:45:04] So I don’t know the mechanism. I honestly I don’t either.
[00:45:10] Dr Mike T Nelson: I have no idea.
[00:45:11] Dr. Catrina Fabian: This is one of those things that I just need to be honest with my patient. Yeah,
[00:45:15] I don’t know. But
[00:45:17] Dr. Catrina Fabian: usually they’re willing to try anything that works. And as long as we rule out all the contraindications and everything, obviously,
[00:45:22] Dr Mike T Nelson: Oh, sure.
[00:45:23] Dr. Catrina Fabian: Potential benefit and very little to no risk. So they’re usually up for it.
[00:45:28] So I don’t know what the mechanism is. I don’t know if this If it’s like something to do with time because we know that like fashion needs time to be affected. And so usually the process with the probes is slow. It’s 10 seconds on each spot, for example. So
[00:45:48] yeah, I’ve always been curious. I even had it went so far as to have an NDA with the creator for a full year.
[00:45:53] And I, super smart dude, knows a lot of stuff, was getting some crazy results, but I couldn’t follow what was going on, I have no idea. Definitely seemed to work though, I don’t know. Right,
[00:46:06] Dr. Catrina Fabian: I
[00:46:07] Dr Mike T Nelson: know. It’s always wild to me how you can find things that work, but yet we’re so behind on trying to figure out mechanisms of how.
[00:46:16] But at the same point, like. What I like about your stuff too is that you’re willing to try things to see if they work even if there Isn’t really an answer right because I think that’s the definition of being a good clinician is you know what the upside is you know? What the downsides are you’re not gonna do anything?
[00:46:31] That’s obviously has a lot of risk or things of that nature But at the end of the day The person’s paying you for a result. They’re not paying you to run a randomized, blinded, placebo controlled trial. That’s research, and by all means, yes, have a sham control, and all that type of stuff, too. But it’s just, it’s a little bit of a different mindset.
[00:46:50] So I think sometimes when People are clinicians. It’s hard because you may be doing things that, are very effective and you’ve seen it time and time again and have no idea as to what’s going on with the mechanism.
[00:47:03] Dr. Catrina Fabian: Right? Like I was one of the things that my very first mentor in the field taught me was that.
[00:47:10] research. Unfortunately, it’s amazing. And Dr. Mike, you’re a huge research whiz and know so much more on it than I will ever, but it’s such a great tool, but unfortunately, it’s often like 10, 10 years behind clinical practice. So there are things that we need to try that we just don’t know the mechanism behind or like the statistics on yet.
[00:47:32] But we keep trying and then yes, we get it. Yes, research will show one day,
[00:47:36] Dr Mike T Nelson: yeah, it’s getting there. I know that’s a whole lot of who’s going to pay for it and who’s going to run it and all that kind of stuff too. So yeah it’s a never ending battle because as like we do one research on one area, you end up with 15 more questions you want to look at too.
[00:47:52] So it’s this very slow, methodical step wise fashion. And then I joked with a buddy of mine that. At this point, I think I have more questions than I have answers than I’ve ever had before. Hopefully I’ve accumulated a little bit of knowledge, but as you figure that one next thing out, then that has 12 different questions of something you never thought about before.
[00:48:11] So it’s a, it’s a never ending cycle.
[00:48:15] Dr. Catrina Fabian: Oh, I know. And oftentimes that, yes, that pops up in clinical practice where it’s like, Oh, I just wish I knew more on this. Or I wish I could study like patterns across the population and see if this is actually a pattern.
[00:48:28] Dr Mike T Nelson: Definitely.
[00:48:29] Dr. Catrina Fabian: Yes. Yeah. That happens a lot.
[00:48:31] Because all I see as a clinician are clinical patterns at this point. And I’d love to be able to have some absolutes or, I know that’s not possible, but more absolute know, knowledge.
[00:48:43] Dr Mike T Nelson: If someone is listening, if we make this kind of more practical, is there things in your clinic, in your practice that they should both first off, avoid?
[00:48:54] And then the next question would be things they should maybe add or do more of.
[00:48:59] Dr. Catrina Fabian: Alright, so this would be to improve someone’s overall pelvic health?
[00:49:03] Dr Mike T Nelson: Yep, overall pelvic health. Yeah, I mean for people who maybe don’t have any issues now, but they’re like, ah, I know this could be a thing, later. So I want to Make sure I take a better path.
[00:49:14] Dr. Catrina Fabian: 100%. Okay. So, the first thing we talked about a lot is breathing. So maybe even take a video of yourself breathing from different views, the front, the side, and see if you are getting 360 degree expansion. If you are, that’s great because we know that your whole abdomen, abdominal muscles, and pelvic floor muscles are probably working well.
[00:49:36] The next thing is to honestly hydrate. Yeah hydrate adequately the number of times i’ve had to And for my patients on normal hydration or yes is, it’s often in a day. And so that will set up good bladder health and that will affect quite a lot.
[00:49:58] Dr Mike T Nelson: Do you use electrolytes with hydration?
[00:50:00] Or do you recommend water or any certain amounts you recommend?
[00:50:03] Dr. Catrina Fabian: So I usually say, so on the topic of electrolytes, it depends if someone is getting a lot of fluid in and they’re still showing signs of dehydration or they’re reporting that then I’ll say, oh, have you tried using some electrolytes?
[00:50:20] That usually helps. That usually works great. And then as far as the amount of water, I will usually preface and say that everyone’s fluid retention is very different. So some people can drink the same amount of water as the next person, but still show signs of dehydration. So a good rule of thumb per urologist is you take your body weight in pounds, you divide it by two, and that’s a good starting amount for ounces of fluid.
[00:50:48] Then you adjust from there and also check the color of your urine. Unless it’s affected by medication or food intake.
[00:50:59] Dr Mike T Nelson: Perfect.
[00:51:00] Dr. Catrina Fabian: Yeah And the third thing is a little bit more like woo or holistic We didn’t
[00:51:07] Dr Mike T Nelson: talk about any woo stuff. So you’re good
[00:51:11] Dr. Catrina Fabian: Right, and but that would be you know, if someone is experiencing chronic stress or anxiety or has traumas that they have not healed from but would like to, it would be amazing to start that journey because we know that there is a lot of research on this, that there’s a big connection between overactive pelvic floor muscles and chronic stress, anxiety, and all types of trauma.
[00:51:41] And we know that bladder symptoms Sexual dysfunction and bowel function can be greatly impacted by acute or chronic stress and anxiety. You think those are, I know this is a vast oversimplification, but you think one of the mechanisms there is just this overall sympathetic response to add tension and to go more into a flexion type response that’s partially responsible for that?
[00:52:11] Yes, I think that is part of it, that positioning, or if someone is in pain or they’re anxious that is affecting muscle lengthening and positioning of even the pelvic floor because we’re probably getting some tilt of the pelvis. But then also we know that organ functions are so dictated by parasympathetic or sympathetic nervous system and so if someone is still in survival mode their body’s gonna Do what it needs to do that, and that probably means holding in someone’s poop, not letting them urinate, and not being able to have sex without pain, or,
[00:52:49] sure.
[00:52:50] So, yes.
[00:52:52] Awesome. Are there some things that people should try to avoid?
[00:52:57] Dr. Catrina Fabian: To avoid? Ooh, that’s a good one. The first
[00:53:01] Dr Mike T Nelson: thing I think of is what we talked about with every lift above 9RM in your gym, you’re doing a hard Valsalva where your eyeballs look like they’re gonna pop across the room.
[00:53:11] Dr. Catrina Fabian: Yes, I would highly recommend avoiding that. Yes, it’s avoid holding your breath through. a workout. Avoid tension in your body with movements like jumping rope all the time. Avoid straining. That’s the biggest thing in your daily life because that will put undue stress over the pelvic floor. And that also includes daily activities like peeing and pooping.
[00:53:35] Don’t strain during those.
[00:53:38] Dr Mike T Nelson: Perfect. Anything else?
[00:53:41] Dr. Catrina Fabian: No, that’s pretty much it. I found your HRV course fascinating. It was great. Thank
[00:53:45] Dr Mike T Nelson: you so much for doing that. I really appreciate it.
[00:53:48] Dr. Catrina Fabian: Yes. I thought it was awesome. And you simplify complex ideas very well, which is great. Thank
[00:53:56] you.
[00:53:56] Dr. Catrina Fabian: You’re welcome.
[00:53:57] And for me, it’s been great because if my patient has like an aura ring or something, I can give them some education on their HRV or match those patterns. Thanks. To what we’re seeing in their pelvic floor. So it’s been good.
[00:54:11] Dr Mike T Nelson: Yeah, I would imagine as a Clinician you could do a lot of the right things you could do some manual work You can send home with their good exercises all that stuff.
[00:54:19] But if they’re Running around just stressed out of their mind, like their body is literally going to go back to the same state that they were in before. That’s just how it works, unfortunately.
[00:54:33] Dr. Catrina Fabian: Exactly. Yes. That is always a thing to consider. For me I need to be careful that it’s not a cop out and that I’m, not just saying Hey, make sure, make sure you’re not stressed, but like actually give them actionable things that they can work on to manage their stress well.
[00:54:47] And understand that, okay, you might just have more symptoms in periods of stress.
[00:54:54] Dr Mike T Nelson: Awesome. Well, thank you so much for sharing all your tips and techniques and everything there. Really appreciate it. I know you’ve got a lot of great stuff on Instagram and everything else, so tell us what services you have, where you’re located, and what do you, people can find you at.
[00:55:10] Dr. Catrina Fabian: Alright, you can follow me on Instagram at powerinthepelvis, no spaces, no periods. I also have a website, powerinthepelvis. com, and so I do treat people in person one on one in Las Vegas, Nevada, as well as virtually.
[00:55:31] Dr Mike T Nelson: Awesome. And if people want to get a hold of you, is the website or Instagram the best place or either one all go to the same location?
[00:55:37] Dr. Catrina Fabian: Yeah, you’ll see my contact information on both. And so emailing me at Katrina with a C, Katrina at powerinthepelvis. com is the best way to set up a consultation with me. And so that we can start working together. We’ve got a great gym where I am and I love seeing all types of people from very active people, sports minded people, all the way to the postpartum, a mom who needs to function better in their daily life.
[00:56:05] Dr Mike T Nelson: Awesome. And you have an online option too, for people who are not in the Las Vegas area, because I, I’ve referred several people out over the past years, nobody recently, but it’s one of those things where once you start talking to people and it’s something that most people will never mention, even on the first session, like sometimes if you’re really doing stuff and you get into it, they will but I don’t even think i’ve had a maybe two people who came in originally and said that yeah This is going on. So it’s usually Something that is happening a lot more than what people are talking about it So if people are having symptoms and having things going on Then there’s an online option.
[00:56:43] They should definitely look you up.
[00:56:45] Dr. Catrina Fabian: Yeah, that’s right No, I thank you so much for having me because building awareness is the first step and you know I still have patients referred to me and they tell me I had no idea that this existed Like I don’t need a surgery or medication. That’s awesome So I really appreciate you bringing awareness to this and helping us people out with very, conservative options
[00:57:05] Dr Mike T Nelson: Yeah, I always think surgery can be definitely useful as a time and a place for it but If you can exhaust all your non surgical options first, like my biased opinion, just do that first.
[00:57:17] Right.
[00:57:18] Dr. Catrina Fabian: 100%. And yes, medication and surgery have their place. And my job is just to inform you how, to, know the side effects have conversations with the surgeon or prescribing physician because they can be adjuncts to our treatment. And so, yeah, there are times where I do want people to go that route, but oftentimes.
[00:57:37] They, they can just do physical therapy or rehab. So awesome. Well, thank you so much for all your time. I really appreciate it. Thank you.
[00:57:47] Thank you so much. That was great.
[00:57:51] [00:57:52] Dr Mike T Nelson: Thank you so much for listening to this podcast. Huge thanks to Dr. Katrina for all the wonderful stuff and sharing all of her wealth of knowledge.
[00:58:00] As we mentioned, she does do online consults, so definitely check her out, especially if you’re in the Vegas area, you can check her out in person. We’ll put all of her wonderful information, Instagram, everything else, down below. So huge thanks to her for coming on to the podcast. If you’re looking for a boost from ketones without having to do a ketogenic diet, check out Tekton.
[00:58:25] We’ll have a link down there below. I’ve also used it when fasting. Lately I’ve been doing a little bit longer fast about once per week. So check them out below. Thank you as always for listening to the podcast. Really appreciate it. If you know someone who may enjoy this podcast, please forward it on to them.
[00:58:44] I hit the old subscribe and and all the wonderful things to help us out with. The old algorithm goes a long way to expanding the audience and to keep continue to getting More guests for you each week at no cost. So thank you so much. Really appreciate it Talk to all of you next week
[00:59:05] Personally, I don’t care for puppets much. I don’t find them believable. I don’t believe you!
[00:59:11] This podcast is for informational purposes only. The podcast is not intended as a substitute for professional medical advice, diagnosis, or treatment. You should not use the information on the podcast for diagnosing or treating a health problem or disease or prescribing any medication or other treatment.
[00:59:28] Always seek the advice of your physician or other qualified health provider before taking any medication. Or nutritional supplement. And with any questions you may have regarding a medical condition, never disregard professional medical advice or delay in seeking it because of something you have heard on this or any other podcast reliance on the podcast is solely at your own risk information provided on the podcast does not create a doctor patient relationship between you and any of the health professionals affiliated with our podcast.
[00:59:54] Information and statements regarding dietary supplements are not intended to diagnose, treat, cure, or prevent any disease. Opinions of guests are their own, and this podcast does not endorse or accept responsibility for statements made by guests. This podcast does not make any representations or warranties about guest qualifications or credibility.
[01:00:12] Individuals on this podcast may have a direct or indirect financial interest in products or services referred to therein. If you think you have a medical problem, consult a licensed physician.






Leave A Comment