Welcome back to the FlexDiet Podcast! In this episode, I sit down with Dr. Allison Brager, a PhD neuroscientist, CrossFit athlete, and military sleep expert, to unpack everything you need to know about the science of sleep.
We dive deep into the phases of sleep, circadian rhythms, and chronotypes, plus we take a critical look at popular sleep advice—what’s backed by science and what’s just noise? Dr. Brager also shares fascinating insights on sleep in the military, how to optimize recovery for athletes, and the biochemistry behind quality sleep.
Looking for practical strategies and the best sleep supplements to improve your rest? We’ve got you covered.
- Tecton Life Ketone drink! https://tectonlife.com/ DRMIKE to save 20%
- LMNT electrolyte drink mix: miketnelsonlmnt.com
- Dr. Mike’s Fitness Insider Newsletter: Sign up for free here.
Flex 4:
Check out Dr. Brager’s top recommendations for sleep supplements.
Available now:
- Grab a copy of the Triphasic Training II book I co-wrote with Cal Deitz here.
Episode Chapters:
-
00:51 Deep Dive into Sleep
- 01:33 Top Sleep Supplements
- 02:11 Sponsors and Personal Updates
- 02:56 Conversation with Dr. Allison Braeger
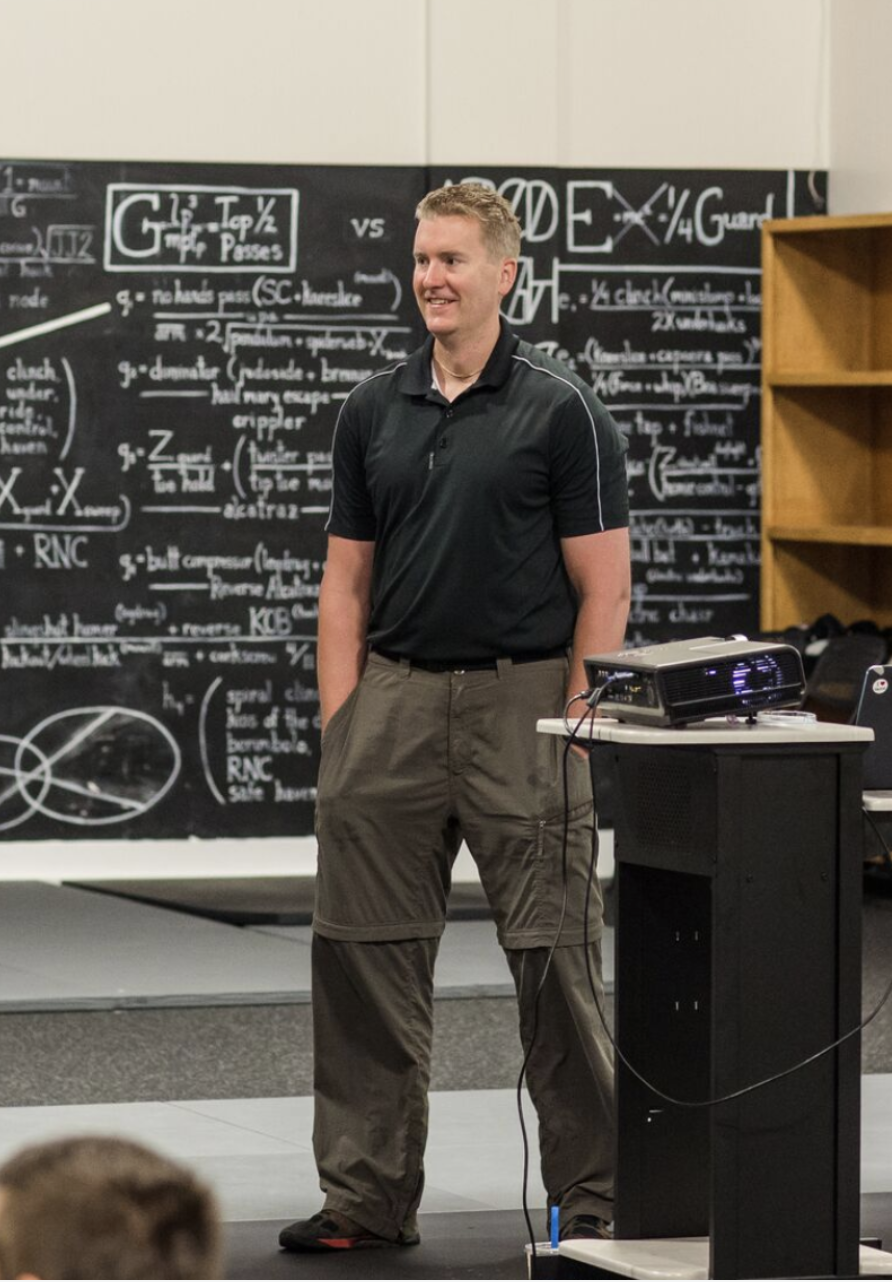
- 03:32 Teaching at West Point
- 04:41 Chronotypes and Sleep Advice
- 09:40 Training and Sleep Optimization
- 13:48 Impact of Travel on Athletes
- 26:09 Wearables and Sleep Research
- 33:22 Intense Competition Experience
- 34:27 Lab Testing Mishaps
- 35:03 Competitive Nature in Athletes
- 36:09 Debating Sleep Stages
- 39:22 Heart Rate Variability and Sleep
- 47:00 Challenges in Sleep Research
- 49:38 Frustrations in Academia
- 55:50 Alternative Research Paths
Flex Diet Podcast Episodes You May Enjoy:
- Episode 283: Unlocking Better Sleep and Stress Reduction with Dr. Dan Cohen of Soltec Health
- Episode 273: Unlocking Better Sleep: Insights and Strategies from Dr. Chris Perry
Connect with Dr Brager:
-
Instagram: @docjockzzz
- “Meathead Unraveling the Athletic Brain”: Purchase on Amazon
Get In Touch with Dr Mike:
Rock on!

Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
Greetings and welcome back to the FlexDiet Podcast. I’m your host, Dr. Mike T. Nelson. On this podcast, we talk about all things to increase performance, add muscle, improve your body composition, and do all of it within a flexible framework. And today on the podcast, we’ve got my good friend, Dr. Allison Braeger, and we are talking about all things related to sleep and much, much more.
So you may have heard of her before. She’s a PhD CrossFit athlete. I’ll let her tell you about her new work. She’s doing in the military here Which is great and just all around wonderful person. I got to meet her in person again a while back and Today we’re doing a deep dive on all [00:01:00] things related to sleep and everything from what are the different phases of sleep?
What is a critique of some of the popular sleep advice? Chronotypes and how they are related to sleep. Travel and consideration of your circadian rhythms. Competitive stories about how you can use sleep to help with training and everything else. So, I tried to do a little bit more of a deeper dive here on all things related to sleep and, just overall training.
performance and health also. And if you want to know what are the top supplements that Dr. Breger recommended related to everything related to sleep, you can check out the Flex4. That was the question. And if you’re on the exclusive insider newsletter list, you’ll get access to her answer there for the kind of the top recommendations for sleep supplementation.
If you’re not, you can still get on it. So go to the link down [00:02:00] below and you will be able to hop on to the Insider Newsletter, which is free, and we will directly send you the answer to that question of the top sleep supplements. Our other sponsors are Element. I’m recording this down here in El Cuyo, Mexico, so you may hear birds and waves and stuff in the background still.
And we brought down a whole bunch of Element to have while we were down here, since it is It’s quite hot and humid. I’ve been doing some running in the morning, been doing some kiteboarding when there’s been wind, and it’s always nice to stay hydrated, and I’ve realized it just makes a huge difference, especially if I’m coming from the cold of Minnesota down here, and I’m not super acclimated yet, just having more electrolytes, especially sodium with fluid, makes a huge difference in just overall energy levels, too.
Dr Mike T Nelson: Also check out ketones from our friends at Tekton, And much more. So without further ado, here’s a podcast with Dr. Allison Breger.[00:03:00]
Welcome to the podcast doc. How are you doing?
Dr Allison Brager: Oh, I’m doing great. It’s good to see you again. It’s been a while.
Dr Mike T Nelson: Yeah, we finally got to meet in person at Jason Leiden’s event in Connecticut, which was Is that a year and a half ago now?
Or is it a year in September? I lost track of time already. Oh,
Dr Allison Brager: it’s over a year. Yeah, it’s October of 2023.
Dr Mike T Nelson: That’s right. Yeah, that’s wild. Crazy. Yeah, and I know you’re not traveling as much now. You have a big teaching gig. I don’t know if that’s public knowledge yet or not.
Dr Allison Brager: Oh, no, that’s fine. Yeah. It’s funny being like the army’s jet lag sleep expert, but I’ve been a practitioner as much as I’ve been a principal investigator in it.
But yeah, I’m going to go to West Point for three years and teach cadets hopefully instill good sleep habits and practices to set them up and their, future soldiers up for success. But I know that’s a tall order because other sleep scientists have tried to in the past [00:04:00] with no success, but I don’t know, maybe this generation’s different.
Dr Mike T Nelson: And are you teaching purely on sleep or are you teaching on many different topics?
Dr Allison Brager: No, so I’ll be the program one of the program leads for this course that every cadet has to take it’s called the psychology of leadership course. Essentially it’s psychology within the lens of military operations so applying all the principles to some element of, conducting warfare or manipulating.
The the character and the, the psyche of war through the lens of psychology.
Dr Mike T Nelson: Got it. Got it. Related to sleep, like for, I’ll phrase this in two ways, for new people coming in to let’s say even that school versus. People have been maybe special operators for 10 years. Well, how would your advice be different for those two groups?
And what would you tell [00:05:00] them?
Dr Allison Brager: That’s a great question. Honestly, in terms of sleep amounts, sleep quality, there really are no differences, right? Because whatever your sleep set point is based on truly genetic factors, like that’s what people don’t realize is. 80 percent 90 percent of sleep, just like most other physiological processes is tied to a genetic footprint.
Your set point is your set point and that’s pretty much established around the ages of 18 to 19. But I think. Where the difference lies is the timing of sleep, right? Like cadets don’t really have as much control over their schedule, like every single minute of their day is mapped out.
And they might naturally be. Evening people like I am and forced to wake up early. And in fact, there’s going against their natural biology because teenagers naturally [00:06:00] have delayed sleep phases and rhythms, whereas with special operations, like they’re going to have more control in some cases when they’re not on the X over their schedule.
So, they can figure out cause we give them the flexibility to like. When they’re back in the rear, they can be as optimal as they want, as long as they get their work done. I would encourage them to take advantage of what they know they are as a person, whether they’re a morning person or an evening person, and use that to their advantage, and use that as their, more or less combat power.
Whereas cadets, I feel like they just they’re always in. a time point of mitigating things. So, trying to keep the band aid on so that it doesn’t rip off.
Dr Mike T Nelson: Got it. And you’re talking about like chronotype, how would someone who’s listening, how it, if they don’t do any genetic testing or any other testing, how would they know what their chronotype is?
I think most people know, they just never been given [00:07:00] permission to figure it out,
Dr Allison Brager: yeah, no, that is that’s a great question. There is a questionnaire. We actually Jason Lydon and I were part of power monkey at power monkey camp, I make everyone fill out the questionnaire.
It takes maybe 25 minutes, but it’s called the morning evening questionnaire. And it has 20 different questions. They’re all written very similarly, and some are like repeated but the words are switched around to, create internal validity. But that’s honestly the tried and true way like having the genetic test is a nice to have.
But a must have is actually this morning evening questionnaire. And from what we know, like 80 percent of the population are intermediate chronotypes, meaning they usually perform best when they wake up at 7 a. m. And then go to sleep normally around 11 p. m. Whereas vampires like me I like to wake up 839 and go to bed a little after midnight.
That’s 10 percent of the population. [00:08:00] It’s not cognitive dissonance because my parents are like that too. And I do have the genetic sniff. I looked it up when I did genetic testing for it. And then the other 10 percent are morning people.
Dr Mike T Nelson: Plasticity is in there. So let’s say you’re more of the evening type, like yourself can you really push yourself the other way by getting sunlight and using light cues and feud cues and all that kind of stuff?
Or is that something that just runs on top of it? Like the second you start removing those things, you just slide back to where you were before.
Dr Allison Brager: That’s a great question. No, you have to, it’s, the technical term is circadian reentrainment. And in order to reentrain, you have to keep introducing those stimuli at the
Dr Mike T Nelson: start.
So it’s got to be a constant thing to try to override the underlying program is how I think about it. Yeah,
Dr Allison Brager: because the minute you’re removed from that, you go back. Perfect example When I was a company commander I used to have to work out [00:09:00] really early in the morning, my brigade commander.
So I have to wake up at like 4 AM to be 5 AM. My preferred workout time is 7 PM at night. Like I working a full work day and then to me working out as like a cathartic release. But I had to. Not only was I getting sick more often and feeling more fatigued and all that, but even when I kept everything consistent, like the minute, there’s a week or two, he wasn’t there.
So we didn’t work out with him. Like the minute I switched back to my normal schedule, like my clock, it was immediately back there. But then when I had to go back on, it was awful.
Dr Mike T Nelson: Do you find that optimal training times where people want to train or feel best and have the best performance is also related to that.
I feel like athletes I’ve worked with who have a later chronotype almost All across the board, left to their own devices. They all tend to exercise later in the day. [00:10:00] I feel like the early morning people almost exercise more earlier in the day. Like when I started my own business, like the two big things for me were not my two goals were not set an alarm on Monday and then be able to train between one and three in the afternoon.
That was like my two goals.
Dr Allison Brager: Yeah, no, absolutely. So I think. I think people pre select into sports because of chronotype, and I know that’s really wild and far fetched, but you think back to when you were a kid, unless you had parents who like said, my son’s gonna be a baseball player, my daughter’s going to be a gymnast.
I look now because of power monkey, right? All of us who are coaches at power monkey, we’re professional athletes at some point in our careers, whether, like Jason was a pro basketball player. I did CrossFit. I also tried to make the Olympic team and track and field Dave and a bunch of others were [00:11:00] weightlifters and gymnasts.
When did we practice? We all practiced late at night. I was a gymnast too growing up. Before I was a pole vaulter, I did gymnastics for 18 years. So like my gymnastics practice ended at 9 PM every night. I would go home, eat simultaneously, eat dinner and go to homework and get to bed so I could get eight hours of sleep.
And so I think that’s why I’ve, started doing well in those. Because my body is peak to perform at those times of the day. And it’s still true today, right? Like I hate working out in the morning. That is the last thing I want to do in the morning is workout. Yeah,
Dr Mike T Nelson: no, that’s super interesting because I have had a few athletes where.
It’s weird for them to have to perform at different times. Like a lot of times you may have like baseball, right? So you may have games in the afternoon, but if you’re getting into playoffs and world series, those are almost always evening games too. So then you’ve got that [00:12:00] ability to have to switch back and forth.
But if you’re talking about American football. You’ve got potentially games in the afternoon, but then you might play Monday night, so you have an evening game too. So any thoughts of trying to, if you have to switch back and forth between the two, because your sport is scheduled at that particular time, is there things you should do leading up to that?
So for example, if take American football, cause the Vikings are playing a playoff game coming up, they’re playing on Monday night. Is there something they should do to get prepared for that week? They’ve got one week of time. And they’re used to normally playing on the afternoon schedule.
Dr Allison Brager: Yeah.
So we’ve done a little, I’ve done a little bit of work with not so much NFL teams, but collegiate teams I’ve worked with in state in the past. And then LSU is that’s essentially like when those. big playoff moments like playoffs, especially that’s what you want to do is start delaying everything like you don’t want to have a huge delay, but maybe 30 minutes at a time leading up [00:13:00] to the time that coincides with that game.
Now during the regular season, it’s a little bit more difficult, like really during the regular season, you have to use like Mitigation factors such as we group them as like light noise and temperature. So how do we manipulate those things in your environment to quickly shift your schedule to include like even caffeine and melatonin, right?
Like those can shift your clock, but obviously they can shift alertness levels too. But when it comes to playoffs yeah, that’s when you want to gradually restructure everything till later. So you’re not just relying on like pharmaceutical aids and that quick acute effect you’re going to get from sunlight.
Dr Mike T Nelson: Do you find in And I think you might’ve had a post on this a while ago, like because of the way they’ve changed college sports now, it’s basically, they’re doing a lot more travel than they’ve ever had to do [00:14:00] before. Have you found that. presents like a whole host of problems. Like I would love to see, maybe this study is being done like a retroactive study, just looking at something simple, like injury rate, between before they had this kind of set schedule.
Now they’ve got this kind of more crazy schedule. I would have to imagine the injury rates would go up. And again, I’m just guessing on that.
Dr Allison Brager: Yeah, so that’s my hypothesis, too. I think it’s too early to tell, but you’re right I think Mike retroactively.
Dr Mike T Nelson: Yeah, post hoc, yeah.
Dr Allison Brager: Yeah, we’re going to see that in injury rates.
We’re going to see that in just burnout. Really, I feel like the only thing not forcing psychological burnout now in these college athletes is the NIL. That might be the one saving grace. The fact these athletes are getting paid, they’re less likely to be psychologically burnt out because there’s money now attached to it.
Dr Mike T Nelson: Yeah, but then you also have them transitioning between more teams too. If you’re a coach, you used to be able to I [00:15:00] probably got these athletes for four years. Now it’s shit, I don’t know.
Dr Allison Brager: Yeah, exactly. Well, we did do so years and years ago. My, my cousin’s an ortho surgeon in Cleveland and he’s worked with the Cleveland Browns and the Pittsburgh Steelers.
And so we were actually able to get access to like MSKI data. And then we actually got access to some concussion data too that. We’re still working through it’s like one of those things we retroactively got because it was after the NFL lawsuit because before that they were very close hold about yeah,
Dr Mike T Nelson: they wouldn’t share data with almost anybody have
Dr Allison Brager: to.
So, yeah, it was what we found is like teams on the west coast. Are more circadian, they’re set up for circadian advantage in terms of winning throughout the season because they’re playing games that more often coincide with their peak athletic time and the early evening or late [00:16:00] morning compared to East Coast teams.
And then if you look at injury rates between West Coast and East Coast teams throughout the regular season, East Coast teams get injured. five times as often. If you just look at whatsoever from the starting roster and the amount of weeks that those players on who are starting end up on injury reserve.
It’s that consistent. Now, this is an analysis we did in 2013, 14, and 15, as they were transitioning to the tackling roles, right? But I would still bet it holds true today that West coast teams get injured less often than East coast teams.
Dr Mike T Nelson: And do you think part of that is they’re just more performing at more of an optimal or peak time, or is it because of the location and then they have to travel?
There’s less. detrimental effects upon their circadian rhythm so their sleep is better even when they have to travel more?
Dr Allison Brager: So that’s a great question so we actually controlled for that we look [00:17:00] at the amount of times that a team was traveling and if you look at like the amount of time zone pops between east and west travel and west and east travel between the two it’s actually pretty similar and so if you’re just controlling for the team’s biological time because Operating on this hypothesis that they’re not going to have time to adjust, which is true, right?
The day before and they’re in that time zone and they haven’t adjusted. But when you’re just controlling for that you still see that as a factor.
Dr Mike T Nelson: What are your thoughts on, so now I’m just using the NFL as an example, cause it’s more top of mind. They had some games in. Central America, which, generally are on similar time zones, but they have big games in London. And I know just from people in the industry and being in this field, there seems like there’s a debate of, and you even see this in high level athletics of let’s do everything as [00:18:00] normal as we can at home and we’ll do the flight a little bit later, we’ll get there, maybe the night before and the games the next morning.
And yes, that night of sleep is going to suck, but we had all this good time at home and then we’ll go perform. And then you see the opposite of other teams are like, well, we’re going to get there because it’s usually early season game. We’re going to get there six days early, get everything ready. Try to get acclimated to the time zone there and then roll in that way.
Dr Allison Brager: So I think either approach. Is equally as good. I think the bad approach is somewhere in the middle.
Dr Mike T Nelson: Yeah. I think in the middle is where you get hosed.
Dr Allison Brager: Yeah. Cause so we’ve done these types of studies. And so I think, that’s most of my career has been. Spent doing preclinical sleep physiology
studies,
and we actually did a very similar study in mice.
Oh, cool.
People think that’s not an appropriate [00:19:00] model, but it actually is because even with mice being nocturnal, like the neuroanatomy and physiology of their sleep system is conserved across evolution. Same as it is in a human. And so we find like when you’re shifting, when you’re advancing mice and their schedule by six hours at a time, it takes about three to four days for that shift to fully occur.
But the dynamic part of that shift is on days three and four. So you get a little bit later. Yeah. So you get a little bit of a shift on days one and two, but for the most part, like the circadian system is still holding on to a schedule and then around days three and four that’s when you get this huge drop off and it’s like this, the circadian system can no longer function and it.
starts its process of adjusting. So right by day [00:20:00] six, the animal has now effectively re trained. But the real rate of re entrainment is happening between days three and four, not so much on days one and two, like people would think. So, that’s why I guess, if I had to choose between the two, yeah, sure.
I would do the six days, right? But I know it seems like they don’t really have those luxuries when they have those games because it seems like they do that and then, they play that Sunday and then they’re playing again that Thursday.
Dr Mike T Nelson: Yeah, that’s the thing is either way on the back end of that, you’re a little bit hosed, especially if you have an early game.
Dr Allison Brager: Yeah. And that’s one of the things I tried to convey to Michigan State when I was working with them. So it was right when the Big Ten merged with the Pac 12 and they were doing a game out at University of Washington. I was like, Okay. This is a great plan you came up with, like truly they came up with a great plan leading up to the game, but then after the game, [00:21:00] like that night, they can take a red eye back to Michigan.
I was like, okay, yeah, I understand. You got to get back to work, but you’re gonna get hosed. You’re gonna get, you’re gonna get absolute, like you’re increasing risk for injury. So they actually went and they changed the plan. Where they just did the film the next day in the morning, and then they flew back that afternoon, because otherwise, I think they really would have been struggling that week.
Dr Mike T Nelson: Yeah, and the delay in the circadian rhythm kind of makes sense, because I’m thinking back I either would If I was teaching overseas or something like that, I would either stay for five to six days or on rare circumstances, especially more early on, I would end up being really short and the really short ones weren’t that bad until I got home and then it felt like it was horrible.
But the ones that were like three to four [00:22:00] days were just the absolute worst because you never felt like you got back to normal. And then when you get home, you still feel like a trash.
Dr Allison Brager: Yeah. Yep. No, absolutely. Yeah. I was earlier this month I was competing in Budapest at the master’s world championships for it’s not CrossFit it’s called functional fitness, so it’s like the athletic organization trying to make.
Functional fitness is sport in the Olympics, so there’s like blocks you have to check.
Dr Mike T Nelson: So like a grid athlete, or I don’t know if that’s still around.
Dr Allison Brager: Oh, the grid just came back. No, this is. Oh, it
Dr Mike T Nelson: did. Okay.
Dr Allison Brager: It, I’m going to be like, it’s pretty much, it’s CrossFit. Okay, it’s a
Dr Mike T Nelson: different name.
Dr Allison Brager: It’s just called international functional fitness, but it’s very, so essentially it takes all the domains of CrossFit.
So there is a strength event. There is a skill event and it’s oh I
Dr Mike T Nelson: did hear about this. Yeah standardized too, right?
Dr Allison Brager: Yep. It’s
Dr Mike T Nelson: [00:23:00] yeah
Dr Allison Brager: A power event, a stamina event and an endurance event and like Last year when I did the world championships is in Vancouver and I flew home the next day like the next morning, Competition ends.
So all the countries get together. It’s like cool runnings. We like
nice
Vancouver and had a few beers Vancouver’s early flew home. I felt like absolute ass for two weeks. And then I got sick, right? This time did the same thing, right? All the countries got together at an after party, but then I stayed in country for another three, four days and I had an easy transition home.
So yeah, you either have to go home. I think in those circumstances you have to wait your time out.
Dr Mike T Nelson: I finally got wise to that. I also realized too, like teaching two days in a row by myself, not too [00:24:00] bad. Three days in a row. That was definitely the limit. If you’re like the only one there. So I got wise on if it ended on a Sunday night, like Monday, I would just not schedule anything.
Like I go walk around, do whatever, get some food, like no cognitive tasks, find a float tank that night. Anything but anything that I had to do something because I found every single time I had to do something it was horrible I was toast anyway And then when I came home, I got sick. So I’m just like, ah, it’s not worth it.
Dr Allison Brager: Absolutely.
Dr Mike T Nelson: The people who were training later at night, and I’ve had this issue in the past, cause I’ve had to train in the evening in the past, especially when I was doing my PhD, I had a hell of a time downregulating after training. And this would be like, I pulled caffeine out. I would not get real amp for lifts.
I would do some strength training. It was even not as much fun, even tried taking out the death metal and it didn’t matter what I did. It was just [00:25:00] something about the act of lifting anything moderately heavy. It would be two to three hours before I could get to sleep. Is that different per chronotype, do you think?
So if someone is more of an evening type, are they better at downregulating after that then?
Dr Allison Brager: So I don’t think we’ve actually looked at that. I know they’ve finally done like dose response curves in terms of what is the optimal amount of time before you sleep for like high intensity training and it doesn’t have to be a true hit workout.
Like strength training to me falls in that category because of,
Increasing core body temperature and over activating your central nervous
system.
But I don’t think we’ve done it through chronotype. I predict there probably is a difference because I will say I’m, I can do that, I, now I can’t like go home and go straight to bed, but if I have a good hour and a half to, if I have two hours, I can go straight to [00:26:00] sleep.
But I know people who say it’s just what you said, I need five to six hours after I do that to like wind down.
Dr Mike T Nelson: Yeah, and I’ve seen some data on Aura and other, wearables, which you can discuss the validity of it, but even just like heart rate profiles, which are pretty accurate from Aura.
I’ve seen some athletes where they had two hours, man, they were good. Like their heart rate drops down. Everything is good. Where, someone like myself, you can just see where my heart rate just stays elevated for a longer period of time before it drops off.
Dr Allison Brager: Yeah. I do think really those companies so their validity to a clinical sleep study is not that bad.
Aura actually has really good validity. We’ve got within the government, we’ve done head to head comparisons across all the devices. And I know some companies will refute this, but or it performs as best to. The gold standard to sleep study across the board. But regardless of what type of device you’re [00:27:00] doing, like looking at this observational data and large scale populations, like it’s really these where I don’t know, I know my field does not like to hear this, right?
But it’s true. I, the wearable companies are leading the way in sleep research because they’re finally either confirming or validating. Small scale dust studies that were done in the lab are finally providing answers to questions that people have had for decades, but have never taken to investigate because, right, people, time, money, resources.
Dr Mike T Nelson: What would be some of those good questions that wearables are giving us some cool data on?
Dr Allison Brager: Yeah.
Dr Mike T Nelson: Do you have any other questions you think that would were, like, what would be some cool stuff we’ve learned from wearables recently that you think is worth highlighting?
Dr Allison Brager: So, this, now we can get into the biochemistry of sleep.[00:28:00]
I wonder differences in sleep quality between people who primarily do endurance training versus so say a mix of anaerobic and aerobic versus purely anaerobic versus aerobic training. I can guarantee that sleep quality is different and then also too if you were say An anaerobic athlete, your whole life.
So your weightlifter, your whole life versus your long distance runner, your whole life, I’m sure the sleep architecture of those individuals looks very different. Because of right. Their body trying to keep up with the demands of the sport. Like I predict that a lot of strength athletes. require more slow wave sleep, right?
Because what’s replaced with slow wave [00:29:00] sleep, the creatine the ATP reserves, and of course, right, the bolus of testosterone growth hormone, anabolic hormone factor release. Not to say that’s as like not important for aerobic athletes, but the amount and volume of energy resources that you are exhausting with anaerobic training.
From a glycolytic creatine perspective is far greater than with aerobic training. And all those things are primed and prioritized during like slow wave sleep. So that’s like a hypothesis I have. No one has yet to test it, but that is something I’d be curious about.
Dr Mike T Nelson: That, I don’t work with a ton of endurance athletes, but the handful I have worked at compared to strength and power athletes, and again, there’s a lot of genetic components to it, but just about every strength and power athlete I can think of.
As we ramp up [00:30:00] their training, like if they’re left to their own devices, if they can sleep more, they almost always sleep more. Like I would say most of them are eight to 10, 11 hours, sometimes in bed. We’re endurance athletes. Again, my sample size and endurance athletes is really small. I don’t see that big of an up regulation when their miles go up,
Dr Allison Brager: yeah. It’s funny you say that because I was just listening to Bert Soren on Joe Rogan’s podcast. Yeah.
I love Bert. Talking about
yeah, being a I forgot he, he threw with one of my teammates who wrote the four for my book Adrian Blewett and,
oh, cool.
Yeah Bert was saying as a thrower, if you weren’t in the ring, you were lying down and taking a nap, trying to stay in a supine position as much as you could.
Dr Mike T Nelson: Yeah. And you, and it’s so weird because you would look at sometimes they’re training, especially like all out, speed and performance, like those types of athletes they almost appear lazy, but their [00:31:00] outputs. are so high, but it’s just the duration is so short that I think looking at it, it just looks like they’re not doing much, but I think we underestimate the output that they’re doing within that period of time.
Dr Allison Brager: Oh, for sure. Like I, so, I still pull ball and I. I’ll take eight to 10 jumps in a pole vault session. And I truly, I can’t do a seven step approach, which is like 14 steps in total, because you only count like your left foot. That’s why you say seven steps. Cause I just get so exhausted, my older years, like 10 jumps in a pole vault session from a four step approach, so eight steps in total.
Is exhausting. Like I get, I used to get so exhausted from whole vault practice or gymnastics. Right. When we’d have a full on floor routine day, or instead of drilling, we would do a full on, beam bars, vault floor routine like that 90 seconds of [00:32:00] energy output is insane, whereas. I can run a half a marathon with limited training and after the half a marathon, peel okay.
Right. And go about my business. I don’t get that same level of fatigue and exhaustion I get from, 10 attempts to clear a bar or, 10 attempts to perfect a vault.
Dr Mike T Nelson: Yeah. And I’ve noticed too, that. Even just if you use like a simple RPE scale, there’s almost a universe of difference between a true RPE of a nine and a half and a 10.
It just feels like you’re on that part of the curve where it’s starting to do this. Cause I know if I’m doing a really hard row and it’s a shorter distance, like a nine sucks is not fun, but I’ll be functional. I could probably get through a training session after not the best training session, but I could do some light bodybuilding stuff or whatever, like a nine and a half.
No, I’m not doing shit the rest of the day. Like a true 10 out of 10 tests. Like [00:33:00] I’m probably not doing shit for two days.
Dr Allison Brager: It’s funny you say that because. That’s actually what happened to me the very first event of the International Functional Fitness World Championships. So the first event was the endurance event.
It was 4K biker into a 2K row.
Dr Mike T Nelson: Ew,
Dr Allison Brager: that’s horrible. So normally I would go like 90 percent right, but they had the urns wired where you could see who was in front of you by and who is behind. Okay, so my, I, first off, I threw up after three minutes after I finished this, like walking off the floor. I was like, Oh shit, I’m going to throw up.
I, it took me until the second workout on the last day. So basically like two and a half days of the three day competition to get back to normal. Like I went in the [00:34:00] sauna. I use that sodium bicarbonate lotion. I was like lathering in that. What do you call that? Not laxatives. Tums, because my stomach was like that acidosis, the lactic acid I produced.
Dude, it was not fun. At the end of the day, like I can’t be mad at myself because I gave it my all like that. I did a true RPA of the 10 on that workout.
Dr Mike T Nelson: Yeah, that’s reminds me of a story. Like Even in the lab, when I was doing stuff, like we would not test athletes next to each other. I made that mistake once and I, we didn’t have a person behind the treadmill to catch them if they got flung off, because it wasn’t supposed to be a true max, it was supposed to be like an RP of a nine.
It was hard, but it wasn’t like an all true max. And then we started the other athlete on the treadmill next to them. And so you see these two people like looking at each other to see how far they went and it was, I thought, Oh God, I’m going to get. Kicked out of here. I’m going to get [00:35:00] fired.
Dr Allison Brager: Yeah. There’s, that’s how, the, you want to know if, even if someone like trains now consistently, but say hasn’t competed in years, like you throw that competitive stimulus in that’s how, if that person’s true athlete or not,
Dr Mike T Nelson: yeah, another buddy he’ll remain nameless, he was an intern for the Chicago bears many years ago.
And when you first got there, he was. He was in charge of Brian Erlacher
Dr Allison Brager: and
Dr Mike T Nelson: his boss basically told him, he’s okay, if he injures himself, you just leave. Cause you’re automatically fired. Don’t even come to my office. Like just drive home. It’s okay. Like the second day he’s there, they were doing some baseline testing and they got on the treadmill.
And so he had two athletes who was in charge of testing. He starts them both at the same time. And then he sees Erlacher’s looking at the other guy’s score and just starts talking shit to him the whole time. And he’s going, Oh my God, he’s going to kill himself. Like on day one, I’m going to be fired. And this is the end of my NFL career.[00:36:00]
Dr Allison Brager: Yeah, no, it’s Hey, when you got to go, you got to go, yeah.
Dr Mike T Nelson: Yeah. Related to biochemistry and the sleep. What are your thoughts about, it seems and I’ve talked to Andy Galpin about this too, that. Equating sleep stages feels like kind of an old antiquated thing, because correct me if I’m wrong, there isn’t a hundred percent agreement on sleep stages.
It’s almost like high end EKG. I worked a lot of electrophysiologists in the past.
Dr Allison Brager: Yeah.
Dr Mike T Nelson: There is definitely standards, like most people agree if you see this, it means this, but it’s not. I was black and white. I think is what people on the outside think that it is. Like they think that it’s 100 percent cutoff.
Here’s your cutoff. This is exactly what it is. I’ve seen two EPs that were the top electrophysiologists in the U S argue about a strip for 45 minutes. And they’re both looking at the same thing on. a [00:37:00] discipline that’s pretty well established and they couldn’t agree with each other.
Dr Allison Brager: Yeah. I’m so happy you say that you said that because I 1000 percent agree with that.
And I, I take sleep staging as like very surface level assessments, like any sort of mechanistic sleep study whether it’s done in humans or an animal models, you want to look at the spectral analysis, right? So. The right sleep architecture is a byproduct of wave frequencies that I think is going to give you the true analysis because to your point, like when I first started working in a sleep physiology lab as an undergrad, there were four stages of non REM sleep.
Right. And stage three was. If there’s 20 percent appearance of the slow waves not more than 50%, then it’s stage [00:38:00] three. And then if there’s more than 50%, then it’s stage four. It was, I remember like when I was first learning to score, cause obviously there’s a learning curve there. I would have to make like a grid, so I made like a.
And I would put it over the computer screen. And then when I’d have epochs in question, I would start counting because that was the only way I could differentiate between stages three and four. And then eventually it got better at it, but I never got great at it. And it was the same thing. With mouse studies, I did just going through all those epochs.
And actually we do know might be different now with AI tools, but back then registered polysomnographer. is far better and way more accurate at sleep staging than an automated sleep staging machine might be different now,
[00:39:00] but
Bottom line being is yes, I think you hold sleep staging with a grain of salt and you look at The spectral features, that’s really, and it’s like that in other areas of science too.
I’m sure it’s the same with EKG with EMG. It’s like the real meat of the problem is in the spectral analysis.
Dr Mike T Nelson: Yeah. Same thing with heart rate variability. Are you doing time domain, frequency domain? What did you transfer it to? What method are you doing it? How did you collect it? How did you get rid of noise?
What do you consider noise? What are you not like? There’s a lot of stuff that goes. Into it and there’s different agreements on it, but even with HRV, like one of the main ones is still from fricking 1996. It’s like the last task force paper. It’s really? I think we could probably update this at some point.
But yeah,
Dr Allison Brager: well, we’re sleep staging how far back that goes.
Dr Mike T Nelson: It’s probably before that. I think I could be wrong in
Dr Allison Brager: 1930. So [00:40:00] the R and K manual by Alan Rex Shafton and So, Kales, they’re from University of Chicago, started that work in 30s, 40s. I think the actual manual came about in 1950 something, but it’s the R& K manual that to date, that is what the American Academy of Sleep Medicine and pretty much all sleep medicine academies around the world are using to certify someone in polysomnography.
So
with
the only update being in the early two thousands where they got rid of stage four and now it’s just stage three. So if greater than 20 percent of your epoch has these slow waves then.
Dr Mike T Nelson: Yeah, it just makes me think of how many discussions I’ve had with clients and non clients about their aura scores. And I do aura for what it is, but they’re like, Whoa, man, this one night, my deep sleep was 37 minutes. And the next night, man, it’s only [00:41:00] 45 and then it dropped to 21 and I’m going, Oh, like how much time do I have to try to.
Explained to this poor person about sleep staging, which I’m not an expert in and the fact that aura is trying to aggregate based on these accumulated studies of a surrogate marker, because it’s not even looking at EEG, it’s looking at heart rate data to interpolate what was actually going on and some other metrics and HRV and temp and stuff like that.
So it’s already one At least one or two things removed from even a direct measurement much less the staging and everything else goes into it
Dr Allison Brager: right I’m, so happy you have that sentiment because I do too and you know a lot of Like I see a lot of goodness in wearables and for oh sure
Dr Mike T Nelson: Yeah,
Dr Allison Brager: but like at the end of today I am a purist like to me the gold standard is eeg and it always will be you know It’s just like those Like I tried people to see the irrational [00:42:00] thinking behind the smart mattresses, where the smart mattresses, they monitor your sleep staging.
Yep.
And then adjust the temperature of the mattress based on that. I’m like, okay, so this mattress. Is able to detect from whatever sensor is touching anywhere, any body part and then sleep stage. Something that’s of the brain, by the brain and for the brain, based on that. And it doesn’t even have to be the same reference point.
And you’re going to tell me that it’s accurate. Oh that’s a good point.
Dr Mike T Nelson: Yeah I had an idea for this and I don’t know if some of the algorithms that the companies are doing it is. Correct me if I’m wrong, I think. Once you’re actually in a deeper state of sleep, you can drop external temperature pretty low, I think.
Correct. And if that is true, could you design an algorithm that, because not necessarily using [00:43:00] sleep staging, but using heart rate and movement to see as heart rate is going down, basically just keep dropping the temp, drop the temp and look at how much they would move in elevations and heart rate.
And once you estimate that they’re in a deep sleep, drop it further until they actually start moving and heart rate escalates, and then could you get someone into not a hibernation state, but like a deeper level of sleep by dynamically controlling it, where. Once they’re in that sort of stage, like dropping their town, but not so far that they get cold and then they like wake up.
Dr Allison Brager: Yeah. You know what that you, so there is a really awesome, great sleep physiologist, Craig Keller. He has done a little bit of this work in the sleep community. Like he’s, or he’s trying to now, like he’s basically I don’t know what the correct term would be like a thermo, thermologist.
So someone who studied like
Dr Mike T Nelson: the thermoregulatory
Dr Allison Brager: systems. Yeah. Yeah. For his whole [00:44:00] career. And then he of course got into the sleep field because of the close connection between REM sleep and core body temperature. But this is something he’s actually been trying to do. And he’s been working with professional soccer teams.
This is his. Pet project in retirement from Stanford. Oh, cool. And he still teaches at Stanford. And he like, Craig will never retire. He’s
just a podium
man. But yeah, no, I think that something like that makes. Perfect sense. If you want to, if you want to create the real Austin powers of preserving somebody in the hibernatory state and then bringing them out of it, I think that’s how you would go about doing it.
Dr Mike T Nelson: Yeah. Cause I’ve been
Dr Allison Brager: probably how animals do it. I don’t know enough about the thermal regulation of hibernation and animals, but I imagine it’s very similar.
Dr Mike T Nelson: It seems to be similar. And I don’t know why, like I’ve always read research about hibernating bears and the fact that Is if you’re a bear, you just basically get really fat before fall, you go to your little den, you go to sleep, [00:45:00] you don’t really get up, you don’t get out, you don’t really drink water, you don’t eat anything else, you don’t really use the bathroom that much, and when you wake up in spring, one, you bypass the horrible winter, it’s the older I get in living in Minnesota, that just sounds like a better idea every year.
And you have almost no muscle loss. The bears are not in there doing frickin push ups and, whatever, and like the Oh, I’m in hibernation, I gotta exercise today. They don’t exercise at all. And so I’ve always been curious about Could you recreate some states like that with I don’t know, artificial intelligence or manipulating your environment for humans to compress their sleep cycles because yes, everybody needs to sleep more, but that seems like the last thing anybody wants to do.
So if you could compress the sleep cycle. Somehow, I don’t know. It was weird thoughts in my head. No,
Dr Allison Brager: I love it. , honestly. Hey, that’s a good idea. Pitch to Elon [00:46:00] Musk and start a little startup. Yeah.
And
make millions off of it. I think that would be the golden ticket to, ’cause they do like you, I think there are ways to pack the sleep system and to either get into the deeper stages of sleep more quickly or to like.
Replace the homeostatic need for sleep. Like creatine is actually one of those things.
Yes. Yeah. And we have evidence for
that, right? It’s do a creatine supplementation protocol. You are actually more physiologically resilient to acute sleep deprivation. And it’s because right. Creatine is is reproduced during slow wave sleep.
So if you already have that. creatine being fed into the cell, then hypothetically you don’t need as much creatine replenishment through the act of slow waste sleep to have that creatine reserved for the next day. Yeah, I totally agree with you. I think about those things all the [00:47:00] time.
Dr Mike T Nelson: Yeah.
Anything related to the biochemistry of sleep that you find is fascinating that people may not know?
Dr Allison Brager: So actually, I think one of the things that is still controversial because unfortunately the one scientifically sound study for this, it was like a one off study because there’s pretty much one lab in the world that could quantify ATP with high fidelity, because believe it or not quantifying adenosine like extracellular adenosine and measuring it accurately is really freaking hard to do.
There are like two research groups, at least in the sleep field that are able to do that. And it’s through years of manipulating the high performance liquid chromatograph in a way that it can detect adenosine. And the one study that found an increased surge [00:48:00] in ATP with entry into slow wave sleep confirmed not through sleep staging, but sleep staging and spectral analysis had to retract their paper because their calculations were off.
Oh.
So, they were off by A thousand fold or something. Oh wow. So it wasn’t like a small
Dr Mike T Nelson: number. It wasn’t a little
Dr Allison Brager: one. They forgot about two decimals, right? I think that’s like an area where I want to know more about. Like I know we have so many sensor suites now that are typically like hypothetically able to look at different small molecule metabolites.
and different biofactors from sweat, like those sweat patches that now exist, like if we could come up with a high fidelity sensor that is able, obviously it’d be correlative look at metabolic byproducts and sleep staging or, sleep state or sleep architecture by way of [00:49:00] spectral analysis, I would love to see that but unfortunately I feel like we know so little about basic biochemistry of sleep, either because people didn’t think it was important, or like now there’s so much focus and money on public health and solving the public health crisis that people don’t want to do these foundational studies that I think really will help you address the public health crisis, and you have the same perspective to
yeah,
in the public health crisis yeah, sure, there’s behavioral interventions involved with that. But it’s also you have to start with the basics, right? You have to start with the basic cell and then work backwards.
Dr Mike T Nelson: Yeah, and I think, unfortunately, academia isn’t Really set up to answer basic questions.
So I had a real basic question I did for part of one of my HRV studies was basically, Hey, you take the same RR intervals. Do you run them through two different algorithms? You both technically apply the same thing to them, but maybe you do slightly different things. [00:50:00] Do you get the same result? Seems pretty basic, right?
So just doing a gauge R and R. And I thought for sure someone had done it, look through all the literature for weeks and weeks, couldn’t find it. Great. Okay, cool. We have the data from the study. This will be, easy to publish. Long story short, after 14 iterations of that paper, I gave up and said, screw it.
I quit. Basically, nobody wanted to publish it because it looks bad that, oops, we missed this.
Dr Allison Brager: Yeah.
Dr Mike T Nelson: And it’s not new. It’s not sexy. It’s boring and basic, but it just feels like in academia, it’s always. The next new crazy thing, because that’s how you get a promotion and that’s what gets published and that’s what gets driven, there isn’t a drive to go back to some of the old school, basic analysis that we need to build all of this other cool stuff on top of, but.
I,
Dr Allison Brager: I’m right there with you and not to poo on academia, but I’m going to do it. Cause I am a recovering academic is
Dr Mike T Nelson: yeah, [00:51:00] me too.
Dr Allison Brager: That’s that’s my problem with academia. And I get so frustrated at these conferences because like we don’t in the government, we don’t always share the methods behind the madness, but I can tell you the reason I love doing.
Science for the government is we take that approach is like, even if it’s a foundationally known concept. That’s our transition process with R& D is we go from basic science in the lab, and then we apply that science to the field, and then we start adding this technology into the play, but then we test this new technology in a basic setting, then an applied setting, and then do reiterative Development before it’s available.
And that’s, you have to always go back to the basics and the foundation. It’s just like you do in athletics, right? At the end of the day, like your warmup routine, your technique for highly skilled activities. It’s all about perfecting and returning [00:52:00] to basic movement and drilling and technique. So yeah, I totally agree.
And I. I probably am the nicest academic reviewer because of that, because I know I review for two different sleep journals, or I’m an associate editor for sleep health and sleep advances. And people, friends, colleagues, whatever would be like, Allison, why would you accept or give them the benefit of the doubt with that paper.
That’s such a basic concept. There’s nothing intuitive about this. I’m like, no, but okay. It might not be something that’s like revolutionary, but like it basically found exactly what you said, the gap in knowledge and basic fundamental understanding that was missing.
Dr Mike T Nelson: Yeah, I’m the same way when I do peer reviews and probably because also I got farmed out to a different department for a year and a half of my PhD to get my third [00:53:00] study done.
We did all the work, blah, blah, blah, blah, blah. And we found the result and the result basically said no effect. I’m like, okay, whatever. Cool. Like I’ll write it up. I had most of the study already written and everything. The lead author of the PI is well, we’re not publishing it. What do you mean?
We’re not publishing that. I need this as my third study for my PhD to graduate. He’s well, we didn’t find an effect. And I’m like, whatever we found is what we found. I don’t know what you want me to do about that. And so we had this long argument and long story short, it never got published. And I had to go find a third step for another two years.
Dr Allison Brager: Wow. Yeah. It’s funny you say that. Cause one of my, one of the women I worked for as a graduate, or when I was an undergrad, I worked for her. She’s a graduate student at Brown. She has her own lab now at Rush University. It’s she spent her whole dissertation and pretty much most of her career finding a null effect with Trying to manipulate the delayed phase [00:54:00] of a teenager.
So again, like we talked about, when you’re going through puberty, your circadian clock naturally delays itself. And so it’s a delayed phase. She tried anything and everything to stop that delay from happening, timed light exposure to a combination of light, caffeine, melatonin, all the above. It would not, the robustness of the rhythm would not shift.
And
a lot of her early work is not published because, nobody wants to publish it. But I don’t know. I always see no effects as as more profound than like significant effects. Because I think not having an effect just, right, it shows you just how complex the system is. And how robust it is and unwilling to change.
Dr Mike T Nelson: Yeah. And usually it also shows you that what you thought was going to happen was wrong. It’s if anything, we should have that stuff published because if we could, that was the things we couldn’t predict. Like our prediction wasn’t correct. I’m talking to, not talking to statistical sense, but just, [00:55:00] Hey, here’s what I think is going to happen with this study.
Oops, it wasn’t right. And you’ve spent 15 years of your life studying this thing and your prediction was wrong. That would be cool to know.
Dr Allison Brager: I know. I think they do have a journal for negative findings now.
Dr Mike T Nelson: Yeah I always ask. I’m almost
Dr Allison Brager: confident they do, right?
Dr Mike T Nelson: I think they do, and I always ask my academic friends about that, and they all come back with the same answer.
They’re like, being the top publishing author in that is basically academic suicide. It’s
Dr Allison Brager: Oh, crap. Yeah, I know. But again, that’s why I’ll never go back. I’ve always, I still like adjunct teach and all that, right? Yeah. I’m excited to go to the West, to West Point and be in the classroom, but like I do not miss academic research at all.
And I will not go back.
Dr Mike T Nelson: No, my, my big turning point was when I realized, Oh, you mean, if I have my own funding source and I don’t need to make money doing research and I have the skills to [00:56:00] help people, I could work on almost any project I want because. Most people would not turn down someone offering free help who’s qualified.
Oh, so I could still do some of this stuff and just pick and choose what I want and skip all the committees and the R1 writing the grants and all the other crap I have no desire to do. I will never make any money off it, which is fine. I don’t care. I’m like, okay, that sounds a lot better.
Dr Allison Brager: Yeah, exactly.
Yep, exactly.
Dr Mike T Nelson: Where can people find out more about you? I know you got a lot of great stuff on Instagram and other places.
Dr Allison Brager: Yeah. So I’m mostly just Instagram. Since I worked for the government, I just. Pretty much keep it to that one channel. I’m not really on LinkedIn or anything. So doc jock ZZZ, I normally, post things on there. I do have my popular science book meathead unraveling the athletic brain.
I wrote that like over 10 years ago now, which is crazy when I was a postdoc when the field was just starting about understanding the neuroscience of athleticism. Like we finally started doing multiscale EEG [00:57:00] studies, MRIs. And more mechanistic studies on the brain of athletes, but just the basic foundational knowledge in terms of neuroscience of performance it’s in that book.
So you can buy it.
Dr Mike T Nelson: And where can people find the book?
Dr Allison Brager: So you can just Amazon so type in my. First last name meathead unraveling the athletic brain. I wish I had a copy here, but I don’t
Dr Mike T Nelson: That’s right. I will definitely put a link to it. Thank you so much really appreciate all the
Dr Allison Brager: Your new book too.
Dr Mike T Nelson: Oh, yeah. Thank you. It’s nice to finally get it out like
Dr Allison Brager: I
Dr Mike T Nelson: don’t recommend writing books a lot, as it is a very long,
Dr Allison Brager: arduous,
Dr Mike T Nelson: a lot of work process.
Dr Allison Brager: It’s more fun than writing reviews. I’ve been like, procrastinating like hell on a review and a textbook chapter. Also, because I don’t get paid for that,
Dr Mike T Nelson: academic textbook chapters, I gave that up, because it’s a lot of work for
Dr Allison Brager: Nothing,
Dr Mike T Nelson: not much of anything at all.
Cool. Awesome. Thank [00:58:00] you so much. Appreciate it.
Dr Allison Brager: Yeah, of course. Absolutely.
Speaker 2: Thank you so much for listening to the podcast. Really, really appreciate it. Huge thanks to Dr. Allison Brager for all of her wonderful information there. Make sure to check out all the great stuff she’s got on social media and all of her wonderful stuff that she is doing. If you wanted to hear her top four sleep supplement recommendations, go to the link below at the Flex4 and it’ll be sent to you automatically.
It’ll also enroll you into the Daily Fitness Insider Newsletter from me, and you’ll have a lot more information there. If you’re already on the newsletter, you will get that automatically. If you’re interested in ketones for cognition and performance, check out my friends over at Tekton. Full disclosure, I am a scientific advisor and ambassador to them.
[00:59:00] Also check out our friends at Element. I’ll have a link for that down below. Also, so thank you so much for listening to the podcast. If you could give us the old like and downloads and whatever else to help us with the old algorithms, that always helps a ton to help us with better distribution. Thank you again.
And we’ll have much more coming to you next week. See ya.
Speaker 3: There’s something wrong with this hearing aid. Yeah, what’s wrong? I can’t hear with it. Oh, no wonder. It’s too far away.
Speaker 4: This podcast is for informational purposes only. The podcast is not intended as a substitute for professional medical advice, diagnosis, or treatment. You should not use the information on the podcast for diagnosing or treating a health problem or disease or prescribing any medication or other treatment.
Always seek the advice of your physician or other qualified health provider before taking any medication. Or nutritional, [01:00:00] supplement, and with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have heard on this or any other podcast.
Reliance on the podcast is solely at your own risk. Information provided on the podcast does not create a doctor patient relationship between you and any of the health professionals affiliated with our podcast. Information and statements regarding dietary supplements are not intended to diagnose, treat, cure, or prevent any disease.
Opinions of guests are their own, and this podcast does not endorse or accept responsibility for statements made by guests. This podcast does not make any representations or warranties about guest qualifications or credibility. Individuals on this podcast may have a direct or indirect financial interest in products or services referred to therein.
If you think you have a medical problem, consult a licensed physician.






Leave A Comment