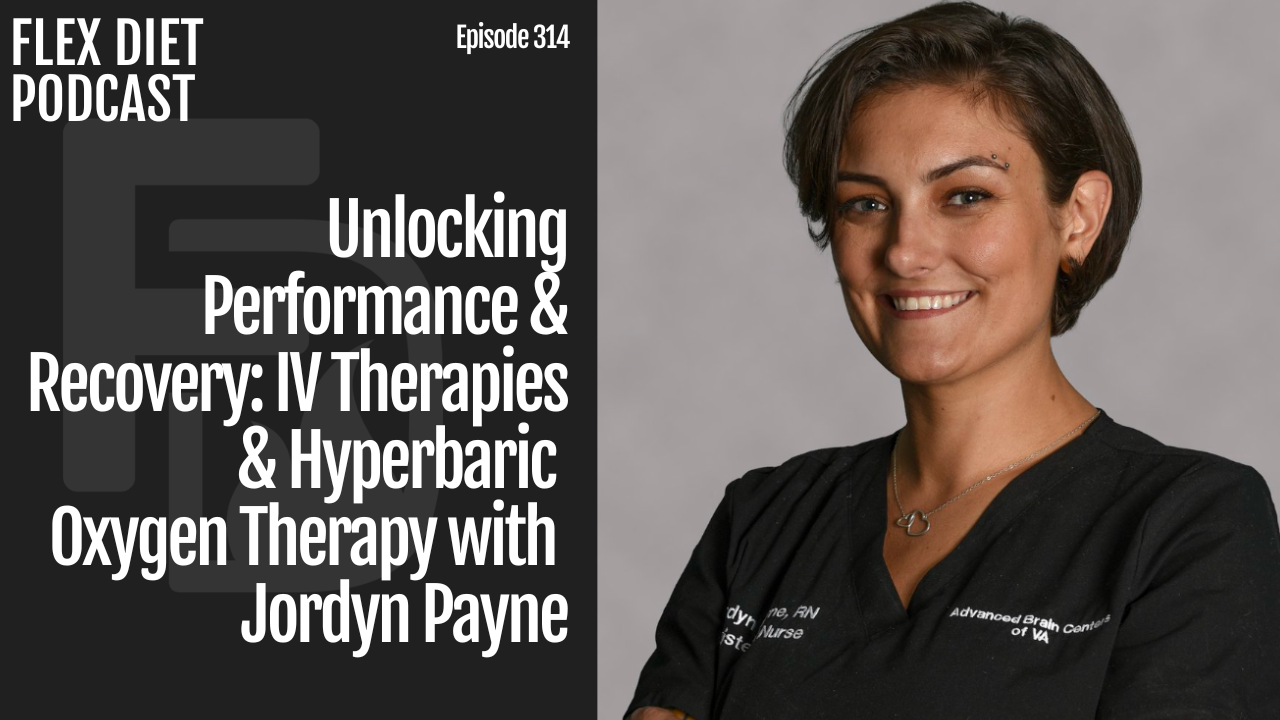
Join me, Dr Mike T Nelson, on this week’s Flex Diet Podcast as I sit down with Jordyn Payne from Advanced Brain Centers of Virginia to dig into the real benefits and applications of IV therapies and Hyperbaric Oxygen Therapy (HBOT). We get into the details of Myers Cocktails, NAD infusions, and other IV treatments—how they can boost brain function, improve performance, and speed up recovery.
Jordyn also shares insights on HBOT’s role in treating traumatic brain injuries and concussions, plus how it can be a game-changer for overall brain health. We also discuss the importance of preventative medicine and how to vet IV therapy providers so you don’t waste time (or money) on subpar treatments.
- Tecton Life Ketone drink! https://tectonlife.com. Use code DRMIKE to save 20%
- LMNT electrolyte drink mix: miketnelsonlmnt.com
- Physiologic Flexibility Certification Course open through March 24, 2025. Enroll here.
Available now:
- Grab a copy of the Triphasic Training II book I co-wrote with Cal Deitz here.
Episode Chapters:
-
01:29 IV Therapies and Their Benefits
- 01:57 Physiologic Flexibility Certification
- 05:00 Discussion on Patient Populations
- 07:36 Rise of Preventative Medicine
- 14:09 NAD Infusions: Benefits and Experiences
- 25:07 Combining Therapies for Optimal Results
- 30:05 Exploring Myers Cocktail
- 31:40 Understanding the Myers Cocktail
- 33:33 Choosing the Right IV Therapy Provider
- 38:26 Hyperbaric Oxygen Therapy for Wellness and Performance
- 40:43 Hyperbaric Therapy for Athletes and Brain Injuries
- 48:06 Comparing Soft Shell and Hard Shell Hyperbaric Chambers
- 53:48 Safety and Efficacy of At-Home Hyperbaric Units
- 57:43 Conclusion and Contact Information
Flex Diet Podcast Episodes You May Enjoy:
-
Episode 309: Understanding Adaptogens: Boost Performance & Well-being with Dr. Jeremy Townsend
- Episode 215: Breathing, Heart Rate, and HRV: An Interview with Dr. Scotty Butcher, The Strength Jedi
Connect with Jordyn:
- Website: Advanced Brain Centers of VA
- Instagram: @abcofva
Get In Touch with Dr Mike:
Rock on!

Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
Welcome back to the podcast. I’m your host, Dr. Mike T. Nelson. On this podcast, we talk about all things to increase performance, muscle, improve body composition, and to do all of it in a flexible framework. Without destroying your health today on the podcast. We’ve got Jordan Payne and we’re talking all about two topics today the use of IVs for everything from Myers cocktail to NAD and this could be for people looking for a cognitive or performance edge or even for different pathologies She is from the Advanced Brain Centers of Virginia And we also talk about what’s commonly called HBOT, or Hyperbaric Oxygen Therapy.
Wide range here again for people just looking for an edge for performance, maybe cognition, and then also [00:01:00] pathologies such as traumatic brain injury and concussion. So this I thought was a really cool chat with her. I got to meet her in Virginia when I was out there recently, I got my first Myers cocktail IV, which is a big deal for me cause I absolutely hate needles but it went well.
She did a great job and wanted to have her on the podcast to discuss what she has seen in terms of potential benefits and experience. What are some questions to ask if you are looking at these different types of therapies? What are some of the differences between them? And what’s really interesting in this area is there’s just not really a ton of research.
I know there’s a bunch more coming. So in that area, I always like to ask people who are clinicians who are doing this. on a day in and day out basis, what are some of the anecdotal things that they have seen? Also want to let you know that if you are [00:02:00] listening to this week, the Physiologic Flexibility Certification is still open right now until March 24th.
At midnight pacific standard time 2025, if you are looking for ways to increase your body’s ability to recover and become more anti fragile and just generally harder to kill, and you’ve got pretty good on the basics that exercise, nutrition, and sleep. This, in my biased opinion, is the next level.
Everything from temperature changes, sauna, cold water immersion, to pH changes. The pillar number three is advanced fuels. So we’re looking at ketones and lactate were some of the benefits of those. And then the last pillar is oxygen and CO2 regulation. Everything from different types of breathwork to different types of training.
And the great part about this is. We give you the overall big picture and [00:03:00] framework, and then we have a ton of really detailed stuff. I went and spent a lot of time looking at all the research on all these different areas. I started looking at this concept, man, over almost eight, maybe nine years ago now.
So I’ve been reading a fair amount of research on that since then. I think when I tallied up all the studies I read, for this cert. It was over 400. There’s a lot, not that many in there because some of them just didn’t really apply. So they weren’t really used. But we make it useful. So even if you don’t have an advanced degree, you can still understand what the heck is going on.
And then we boil it all down to five explicit action items yourself or your clients can use right away. So if you’re that check out the newsletter. We’ll put a link down below to that. That’s going to be the best place to get all of the information, the link for the page and everything to get more.
You can also just hit reply once you’re [00:04:00] on the free insider newsletter if you have any questions about the cert. It is open right now if you’re listening to this once this podcast is out. Until March 24th at midnight Pacific Standard Time 2025. And it will not open again until fall of this year. So if you’re thinking about it check it out right now is your chance.
Big thanks to Jordan for all the wonderful information and enjoy this podcast chat with her all about IV therapies and hyperbaric oxygen treatment.
Dr Mike T Nelson: Hi, how are you today, Jordan? Welcome to the podcast.
Jordyn Payne: Hi, thank you, I’m well, thank you for having me.
Dr Mike T Nelson: Yeah, how is everything for you and you guys in your clinic? Correct me if I’m wrong, is near Virginia, is that correct?
Jordyn Payne: Yes, in Virginia, in Reston, Virginia. On the Reston Hospital campus, although we are not in the hospital, we are very close to it, right next to it, on the same campus.
Dr Mike T Nelson: Awesome. [00:05:00] And in terms of patient population, like for we’ll talk initially about IV therapies and then we’ll talk about some hyperbaric therapies who do you generally see? Because I think that’s a huge topic that gets left out, especially online when everything is like a 30 second clip.
And as you can see huge differences in maybe people who have certain pathologies compared to people who are healthy and I think at least from what I see is There’s a lot of no discussion about the context of, what the person was doing. What is their background? What are they trying to achieve?
Are you looking at a, someone who has metabolic issues, concussion issues, or is it like an already like functioning high level athlete who’s trying to get to that next single digit percentage? So I’d be curious as to, I know you guys see a wide variety of people, but who do you typically, see come into your clinic?
Jordyn Payne: Yeah, so I think that you you’re right in saying that we do see a wide variety [00:06:00] of folks, and when it comes to IV therapy in particular it depends on what they’re coming for. That’s how we’re going to determine what their tailored needs are and which infusion therapies, nutraceuticals are going to be most beneficial for that individual.
But yes, we see. Athletes, we see folks who just want the anti aging benefits, the general wellness benefits as well as folks with traumatic brain injuries. That’s our bread and butter, actually traumatic brain injuries, post concussion syndrome, neurodegenerative disease processes, neuroinflammatory processes.
But I would say that we have seen an uptick in particular with the general. Enhanced performance benefits. We’ve seen a lot more people come in for that. Whether that is just for an athlete or somebody who is in hit that 40 years of age mark and wants to just improve their overall wellbeing and longevity and anti aging benefits that we can [00:07:00] see with our, with that intraceuticals.
Dr Mike T Nelson: And do you think the uptick in? People just looking to improve. Have you seen that’s gone up more in the last one or two years? I feel like the industry is becoming very divided now where you’ve got ultra high end facilities and high end things, and I know certain gyms have an IV infusion day, or they have someone like yourself come in and provide it as a service in addition to, red light and cold therapy and everything else.
Have you seen it? Seems like it’s a more of a, we’re on that higher spike in that area.
Jordyn Payne: Yeah, I think that especially the newer generations are really becoming more educated in alternative and complimentary medicine and realizing that in preventative medicine is what I really should say, because they’re realizing, oh, there are things that I can do for myself before I become.
Ill and there are things I can do for myself to be a better version of [00:08:00] myself and to prevent these long term issues that I may or may not run into, especially with the increased education in diet and benefits of exercise. I think that it’s just natural that people are going to fall into.
Nutraceuticals and supplementation and overall health and well being. So I think that there’s more information out there in the age of technology. I think people have more resources and that this information is more readily available and people are becoming. Tired of taking medications and then more medications to, to offset the side effects of those medications and things of that nature.
So I think they’re looking for those alternative options and in doing so, they’re coming across what we do. And whether that’s from a gym or a med spa or something a little bit more advanced, like the practice that we work in.
Dr Mike T Nelson: Yeah, it seems crazy to me that the Pharmaceutical model in general is, and I get it like if everything, if all you have is a hammer, everything is a [00:09:00] nail, right?
That I know is some of the GLP ones there. There’s, I don’t know how many different versions of those in the pipeline now, but there’s new
Jordyn Payne: ones all the time,
Dr Mike T Nelson: a couple of years. And then because of some of the original studies have shown muscle mass loss or actually lean body mass loss, which you could debate is how much of that is muscle, how much is not.
But I know several people in pharmaceutical industry are looking at, Okay, so what other kind of drugs can we now target to limit the muscle loss from the GLP 1s? Which to me, the whole mindset of, Oh, well there’s a side effect, so we’ll give you another drug for the side effect, which might have another side effect, so we’ll give you another drug for that.
Yeah, it seems a little crazy.
Jordyn Payne: Yeah. Yeah. I’ve dealt with that myself with being someone who has dealt with chronic illness in the past. Just realizing that, Hey maybe medications is not always the answer. Maybe it’s taking care of myself and my body and eating better foods and, doing things [00:10:00] to Get rid of the free radicals in our body, which is a lot of what our infusions work on in the mitochondrial health.
And, these environmental exposures that we’re exposed to on a regular basis on a daily basis. They do damage over time alongside. the diets that we currently American diet. So I think once we start really focusing on, Hey, how can I help myself? Before I turned to pharmaceutical options I think that we are definitely seeing an uptick in people realizing that’s an option.
Dr Mike T Nelson: Yeah. So if we stay with people who are generally healthy, looking more for, my little air quotes, longevity performance, things of that nature. What kind of services do you provide? What have you found is typically most useful for that population?
Jordyn Payne: Yeah, so, in general we, at our facility, we do hyperbaric oxygen therapy, IV therapies, and then also neuromodulation and neurofeedback.
Generally when we’re looking at a patient or an, customer who who [00:11:00] is looking for general wellness benefits or athletic performance. All of those modalities can be beneficial. It just really depends upon the individual. It depends on what their lifestyle looks like. It depends on what their diet looks like because we are going to ultimately be combating inflammation.
So if we are helping improve the general wellness of one individual who maybe is Consuming other substances or is not doesn’t have the best diet. Their treatment protocol may look different from an elite athlete who is only putting the best of the best in their body. They may need, less hyperbaric or less infusion therapies, depending upon how they respond.
And that’s one of the things that we really try to do is look at the individual and tailor it to their needs. But generally every single option treatment option that we provide is typically beneficial in somebody who’s looking to promote that general health and performance. I would [00:12:00] say though, that my favorite is actually phosphatidylcholine IV.
Really? I’ve never
Dr Mike T Nelson: had that. I believe the only IV therapy I’ve had is. I had one from you when I was out with my buddy cab and it’s not that I’m against it. It’s usually a cost. And like I told you there you did a very good job. Cause I hate needles. So for me to do that was like a big deal.
Jordyn Payne: Yeah. Well, I’m glad that that went so well, but yeah, that was a Myers cocktail, which is generally beneficial for most people. Of course we always do a comprehensive Consultation with each individual before we do any type of an infusion to make sure that we’re not looking at any type of kidney or liver dysfunction that might interfere with infusion therapy because we are putting fluids into the body.
And so, regardless of the fact that anything that we’re administering is naturally found in the body, we do want to be, conscientious of potential risks that are there. Anytime you put an IV into someone, there’s a risk, but [00:13:00] particularly with somebody who may be at high risk of kidney dysfunction in particular.
But phosphatidylcholine is a phospholipid that is is a good source of choline, which is found in acetylcholine, which is a neurotransmitter that we see really help improve brain fog any cognitive function whether that’s somebody who has a history of a concussion or CTE or traumatic brain injury, or is somebody who just generally from the daily, stress and environmental exposures and such might notice that they have a little bit of cognitive lag or brain fog. I just find the phosphatidylcholine works really well and helping with that. And then also at the mitochondrial level of cellular repair. So we can see that folks are able to recover from injury faster if they’ve had long workouts, things of that nature.
Phosphatidylcholine is going to help them recover faster. And all of our infusion therapies do that. Most people are Like to talk about NAD as the heavy [00:14:00] hitter. And that is a great treatment option. I just like phosphatidylcholine the best personally. And NAD is the one that we also provide.
Dr Mike T Nelson: Yeah. NAD I find is, it’s super interesting. Like when a lot of the research originally came out, like. I always look at what is the physiologic story, right? Does the story even make sense? Before we look at any of the data, before we look at anything else, and the story on NAD was like, oh, okay, that makes sense.
We know it declines, correct me if I’m wrong, declines with aging. We know that as a supplement, it does appear at least orally and also obviously by IV would get in. I would say from what I’ve looked at on the data on the oral supplements, which again, IV dose could be different, There’s some interesting stuff with pathologies, but for performance stuff, I haven’t really seen too much of an uptick in it.
I tried one version myself at like two grams a day for probably like two months. I didn’t really notice anything but in terms of [00:15:00] NAD IV infusion, I’ve had friends who have done it and, some of them reported like, Oh my God, it was like the best thing I ever did. Other people said, I don’t know.
I didn’t really notice any effect. There’s very little. Unfortunately on it. So what have you found in your experience since you guys are obviously treating a lot of people tell us a little bit about the experience. Cause I’ve heard it can be painful. And what have you seen?
Jordyn Payne: So I have seen, I would say that every patient I’ve ever had get NAD has reported an increase in energy or decrease in fatigue, depending upon what we’re treating.
And they are always looking forward to their NAD infusions after the fact, because you’re right during the infusion, some folks can experience Discomfort. I wouldn’t say so much pain. It’s more of we may see a little bit of nausea. Sometimes we see a little bit of sinus congestion. Sometimes we see a headache and temperature [00:16:00] changes.
I see that more in women than I do in men. And generally that can be mitigated by slowing down the infusion. Sometimes they can take up to four hours to infuse. Oh, I also, yeah. And I also tend to pre medicate with anti nausea medication Zofran or something like
Speaker 2: that. Yeah.
Jordyn Payne: Yeah. But I’ve also had some patients who they have zero side effects during, but again, once the infusion is done, we don’t see any side effects generally afterward.
Dr Mike T Nelson: Why is that? Because it’s not just the fluid rate. Obviously there’s something. I’ve heard this from, like, most people who have done it too, like, 70 percent of the people I’ve talked to are like yeah, it was not really, like you said, not really painful, but they felt a little icky, it just felt uncomfortable.
But it only seems to be with that, at least what I’ve heard, it only appears to be with the NAD, which I find just oddly fascinating.
Jordyn Payne: Right. Yeah. Honestly, I don’t I haven’t really looked into too much as I don’t have a good answer from
Dr Mike T Nelson: anyone. So yeah,
Jordyn Payne: I don’t [00:17:00] really know. There hasn’t been a lot of good answers to that.
And again, why does it affect one person more than the other? I will say one thing I have noticed with my neuroinflammatory patients. So my individuals who have Usually like an MTHFR gene mutation those types of patients, or my patients with chronic Lyme symptoms, or my patients who have, again, neuroinflammatory conditions.
When they are in a flare, they are significantly more sensitive to their NAD infusions. When they are not, they’re like, hey, slam it in, I’m good to go.
Speaker 5: So there
Jordyn Payne: is definitely something about inflammation. I think that is that increases the likelihood of that discomfort. But I have patients with neurodegenerative disease processes like Alzheimer’s who have not.
about these side effects. So, I’m not entirely sure, but I do know that historically, I have yet to see a patient who has any type of side effect [00:18:00] any more than an hour after the infusion. So that has been Usually patients feel so good the next day that they don’t mind the side effects during the infusion.
Yeah. But generally I have seen a lot of benefit from a fatigue and energy benefit, I’ve seen that be what’s most reported. And we know that NAD works on the metabolism in general. And so I think that’s where it can be beneficial. From a performance aspect is that it is going to boost your metabolism.
Now, if you are an individual who already has a pretty well regulated metabolism, maybe you won’t see as much benefit from NAD.
Dr Mike T Nelson: Yeah, and I believe the cost of NAD, just even getting the raw materials is quite expensive still, correct?
Jordyn Payne: I would say it’s more expensive than the other nutraceuticals at this time, yeah it’s not.
But we, I think that we have made, but it’s also not one of those ones that you do necessarily every day either.
Dr Mike T Nelson: Yeah, so it’s [00:19:00] not something you’re coming in for like daily infusions for months on end.
Jordyn Payne: Right, like so our other nutraceuticals that we do, we will do up to daily. But NAD typically will do, once a week.
Now, if somebody really requests twice in a week, that’s fine too. It’s not dangerous to do it more, but it is cumbersome. It is up to a four hour infusion oftentimes. And so generally speaking, patients aren’t super excited to do it more than once a week. I do think that it, I have not seen the same results from oral NAD.
I do have some individuals who take oral NAD because, maybe they are on a fluid restriction and we can’t do,
A liter of fluid, and they don’t seem to have the same results, but they do notice that over time their body starts to feel a little bit better. And it’s hard to say which supplement is always inducing that too, because we also usually have other nutraceuticals on board.
Dr Mike T Nelson: I feel like if there’s any researchers listening, this would be like a super cool study to do if you could get [00:20:00] IRB approval would be pick your indication, whatever it is, your outcome. Obviously, I’m an exercise physiologist, so I’m biased to does it enhance performance or cognitive output, whatever. It’s super easy set up if you only do like, say, one or two infusions, have a randomized controlled saline infusion, they don’t know what’s what I don’t know, but I haven’t seen any of those studies that are done either.
So I’ll be. Fascinating. And then the second part would be mechanism. Like you mentioned, like, why are some people more sensitive to it? You could look for associations for just different inflammation and things like that would be interesting to see what’s going on.
Jordyn Payne: Yeah. I’ve actually started working on some case studies, particularly, yeah, particularly in the presence of hyperbaric therapy for traumatic brain injuries, post concussional syndrome.
But I’d be happy to start doing some for these IV infusions as well. But of course I would love to do something with an IRB, I’ve done that in the past. I used to work in research.
So I, I love research. So anybody, if anybody’s listening [00:21:00] let’s link up.
Dr Mike T Nelson: Yeah. That’s what I was mentioning.
Next time. Like there might be someone who’s interested and wants to know a good project that. All these things are already being used. They’re over the counter. I don’t think approval would be too difficult. Like the setup is, rather easy to do. Just pick your outcome. It’s very easy to have placebo control.
So, some of the other studies are much more complicated and require a lot more equipment and fancy things like that, where this is, all studies are a pain in the butt using human subjects. I get it. It’s not easy, but. Relatively speaking, it’s a little bit on the easier side, and it just seems like we just have so little data on it, it’d be cool just to see what’s going on.
Jordyn Payne: I’m hopeful in that, what we were talking about earlier with this move toward more preventative type medicine. I’m hopeful that we will start seeing a push in research for these things as well. I’m hoping that we’ll see more interest. And that, as society is moving that direction and [00:22:00] hopefully our, government leadership will also be more interested and then we will see.
Dr Mike T Nelson: Yeah, totally. And I get it from an NIH standpoint, it’s probably not going to be an NIH funded study, but, maybe someone has some money they want to donate, you got a researcher who’s looking for a cool project, like, hey, something like that could happen. What have you seen with like concussion TBI, that type of thing with NAD?
Because I’ve heard from, A few of my friends who do a lot of work with basically concussion TBI, that they’ve had pretty good results with NID, NAD infusions in that particular pathology.
Jordyn Payne: Yeah, so I’m a specific patient comes to mind who he dealt with an injury during a basketball game and ultimately it was a pretty significant traumatic brain injury where he actually had to have a metal plate implant.
Oh,
Speaker 5: wow.
Jordyn Payne: Yeah, so he ended up being one of our protocol patients who was undergoing hyperbaric therapy neurofeedback neuromodulation and then he was doing all of the [00:23:00] nutraceuticals as well. And he. In particular was one of those patients who could tell the difference when he had any beer didn’t. And he very much felt that it improved his cognitive function and energy.
So, that’s the best. Case scenario, I would say where I can really tell a difference, if he went one week without it, or even he could tell when it was time for his
Speaker 5: NAD.
Jordyn Payne: So, he was doing it once a week. So let’s say he was doing it on Thursday by Tuesday or Wednesday, the following week, he’d be like, okay, I’m excited for my NAD.
That’s my gold. My liquid gold is what he would call it. That’s something that we also call IVIG, but he was calling it that. And He very much could tell the difference and he liked doing it just before the weekend because it gave him more energy for the
Speaker 5: weekend.
Jordyn Payne: So I think that’s a really great example of how I see it help with that improvement and over long term ultimately he was able to discontinue treatment with our [00:24:00] practice because he improved so substantially.
It wasn’t something that he had to continue. Indefinitely. So that’s always been best case scenario too, because patients, some individuals, they do end up maintaining doing some type of like a maintenance schedule with us long term just depending on how they are improving and what their triggers are.
One of the things I try to do with individuals is figure out. Okay. What in your daily life have you found that triggers more of your symptoms or a decline in your cognition or disrupts your sleep? Because sleep is a really big issue when we talk about traumatic brain injuries. And so when we can find those triggers, we can also then plan in the future when we’re doing these maintenance therapies.
Okay. When do we need to do it? Let’s plan for once a month or once every three months. With an understanding that if you have been exposed to this trigger or anticipate that this trigger is upcoming, you can plan to [00:25:00] come back in for a one day or five day boot camp, depending on their individual needs.
Dr Mike T Nelson: Yeah. And in advanced cases, and this may be just a purely logistics thing that’s hard to do, or it might not matter. Would you do like the NAD infusion, and then would you have them do like a neurofeedback right after it? Like the theory being, they’ll have more energy, they’ll feel better. Maybe the neurofeedback works better, but I’m not a expert on neurofeedbacks.
I know that’s more on the unconscious level too, so maybe it doesn’t matter as much. I don’t know.
Jordyn Payne: Well, so one of the things that we do try to be conscientious of is that we are doing a lot of different treatment therapies in one day, oftentimes. And so we do try to consolidate as much as we can. So often we actually are doing neurofeedback during an NAD.
Oh,
Dr Mike T Nelson: interesting. That makes sense. Yeah,
Jordyn Payne: yeah. And so patients have really found that to be beneficial and they really like it because As much as we want to be able to give them every treatment and every therapy, we also want to make [00:26:00] sure that we’re maintaining quality of life. And if you’re coming in and just spending so much time and energy at our facility and then have no time to enjoy life otherwise, that’s not helpful either.
So we try to get people in and out as fast as possible while maintaining the efficacy of treatment. And so far we found that doing an AD. While doing neurofeedback has worked quite well. From speaking to a neurofeedback standpoint, I think that would be a better question to address to our chief of neurofeedback, who’s been doing this forever.
She could probably speak even better to that, but we do have some Methods in place like for neuromodulation, we’re going to do certain neuromodulators pre neurofeedback and certain ones after we do hyperbaric therapy pre infusion therapy every time if they’re going to be doing hyperbaric, they’re going to have their hyperbaric therapy prior.
To infusion therapy, if for no other reason than the fact that once you’re in a hyperbaric chamber and you need to, if you need to urinate, it’s going to be,
Dr Mike T Nelson: [00:27:00] but
Jordyn Payne: there’s some other benefits to it as well. So
Dr Mike T Nelson: cool. Yeah. We’ll get into that in just a bit. Yeah. So I mentioned that also for, I work at the Kehrig Institute, so they do a lot of, functional neurology and me know in general with concussion, there’s a lot of stuff that goes on, but in my brain, like mechanistic wise, I’m thinking.
There’s definitely an energy issue. There might be maybe a plasticity issue. Neuroplasticity can be a pro and a con. So if we can give them something that’ll increase more energy, they could do more therapy. They could try to take that neuroplasticity and drive it in a better direction or possibly agents that could increase neuroplasticity.
Would you get a better result by having. An upregulation and maybe more of that critical period and providing them the energy so they can do more of the work similar to athletic training, right? If you have the right fuels, you have everything on board, you can do a higher level of quality work. We would [00:28:00] expect whatever direction you’re pointing that at, you would get better over time faster.
Jordyn Payne: I just don’t know that in with, in the case of NAD, I don’t know that we really see that increase in energy immediately after the NAD. So I would say I can think of one patient where I have seen that where he does actually seem to almost perk up during his NAD infusions, but that is not a traumatic brain injury patient.
That’s a neurodegenerative diseased patient with aphasia and dementia. But generally speaking, most people say that they don’t feel that energy boost until one to two days later, even sometimes the next morning even. But I wouldn’t say that I would see that directly after NAD and at least definitely not enough to really benefit the neurofeedback.
Dr Mike T Nelson: Yeah, that’s what’s interesting because That’s what I have no idea of. Like is, some of these things are obviously have delayed effects because of signaling and everything else going on too. Like, it just seems like we don’t really [00:29:00] know what exactly that time course is at all either.
Speaker 5: Have
Dr Mike T Nelson: you ever thought of using.
This may not be available yet, but like, ketones or something like that as a fuel source for like concussion or brain injury or anything like that, or is it just not really available? So it’s not really an option.
Jordyn Payne: Yeah, I wouldn’t say that it’s necessarily available to us as of right now for our practice, although I have looked into it and other like research type facilities.
We have we are only about 2 years old. Our practice are 3 years old. At this point. I’ve been here for 2 years. But we are looking at expanding into other, alternative treatment types, like using ozone therapy, keelage, IV chelation. So we’re hopeful to see those two things come into our practice here soon.
I know that we’ve seen a lot of a lot of requests for both of those things. So we’re looking into implementing [00:30:00] that, but no, with the ketones as of yet, we have not started implementing that.
Dr Mike T Nelson: Yeah. Very cool. Tell us about a Myers cocktail and then after this we’ll talk about HBOT a little bit.
It seems like that’s the OG and I’m always curious like how did that get started? Because as long as I’ve been familiar with IV therapy, like it seems like Myers cocktail was like the original one.
Jordyn Payne: Yeah, so my cocktail is so good because we’re replenishing a lot of electrolytes, right? So, we’ve heard of folks, post hangover, they want an infusion and they get a banana bag, which is typically the base of that is potentially a Myers cocktail, where we have magnesium and a lot of different B vitamins and including B12, we have vitamin C and There’s a few other electrolytes within there.
So generally speaking, we’re talking about increased hydration. We’re looking at these, this electrolyte replenishment, but the B vitamins in particular, I think, the most beneficial part of the Mars [00:31:00] cocktail because B vitamins are used often as a cofactor for so many of the other antioxidants in our body.
In particular, we see it with glutathione, which is another infusion that we do, which is an antioxidant that occurs in the body. As and glutathione is really beneficial for working on that mitochondrial health. So oftentimes I will give a mito Myers cocktail not only just to feel good because it does, B12, vitamin C, all these good things are going to help you.
have a little bit more energy, feel hydrated, et cetera. But also I give that and then do the glutathione so that it is able to circulate throughout the body for a longer period of time. As it uses those B vitamins as a cofactor. So yeah, it’s the base for everything that we give because ultimately it’s just going to potentiate all of these other nutraceuticals and help them be more efficacious.
Dr Mike T Nelson: And the Myers cocktail I believe that could be. A little bit of variation, like going to a restaurant and ordering whatever, pick your favorite dish. [00:32:00] Like each sort of chef has their own little, Oh yeah, a little of this and a little of that, and I’d take this out, that type of thing.
Jordyn Payne: Yeah. So that is true.
And I think it’s important to, when you are going to be purchasing a Myers cocktail from somewhere, really understanding what you’re getting, because we always try to use a little bit higher. Potency of these nutraceuticals so that we really are gaining that maximum benefit. Because, yeah, there isn’t one set standard of what the Myers cocktail looks like.
Yes, there is the general idea of which nutrients are involved, but the dosing is not regulated. So, so understanding how much of each vitamin you’re getting is it was pretty important when you’re looking at if you’re comparing products from one place to the next. And unfortunately, a lot of locations are do not have that information readily available or not very forthcoming with that.
I did recently. Within the last year I changed compounding pharmacies for Myers cocktail [00:33:00] to something that is a little bit more potent. And I feel works better, but in doing so, I was still using the same fluid, 250 milliliters of normal saline and patients were complaining that it was actually burning now.
I was like, Oh, well, this is because it’s more potent. So 500 milliliters of fluid. Patients respond beautifully. And again, that’s also more fluid for assuming that you don’t have a fluid retention issue. That’s beneficial for somebody who’s looking for that hydration benefit.
Dr Mike T Nelson: Yeah.
And last question, we’ll ask them stuff about each. If someone’s listening to this and they’re like, Hey, I’m interested in trying some IV therapy. I, it like TRT clinics. It seems like IV therapy places are popping up everywhere. There’s at home services and I’m sure a lot of them are good, but anytime I see a.
Exponential increase like that. I always wonder about, quality. And is it going to be a race to the bottom? So for the consumer, for someone who’s [00:34:00] interested in doing this, what would be questions if they’re not able to come out to your facility in Virginia? What would be like your questions of like, hey, what’s You know, when you’re looking at a new place, make sure you ask them this and ask them about this and what would you have on your list of questions?
Jordyn Payne: Yeah, when it comes to the IV therapies, I definitely would ask, what are the doses? What is the concentration of the nutraceutical that you’re giving me? Are they giving you just a hundred milligrams of glutathione?
Speaker 5: Yeah.
Jordyn Payne: three grams of glutathione. We could like we will do sometimes. Are they giving you, what are the doses within their Myers cocktail?
They should be able to supply what pharmacy they get these nutraceuticals from so that you can make sure that it’s a reputable compounding pharmacy. They should be able to tell you exactly what the Doses of each vitamin that’s within that Myers cocktail is again, every single thing that they’re giving you, they should be able to give you that information readily.
That should be readily available. You can even ask [00:35:00] as far as you want to for their policies and procedures and how they are making sure that what are their certifications, are, is the person that is giving you an an iv, are they a. Are they certified to do so? Are they a nurse, or I, you can even ask what their medical director, what their credentials are, because sometimes we’re seeing these places are not necessarily being run by people who are certified to do so.
So I think that any questions that you have as a patient, you have a right to ask them and they have a responsibility to answer and no question is. I think at the end of the day when we’re talking about safety in particular, we want to make sure that we’re getting drugs from reputable sources.
As a matter of fact, we actually had an incident once where even a reputable pharmacy was had a, their NAD was coming from a supplier that I guess was under Investigation and ultimately was causing side effects that it shouldn’t have been causing. So [00:36:00] we had to take that off the market, and go find a new reputable compound pharmacy.
So, you just have to be really careful and ask those questions. Generally speaking, these places are not going to be giving you high doses of things. So, most of the time, there aren’t as many risks. But you’re also not getting as much reward. So when you’re paying, a significant amount, you want to make sure that you’re getting what you’re paying for too.
Dr Mike T Nelson: Yeah. And I view it as very similar to the supplement industry. Like if you just ask good questions, like pretty much all the time, the places that are doing it above board want to tell you what they’re doing and show to you that, Hey, We are doing this. We get these from a reputable place.
Here’s our traceability. Here’s the exact, amounts. Here’s our licensing here because all those things are expensive. They cost time, they cost money and all the [00:37:00] places I’ve ever been associated with or even some of my companies, they want consumers to be more educated because it’s also in their best interest because they’re spending the money to do it.
The better way and they don’t want a bunch of, low fires taken away from their market because then something bad happens. It makes the whole industry look bad and all the stuff that goes into that.
Jordyn Payne: Yeah. And also I just considered preservatives. Are you getting something that is contaminated with a lot of preservatives?
Are you getting something that what is it a derivative of? Are there additives that you’re not aware of? And that goes for oral as well. We usually use a full script as our, Oral supplement pharmacy because typically they’re pretty reputable and making sure that they’re only supplying the best products.
And I particularly like their encapsulations for their products because there are no typically not any additives to that supplement that you’re taking. So those are good questions to ask as well.
Dr Mike T Nelson: Awesome. Anything else you would add on IV therapies? [00:38:00]
Jordyn Payne: No, I don’t think so. I think most patients, most people are good candidates for IV therapy.
Especially once we start hitting the middle age reign because we do start our body stop making and producing as much of these nutraceuticals as they once did. So replenishing that no matter who you are is beneficial. And I think just making sure that whatever you do is tailored to your individual needs.
Dr Mike T Nelson: Awesome. And you also offer hyperbaric oxygen therapy, like what would you see for, let’s say, people who are more looking for health, longevity, athletic performance to start? Like what, is it something that they are typically requesting or is it something you’re looking at, hey, here’s what you want to achieve, like here’s our direction we think might be more beneficial for you?
How does that work?
Jordyn Payne: It’s a little bit of both. I would say oftentimes when we’re looking at folks from a general wellness perspective, athletic performance perspective, they’ve usually sought us out, [00:39:00] right? They have heard from someone that hyperbaric is beneficial. What their goals are and what their history is really going to direct treatment.
There’s a general protocol that we follow that I have seen work well for folks. And ultimately, it also comes down to what they, what their financial Ability is too, what they’re able to afford that is going to also impact their decisions. But ultimately, I’m going to make a recommendation of what is going to work best for them, and then they can go from there.
Because the beauty of this type of medicine is that although it’s frustrating that insurance doesn’t cover it, we’re also not bound by insurance.
Speaker 5: Right? And all those restrictions.
Jordyn Payne: Right, we have less restrictions. We can tailor it to your individual needs and desires and want, whatever is going to work best for you.
And so we don’t typically have to treat as aggressively with hyperbaric therapy when we’re looking at somebody who is just hoping to improve general [00:40:00] performance and decrease inflammation and help with their overall health and wellness. With hyperbaric therapy, a we call it diving, like scuba diving, because it is the equivalent of, descending a certain level of feet below sea level.
When I look at patients who are looking for general wellness. And performance. I generally recommend somewhere between 1. 5 atmospheres, which is about 15 feet below sea level to 2. 0 atmospheres, which is about 33 feet below sea level somewhere in there. And then they do 60 minutes at pressure which means about an hour and a half in the chamber.
And so it’s really going to be dependent upon their history too. Especially when we look at athletes, I have a lot of athletes come in that have a history of a concussion. even if it was just one, yeah, or some type of injury or otherwise. And so that is going to affect the treatment protocol for them.
And sometimes I’ll start them off at [00:41:00] that 1. 5 range, see how they tolerate it and slowly descend deeper down to 2. 0 as tolerated. But I’ve seen a lot of benefit with hyperbaric with, most patients that walk in, regardless of what they’re there for, have noticed noticeable benefit with hyperbaric therapy, especially when we talk about traumatic brain injuries.
And generally I would say India and Israel are on the cutting edge, the forefront of hyperbaric therapy. So we do refer a lot to their research as to what works, particularly when we’re looking at cognitive dysfunction and neurological conditions.
Dr Mike T Nelson: And this is probably a huge speculation, but with athletes, do you think the hyperbaric is helping them Get a little bit back to baseline or above baseline because they’ve probably had a concussion where they’ve been released and your air quotes normal, but there’s [00:42:00] probably still some resonant effect from the concussion that you think the hyperbaric is really impacting.
Or what do you think is if you were to speculate on kind of mechanisms, which. Again, it’s going to be widely different, depending upon even just in healthy individuals.
Jordyn Payne: If an athlete comes in and has had a history of a concussion, right? If there is Still damage. If there is an area that may not be getting as well perfused, there’s not as much circulation blood flow to a certain area of the brain.
In theory, hyperbaric therapy should help improve that,
Speaker 2: right?
Jordyn Payne: So yes, theoretically, if they have a history of a concussion or injury, we should see improvement in those areas. Oftentimes, when we see the symptoms that we see of maybe a long term concussion or like a post concussional type syndrome, we’re going to see that brain fog, that almost like cognitive [00:43:00] lag.
Sometimes you see difficulty with word finding, but they’re maybe not bad enough for the individual to have said, Oh, I have this problem. They’re just like, Oh no, that’s just my daily issue. And it’s like, well, yeah, but that’s
Speaker 5: not
Jordyn Payne: normal. So we and often sleep disruption is an issue with that too.
So typically the first benefit that I have patients tell me that they see is an improvement in sleep. Whether that’s what they’re being treated for or not, I generally would say within 10 dives, 10 sessions, I see patients say, Oh, my sleep has approved. And they’re very excited about that because they’re not even necessarily expecting that.
But when we’re talking about a neurological impact, if we’re talking about traumatic brain injury or concussion. That can take, 40 to 60 sessions to really see full benefit and they don’t really start to notice that benefit until about 20 sessions in. But I would say that for an athlete.
Yeah, I think that sometimes it’s bringing them back to [00:44:00] baseline. Sometimes it is just improving their performance. No, we are going to be better oxygenation throughout the body. We’re going to see faster recovery time. There’s some. research that suggests that there’s some preventative benefits from hyperbaric therapy that we are seeing that, that cell turnover happen at a faster rate that we’re seeing that detoxification process happen faster.
So when we’re, having intense workouts and things, we can see the body get rid of. Any toxin buildups faster with hyperbaric therapy, we’re decreasing inflammation innately. So having that decreased inflammation is going to prevent, uh, help prevent injury in general. And we’re going to recover from injury faster, whether that’s injury at a cellular level.
Or at a more physical level, like, a knee injury, I had a patient who was a field hockey player and she tore her hamstring and had a hamstring repair and then did hyperbaric all summer and was [00:45:00] able to practice with her college that fall. So, that was pretty big she recovered much faster than it, than she would have otherwise.
Dr Mike T Nelson: Well, it’s super interesting, the neurologist I go to the Functional Neurology Center, so Dr. Jeremy Schmo they just put in hyperbaric, I think, maybe eight months or six months ago, and he’s pretty good about reading all the research and, runs a practice, and he said it’s been, very beneficial so far, which I find fascinating.
And you said like the minimum for if we just divide them into normal, healthy people looking for athletic performance, maybe it’s 10 sessions and concussion, something like that is probably a minimum of 20. And that’s the numbers I’ve heard thrown around too, that you might see an acute effect, but.
It’s like anything else. It’s like exercise. If I go to the gym once, like my right bicep’s not going to get much bigger no matter how many curls I do. But if I go again and again, I get these, small benefits that do add up to a positive adaptation over time. [00:46:00]
Jordyn Payne: Yeah, I would say that’s a pretty good baseline for a minimum.
But again, that is also going to depend on the individual and what they’re putting in their body. So yes, the athlete may recover faster than somebody who had a fall in a nursing home and developed a concussion, right? So the way that person’s going to bounce back from that concussion. is going to be dependent upon their lifestyle as well and whether or not they were already doing hyperbaric therapy prior to the concussion.
I think that there is an argument to be made that if you are already doing that, your body is going to recover faster and you may need less hyperbaric in the future when you do have a concussion. Maybe you do need only a 10 day boot camp. But if we’re looking at somebody who has generally a post concussional syndrome, which is, long term effects of even just one concussion potentially.
I would say it’s more realistic to consider 40 to 60 treatments, purely because that neurogenesis, that new nerve cell [00:47:00] formation or cell formation doesn’t really start to occur until dive 20 as well as angiogenesis, which is where we’re going to have that new Vasculature form right over time, though, at a cellular level, we really start to see that occur around dive 20.
and that’s why I typically have found most success with doing at least 40 sessions to really. Go at least back to baseline, if not more improved than baseline.
Dr Mike T Nelson: Yeah, and I believe even the in clinic versions of HBOT are quite different. Do you want to speak a little bit to that? Because, again, I’m not an expert in this area at all, but I’ve seen what I would say look like.
Very shoddily made H Bots that were sold at a clinic by shady looking companies. And I’ve I tried one other very high end, like, hardshell unit that’s, again, just looking at them in person. It just looked like there was a night [00:48:00] and day difference between some of the very, I would say, shady companies versus the companies, trying to do it well.
Jordyn Payne: Yeah, so a lot of places are using what’s called soft shell chambers. Okay. And those are the ones that you’re going to see are more of just the fabric canvas style and they have a zipper and maybe they have like three layers to them with the birds.
I don’t think you’ve done real hyperbaric. That is not a bad thing. It’s not an innately bad hyperbaric setting, but it’s not going to have the same benefits as an acrylic hard shell chamber. Much more
Dr Mike T Nelson: limited, I would say.
Jordyn Payne: It is, because ultimately they’ll say that it can descend to 1. 5 atmospheres, but generally speaking, research has shown that these soft shell chambers really are only descending to about 1.
3 atmospheres. And because they are not an acrylic chamber, even though they may be Pumping in 100 percent oxygen, you’re really only the body’s really only observing about 70 percent real oxygen, right? Because ultimately, it is going to be [00:49:00] escaping to some extent. So, so not that it’s necessarily inherently bad, but it’s not going to have the same effect as these hard shell chambers.
I can we have our model place chamber. So 1 individual per chamber. And they just aren’t, it’s really like comparing apples to oranges at the end of the day because they’re not really even comparable. I did have a patient once who had his own soft shell chamber and he actually got stuck inside of it and he couldn’t get the zipper to open and so, yeah, so it traumatized him for life.
So then he started coming to us and he was like, Oh, I feel much better here. Like, yeah, I bet you do. So that was an interesting case. Now, unfortunately, if you’re going to an actual center, hopefully they would be monitoring you. And but that’s another issue is those centers are often not they don’t necessarily have certified hyperbaric specialists.
They don’t. Have not that it’s a super regulated [00:50:00] therapy, but in general reputable place is going to have more rules and regulations and are going to have policies in place that are going to mitigate risk factors like oxygen, toxicity and oxidative stress. Fire has been a big topic lately.
We make sure that folks are only wearing a hundred percent cotton that any fabric that’s within the chamber is. is hyperbaric approved. We use grounding straps and there should always be a hyperbaric tech, hopefully a certified hyperbaric tech within the room supervising the chamber at all times.
And you can’t necessarily guarantee that anywhere, but if I would say that anybody who’s interested in doing hyperbaric therapy, look into these things before pursuing it, making sure that wherever you go these, Policies are in place and that they are reputable and that their hyperbaric texts are.
Certified and are, and that they’re, they have these safety precautions in place because there are risks involved [00:51:00] like anything recently started doing airbrake halfway through everybody’s hyperbaric treatment because it actually tricks the cells into reuptaking more oxygen because you’re causing an oxygen deprivation right in the middle.
And it also mitigate some of that risk of oxidative stress and toxicity.
Dr Mike T Nelson: Yeah, that was one of my kind of out there questions, like there’s systems on the market now for exercise, which again, this is, it’s not HBA, but in terms of if we look at oxygen regulation, one of them is live O2, I don’t have any disclosures with them, but the theory is that during exercise, again, for healthy individuals, we can give them a high percentage of oxygen, And then we can immediately switch them to be more hypoxic and back and forth.
And at least on the exercise performance realm, the data on each bot I think is a mix. There’s just not a ton of it for exercise performance. We do know that if you can [00:52:00] stick people In a hyperoxic chamber that you will definitely see more exercise performance acutely, right? Because you’re driving more oxygen into the cells.
Now, does that transfer outside of that? There’s a handful of studies that are again, very mixed on that. But like you said, maybe you’re dealing with someone who has a concussion. Maybe you’re dealing with, a bunch of other things where it definitely can be helpful, but do you think there, the future is.
Maybe having that switching be more part of it. Because if you look at a lot of, my buddy Kal Deet sent me this stuff of like the old Russian research, which again, that just sounds cool, but doesn’t mean that it’s always correct. Their argument is that for athletic performance, you have to create a hypoxic environment first, and then the hyperoxic environment is much more beneficial because of that.
Now I don’t know if that applies to non exercise, to pathologies, or The thinking on that, like you’re saying, with an air brake, does that then have more of [00:53:00] that switching involved? And does that, appear to be more beneficial?
Jordyn Payne: Yeah, I definitely I definitely can get behind that thinking, right?
That is one of the things that we recently have seen some newer studies that have come out that show that if you deprive the cells of oxygen, or even trick the cells into thinking they’re deprived of oxygen, They will almost become more oxygen hungry when you reimplement that high dose of oxygen.
So yeah, I would say that is along the same school of thought and that’s how we have seen it be make hyperbaric even more efficacious. But again, it also helps reduce that oxidative stress component. Because it is giving those cells a break as well to help them filter the oxygen at a better capacity.
Dr Mike T Nelson: Awesome. Last question on hyperbaric. What are your thoughts about the kind of at home units? And I don’t want to blame this all on the biohackers, but it seems like Oh, if it’s good in a clinic, we’ll just make it at home [00:54:00] unit and I read, like, something online, so now I’m just gonna do HBOT at home because I spent a couple grand on this crazy unit.
Jordyn Payne: Yeah, so, my patient got stuck.
Dr Mike T Nelson: I know, exactly, I’m just like I,
Jordyn Payne: These things worry me. Yeah, the only reason he was even able to get out of it was because he had like 1 percent battery on his phone. He had, at the time, a concierge type physician who sent one of their techs over, like one of their nurses over, and they were able to get him out of the chamber.
That’s the only reason he got out.
Speaker 5: Oh!
Jordyn Payne: Yeah. So, maybe I’m a little biased because of that incident, but I tend to believe that, and that was a person who has done many different ex NFL athlete. This is a person who has had all these resources and all types of experience.
And this happened to him. I can’t say that I can’t expect that in maybe the layman as well, so no I don’t know. You know what, if you’re going to get something, get an infrared [00:55:00] sauna for home.
Dr Mike T Nelson: I just think there’s a lot of other lower risk things you could be doing first. I don’t know.
That’s where my brain goes to. I agree.
Jordyn Payne: That’s, I tend to be on the same page with that. I really think there are some other alternatives that you can do at home that are going to be really beneficial. And the more that we look into, the hyper and hypo, training. I think that there will be home devices.
I think there are some home devices. They are. But I think as those become more available, there’s a little bit less risk there of doing that on your own. And I think that there are some alternative treatment options that you can do at home that are going to be really beneficial. And we don’t need to go into trying to do hyperbaric.
on your own. And I don’t even think that it’s that beneficial. These soft shell chambers are not nearly as beneficial as these other alternative treatment options. And I’m doing acrylic hard shell chambers. So is it worth it? I don’t think so.
Dr Mike T Nelson: Yeah. That’s my advice. I’ve had a handful of people reach out and ask me about it.
And I’m like, I’m not an expert. I can tell you at [00:56:00] least looking at effect size and research. Maybe clean up your diet a little bit. You’re eating like a trash bin fire, sleeping four hours a night, drinking eight cups of coffee. You probably have some other low hanging fruit you can work on.
Jordyn Payne: Your hyperbaric is not going to work as well because it’s just going to be combating that all the inflammation that you’re already causing.
So now we’re combating, or people who are drinking alcohol the night before, hyperbaric, well, we’re just fixing that all the inflammation you just caused last night, we’re not getting to the nitty gritty of what we actually need to repair.
Dr Mike T Nelson: Yeah, I agree. And then even that, and when they are still insisted upon doing it, I’m like, you’re not my client, but for God’s sake, you appear like you have enough money.
Go find a decent clinic. That’s going to do it in a regulated place. You’re going to be watched. They’re going to give you a better protocol. They’re going to titrate it to your needs and your background. Instead of feeling like. You’re going to go try this on your own just because you can spend the money to have one in your house.
That seems like a bad idea.
Jordyn Payne: I agree. Right. Yeah. I’m on the same page. [00:57:00]
Dr Mike T Nelson: Yeah. Well, if you ever want to file any patents, I think of, have you ever seen those old patents they had? God, it’s probably several hundred years ago with the. The escape systems they had in coffins, they were so afraid of people being buried alive that they had multiple different patents filed for, a bell you could ring that would be above ground to like escape hatches to, I don’t know, I just keep thinking of maybe you need something like that for your You’re hyperbaric.
Jordyn Payne: If they’re going to do these soft shell chambers at home, they just need a little life alert. Yeah, like a
Dr Mike T Nelson: little life alert or like something. I don’t know. Yeah.
Jordyn Payne: Yeah. After seeing the one guy get stuck, well, I don’t wish that for anybody.
Dr Mike T Nelson: Yeah. Awesome. Any other things you’d want to add as we wrap up here?
Jordyn Payne: No, I, I think we’ve covered a lot. I think that in general looking at preventative medicine, anti aging medicine performance medicine, and I even hesitate to say the word medicine because ultimately it’s just these [00:58:00] therapies. I think this is the future.
This is now, this is the present I think that we are seeing this rise and I think it’s all good and going in the right direction and I’m excited to see where everything goes.
Dr Mike T Nelson: Yeah, well thank you so much for all your time and sharing all your knowledge and everything, I greatly appreciate it. Where can people find out more information about you, especially if they’re out in the Reston, Virginia area?
Jordyn Payne: Yeah, so we’re on advanced brain centers of va. com. And that is the name of our practices, advanced brain centers of Virginia. You can also find us under HBOT of Nova. But yeah, advanced brain centers of va. com is our website and you can see everything else there is to know. And we have a lot of research linked there as well.
And you can always give us a call. Our number is on that site as well as at 5 7 1. 828. Oh, nope. I forgot the phone number.
Dr Mike T Nelson: That’s right. We’ll list it.
Jordyn Payne: I don’t usually do that part. [00:59:00] You can go on our website and you can find our phone number and you can get in touch with us and we can definitely set up a consult at any time.
Dr Mike T Nelson: Perfect. And I think you do longer programs for, people who are able to stay for maybe a few days, a few weeks, things like that too, for people that, fly in from other areas, correct?
Jordyn Payne: Yeah, we do. We have, month long programs, two month long programs. It just depends on the individual’s desires and needs and what we can do for them, but we also have, some patients come once a month,
Dr Mike T Nelson: you
Jordyn Payne: know, so it just depends on the individual.
Dr Mike T Nelson: Cool. Awesome. Well, we’ll make sure to link to all of that and yeah, thank you so much for all your info. I really appreciate it. That was great.
Jordyn Payne: Thanks for having me.
Dr Mike T Nelson: Awesome. Thank you so much.
Bye.
Speaker: Thank you for listening to the podcast. Really appreciate it. Huge thanks to Jordan. Make sure to check out all of her wonderful stuff there. at the Advanced Brain Centers of Virginia.
We’ve got the links there and everything. You can call them if you have any specific questions. They [01:00:00] do great work, so I would highly recommend if you are looking at those as some potential therapies to check them out. If you’re interested in more advanced bleeding edge stuff to increase your body’s ability to recover, Just generally be much harder to kill.
Check out the physiologic flexibility certification. It’s still open now until march 24th at midnight pacific standard time 2025 Best place is to get on to the free insider newsletter and I’ll have all that information as it is live You can hit reply there ask me any questions more than happy to help you out Big thanks to all of you for listening.
Really appreciate it. Thank you so much If you can give us the old and the download and leave us a review Whatever stars you think is appropriate That goes a long way to helping us with the algorithms and get better distribution so we can continue to get great guests on the [01:01:00] podcast. Thank you so much for listening.
We really appreciate it. And we’ll talk to all of you next week.
Great little actress. Yep, and getting smaller all the time.
Speaker 3: This podcast is for informational purposes only. The podcast is not intended as a substitute for professional medical advice, diagnosis, or treatment. You should not use the information on the podcast for diagnosing or treating a health problem or disease or prescribing any medication or other treatment.
Always seek the advice of your physician or other qualified health provider before taking any medication. Or nutritional, supplement, and with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have heard on this or any other podcast.
Reliance on the podcast is solely at your own risk. Information provided on the podcast does not create a doctor patient relationship between you and any of the health professionals affiliated with our podcast. Information and statements regarding dietary [01:02:00] supplements are not intended to diagnose, treat, cure, or prevent any disease.
Opinions of guests are their own, and this podcast does not endorse or accept responsibility for statements made by guests. This podcast does not make any representations or warranties about guest qualifications or credibility. Individuals on this podcast may have a direct or indirect financial interest in products or services referred to therein.
If you think you have a medical problem, consult a licensed physician.





Leave A Comment