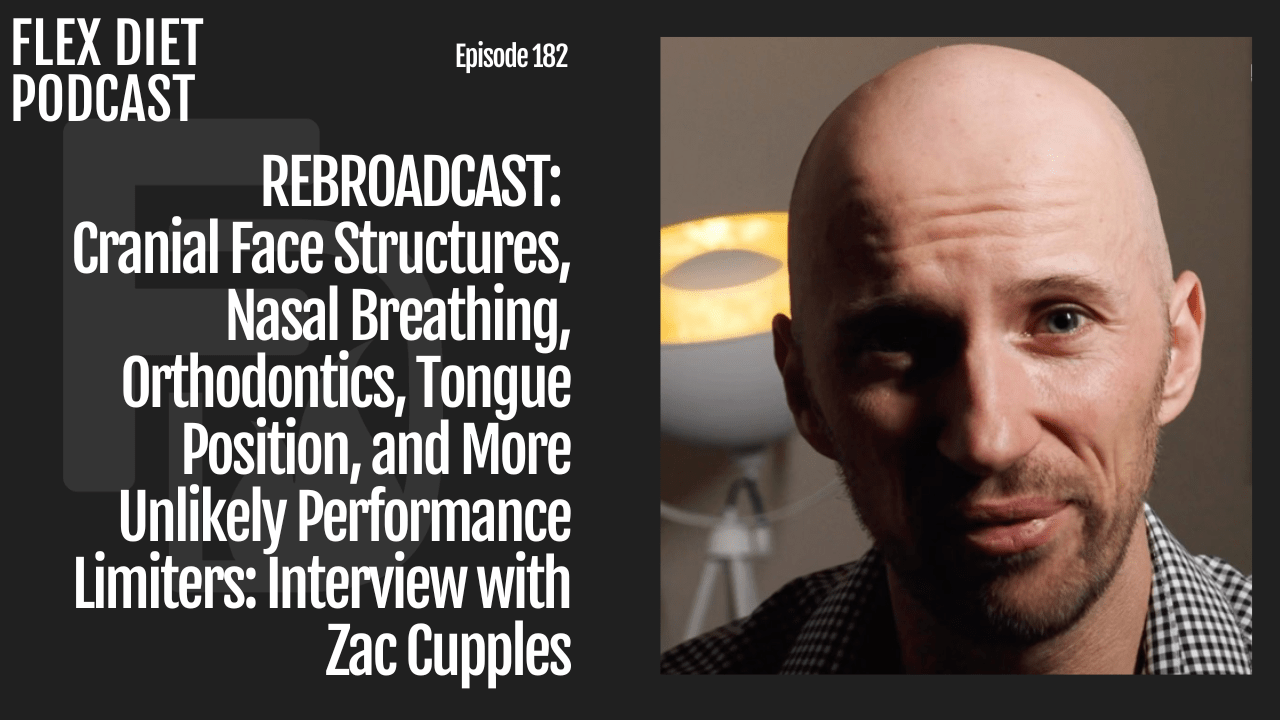
Enjoy this rebroadcast of an earlier Flex Diet Podcast episode. My wife Jodie and I talk with Zac about rate limiters on performance like palate issues, teeth movement, and function, as well as how to get a good sleep study (what to look for and what to ask for). We offer advice on what to do if you feel like you need to seek more information.
The Flex Diet Certification is open for enrollment the first week of January 2023. Go to flexdiet.com to enroll. If you’re outside of the enrollment window, sign up for the waitlist, and I’ll notify you when it opens again.
Episode Notes
-
[7:49] How Jodie avoided dentures
- [10:57] Zac’s background and how he got into this field
- [19:43] What proper mouth structure should be
- [20:36] The connection between sleep and mouth structure
- [23:41] The connection between ADHD and other behavior issues and airway
- [34:22] What to ask for with a sleep study
- [51;39] Addressing oral posture sooner rather than later
- [55:20] How much can you change
- [1:04:35] Recommendations on what to do and where to go
Find Zac:
Rock on!

Dr. Mike T Nelson
Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
[00:00:00] Dr Mike T Nelson: Greetings and welcome back to the Flex Diet Podcast. I’m your host, Dr. Mike T. Nelson. I hope you all had a wonderful Christmas, happy holidays. And today I wanted to do another rebroadcast last one of this month. Again, this is one of the episodes. It’s been in the top 10 of all time downloads of the podcast.
And it’s with my good buddy, Dr. Zach Couples and talking about something that’s a little bit off topic but it is related to performance. We’re talking all about cranial face structures, nasal breathing, orthodontics, tongue position, and what we will call unlikely performance limiters. And my wonderful wife, Jodi, is on the podcast here also, cuz she’s still in.
Process with Zach’s help and some other professionals help here of going through all of this as we speak. So I thought this would be a good podcast with some great information for you, and wanted to remind you that the Flex Diet certification will open again at the beginning of January. So coming up very soon, if you wanna learn how to get your nutrition and recovery.
Up to speed and also learn why the concepts of flexible dieting in a metabolic flexibility can be super useful for you or if you’re a coach for your clients. Flex Diet goes over eight different interventions. Everything from the macronutrients like protein, fats, carbohydrates to techniques such as intermittent fastening, exercise sleep improvements, micronutrition, and much.
So go to flexdiet.com for all of the information. You’ll still be able to get onto the wait list and you’ll be the first to be notified. I’ll probably have some bonus items for you also there. That’ll open the first week, coming up here very soon of January, 2023.
So thank you so much for listening to the podcast and being on the newsletter and everything for this year. Really appreciate it. And thanks for listening to the intro, before the intro. And here is the rebroadcast of this episode. Dr. Zach Couples on cranial facial features, nasal breathing and unlikely performance limiters.
Thank you.
[00:02:46] Dr Mike T Nelson: Hey, welcome back to another episode of the Flexed Diet Podcast. And today we’ve got two special guests. My wife Jody, joins me on this podcast as a co-host, and we talk to our good friend Zach Couples. And as the Flex Diet Podcast is focused on adding lean body mass and a better body composition, all without destroying your health in a flexible based approach.
And today we deviate a little bit from that topic, but it’s definitely related. So one of the things I spend a lot of time thinking about in reading research on is what are some of the limiters on your physiology? So for example, even if your goal is to add lean body mass we’ve talked about in the past that maybe your cardiovascular system or your aerobic capacity.
Maybe a limiter. It’s not directly worked per se on lifting, but the replenishment of the atp, the energy you use is all aerobic metabolism based. And today we talk with Zach about all things related to upper pate in your mouth related to teeth movement and function, and a whole host of little bit more esoteric topics how to get a good sleep study, what to ask your physician for.
What are things to look for on a sleep study and why a sleep study will be useful for a vast majority of people. I’ve had the advantage of knowing Zach for many years. We’ve hung out together. Different conferences, Starbucks and Toronto. And even for many weeks at a time in Costa Rica, I had Dr. Ben House’s facility there at Flo.
Both of us have been presenters there and just got to hang out and live together and I always learned a ton of new stuff from Zach and I’ve been able to consult with him on various clients also. Cause I’ve had more clients recently and myself included, and Jodi included here. that have some upper palate issues, some breathing issues are looking to get orthodontic work.
And a lot of that stuff at face value doesn’t sound like it’s related to anything that we normally talk about on the podcast, but today we’ll get into the details of how. For some people, not everyone, it is very much related and the structure of your mouth and teeth might be a rate limiter. And again, at the end we tell you if you think this is potentially an issue, where to go, how to get started.
Because we’re discussing the overlap of many fields, and this is a new area that’s becoming a lot more popular. And the hard part with that is when you have overlaps of different. It’s unlikely that one person is gonna be the person that can do everything under one roof. So you’re gonna have to try to coordinate with different specialists and that can make it tricky.
Enjoy this podcast as always sponsored by the Flex Diet. Go to flexdiet.com, and you’ll be able to get on the wait list there to the newsletter, which is free for the next times that it opens. Flex Diet certification is eight different interventions related to nutrition and recovery that you can use to enhance your performance.
Body comp and health. It’s ideally designed if you are a trainer to work with yourself and your clients. So it’s a complete system of. Everything from how much protein do you need, how much carbohydrates, fat meat, which is non-exercise activity, thermogenesis exercise, sleep, fasting, ketogenic diets. How do you know to use those interventions and when do you use each particular want?
So it’s set up in a complete system based on metabolic flexibility and the concept of flexible dieting. So go to flexdiet.com, and enjoy this wide arranging podcast with my good buddy Zac Cupples.
We just wanted to get you on here to talk about just some of your experience and just some of the different stuff that’s becoming popular now from nasal breathing, mouth breathing structure. Jodi’s on here too cuz she’s, as going through all of that stuff right now. I’ll have an assessment when I get back.
[00:07:49] Jodie Nelson: I’m calling it narrowly escaping dentures. Doesn’t that sound sexy? , I had some interesting dental work that was done when I was in my twenties which was a bridge that should have never been put in place because the, I could have had a wisdom tooth move into that spot where the missing tooth was.
However, the dentist just went ahead and threw it in there. I have a missing tooth. Tooth on the top. And last Christmas Eve, that whole bridge that was in my mouth for over 20 years fell out of my mouth. And so as we started out the journey of trying to find the right luckily his sister said, , make sure that you know what the oral sur don’t just do a regular dentist because they can yank stuff and you won’t be able to ever get an implant.
And I’m so glad that she said that. So she knows an oral surgeon, she’s a nurse anesthetist, and she has worked with particular ones. She recommended him, he recommended an dentist, an orthodontist, which we didn’t end up going with. Because I was thinking, as long as we’re messing around with my mouth, this is gonna be for the rest of my life fixed.
So this is gonna be the thing that I’m gonna have going on for the next three decades. So I’m going to really do my homework. I wanna know if I have any breathing issues, I wanna know what else is going on. And of course, it’s not just one answer. I’m finding that some trauma. I had a near drowning experience that I never really thought of as.
Impactful to my life, which shut things down in the back of my throat. And just so we’ve got the breathing issues. I don’t just wanna start yanking teeth around because if the foundation’s not good and I’m still clenching my jaw and I’m still doing all of these things, then eventually it’s not gonna change things for the better.
So that’s why we’re on this journey, which I find fascinating cuz so many different pieces like interlink into this whole thing. So that’s why.
[00:09:54] Dr Mike T Nelson: Yeah. That’s why we wanted to get you on the podcast too, since we’re already recording anyway about just your background and your journey and how you got into this.
And then Jodi can talk more about her experience and I’ll have an assessment in December, probably once we get back home, so I’m sure I’ll probably need some. hardware of some form. I talked to Ron years ago at P R I when they did some of their stuff and he’s I haven’t done a formal assessment or anything.
He’s but odds are you probably need an appliance or something like that going on. Yeah. I guess the starting question then is how did you get into this area looking at different mouth structures and T structure and it’s becoming more, I don’t wanna say sexy now, but I mean I first heard about it from Ron a PII probably six or seven years ago.
And at the time I was like, what dentist? What are you talking about? You’re a physical therapist. What does dentistry have to do with it? It didn’t seem like it’s that connected, yeah.
[00:10:57] Zac Cupples: Yeah. To echo what you said, I think I first got intrigued by that when I was taking a lot of P r I coursework.
And it’s funny cuz. , like in, in physical therapy school, we learned about, tmj, tmd and doing different manual interventions for that, but not once. Did we ever talk about integrating with the dentist to potentially help with that? Yeah. So I will give credit to Ron because he at least took it to that next step.
Although it seemed as though in that case when, at least when I took the coursework several years ago, it was a little bit more biased towards occlusion. , which is how the basically how the teeth contact each other. Yeah. And then they would do things to improve upon that with a little bit of appreciation for structure of the pallet or the roof of the mouth.
I would say what’s really skyrocketed me getting even more in depth to this was going through some of it myself. In, let’s see, 20, I went and worked with Ron at the Prime oh yeah, the prime program. I did that I think 2013. Okay. He recommended I get my wisdom teeth pulled out just cuz they were not, I didn’t have room for ’em basically.
And they were all weird directions, so I got those pulled out. I couldn’t move my jaw side to side, so once I had that done, then I could move it side to side, which was intriguing. Interesting. Yeah. And then after that I, I thought, okay, what else can we do to improve this? A couple of my colleagues were getting the rotor rooter done in the nose.
So a septoplasty Yeah. To make more room for that. And so I was initially gonna get that done in Arizona. I’m so glad I didn’t. And this is where, when you’re going through this stuff, you really gotta make sure you have someone good and get a few different opinions. So the procedure they were gonna recommend was potentially shaving down the septum to Oh.
To make it even. But then they’re gonna take a turbinate out. So the turbinate basically helps humidify the air as you go in. Because it was enlarged. The problem is if you do that, you can get a condition called empty nose syndrome. Yeah. Where basically because the anatomy’s changed, you get a lot of the same symptoms you had before, in my case, difficulty breathing through my nose frequent colds.
And it doesn’t fix the problem.
[00:13:16] Dr Mike T Nelson: Yeah. So we had James Nester on the podcast and he talked about that as one of the potential side effects of people having a lot of procedures done right away to try to quote, unquote fix something. So he is yeah, there’s a potential cost to having stuff removed that may not, may not need to be removed.
[00:13:34] Zac Cupples: Yeah. Yeah. I would echo that a hundred percent. So I ended up getting the surgery in Memphis from a doctor who was, cuz I was working with the Grizzlies at the time. , he was connected with them and so he shaved down the septum very lightly and reduced the turbinate. So just made it a little smaller.
And I got profound changes from that, able to breathe through my nose. Like I remember I had plastic in my nose and took it out and it was just like I had never taken that much air in through my nose. And then within two weeks after everything healed out, my resting heart rate dropped 10 beats per minute.
[00:14:08] Dr Mike T Nelson: Yeah. I think I initially met you right after you had that procedure, I think. Didn’t you? Like you were here in town, I think for when you’re with the Grizzlies or something. God, I can’t remember. It was a long time ago. You were in Toronto. Toronto, that’s right. . Yeah, I remember
[00:14:24] Zac Cupples: that. Yeah. I remember taking the picture with you and yeah, it was Starbucks or
[00:14:28] Dr Mike T Nelson: some coffee.
Yes. Yeah. Starbucks, .
[00:14:30] Zac Cupples: Yep. Yeah, I, it probably cuz it was during the all Starbucks breaks. It would’ve been in February and yeah, Toronto was cold all the time, so we, yeah, happened. , but then I would have to, I have to give credit to my friend Joseph and Nelly a physical therapist. We both studied under Bill Hartman and he’s been working up in San Francisco for quite a while now.
And he introduced me to, to Dr. Brian Hawk and was really into just a lot of different airway stuff that I had never even been exposed to. And so it’s like PT school where you looked at the jaw pr I was a little bit more occlusion and then we just kept moving backwards and that’s where the stuff that I’m doing now and I’m exposed to now I think has been a real big difference.
Cuz the issue even with fixing the deviated septum is the septum only accounts for about 20% of the area. Get through your nose. Remaining 80% is impacted by the floor of the nose, which is your roof of the mouth. Ah, yeah. So doing things to affect the. Oral posture and the oral airway can a lot of times have a profound effect on how well you breathe through the nose.
And the issue that I found if someone’s trying to go down this route is you really need someone who looks at all the potential pieces. And then from there it’s really trial and error of what works and what doesn’t. Because there’s not really like a set playbook for any specific case, especially when the dental history gets a bit more extravagant.
Like in your case, Jody,
[00:16:00] Jodie Nelson: I like that you chose a positive word, for that. Extravagant . That’s nice. .
[00:16:07] Zac Cupples: Yeah. So that’s where I’m at with it now. And I’m I’m going through some stuff personally. I’m trying to think what else I’ve tried. So I had, in 2019, I had a tongue tie release. So I was, I had a slight tongue restriction.
and so we ha I had Dr. Sarus Zaggy, who’s like the guy for this stuff. He’s in la. He he did my tongue tie release. Joe is doing my malfunctional therapy, which is basically like physical therapy for the tongue. Got great range of motion. The way they test that is they would have you do opening and then they would have you go tongue tip to the roof of the mouth and then the whole tongue up to the roof of the mouth, basically measure the difference.
I was about 50% range of motion, which you could potentially get conservatively or with surgery. The surgery is for the cost, pretty low risk, high reward. So I got that done. But then the issue that I had now is I had all this range of motion, but I didn’t have room for my tongue. And that’s because my pallet is neuro side to side and front to back.
And that’s what got me hooked up with Dr. Hle. , we both have a couple colleagues who work with him. Yeah. Basically, so what we’re doing now for me is pushing my teeth out forward and sideways as much as we can both top and bottom. And the hope is that gives my tongue more room to sit on the roof, which can potentially affect the dynamics of the floor of the nose to allow me to better nasal breathe.
And the reason why we went with that is because I have a good amount of space in my throat For, from an airway perspective, there’s a certain amount of range you need to have, and I think the minimum you want is like 200 millimeters squared, something around there. And I think I’m in the, like the upper 300 s, which is good.
Because if I had a narrow or arrow weight, usually they recommend surgery as the fix where they basically cut the maxil on mandible and then bring all that Forward. Forward, yeah. Rotate it up. Forward. So it, but that’s expensive. So Yeah. I decided And very invasive . Very much yeah. It’s like a, it’s like a year or two year recovery process with six weeks of having the jaw wired shut.
But if you got sleep apnea Yeah. It is a hundred percent success rate. Yeah. Which I don’t have. I have upper airway resistance syndrome, which we found via sleep study. And so that’s kinda where I’m at. Since I’ve had the appliance three months now, I’ve my sleep’s been dramatically better. I used to get a lot of lulls like around noon.
Or mid-afternoon. Those are pretty much gone. I think I’ve had three in the last three months, which was like every day before that. So it’s been really cool. And so I’m doing that along with I’m working with a malfunctional therapist in town in Vegas who Melissa mug now, she’s really good.
To basically teach my tongue to get where it needs to go. Cuz that’s, I think the one thing I missed with. My first bout was we did a bunch of stuff for motion, but my ability to differentiate my tongue from my jaw or even my, my, my facial muscles just wasn’t there. And so we’re working a little bit on that now.
It’s been pretty, it’s really challenging. You get tired when you can get the tongue in the right position, .
[00:19:23] Dr Mike T Nelson: So if someone has a tongue tie, that’s absolutely not a guarantee that they’re gonna have issues. Correct. It’s just a indicator that, that may be limiting the range of motion of their tongue, or they just have lack of a better word, a dumb tongue that hasn’t really ever been trained to do more range of motion.
[00:19:43] Zac Cupples: Yeah, so it, it really depends on if you can get your tongue in on the roof of your mouth. And so ideally the tongue should sit up and forward and cover the entire roof of the mouth. Now, some people, if they have a large enough restriction, they might not be able to do that. . And so in that case, a surgery’s indicated.
Now other people can get the tongue up there, but they might compensate through the floor of the mouth, which is what I was doing. . So basically you would lift the floor musculature up on the roof of the mouth and then that could be a potential contributing factor to developing brx or clenching.
If you can get development of Tori, which is basically increased bone growth on the floor, on the mandible, which is what I have.
[00:20:32] Dr Mike T Nelson: Yeah. So do you have two that Yep. That I have that as well.
[00:20:36] Zac Cupples: Yeah. So if the tongue’s having to work really hard either stabilize the jar or get up to the roof of the mouth because the floor’s getting lifted, you can get increased bone growth there.
And that’s a potential indicator of some type of sleep disturbance. Y. Even if you’re not, you don’t have a restriction, you could still have a restriction because you’re just compensating through that. But there’s also some people who can just go through myofunctional therapy, teach their tongue to get up into that position if they’re not super restricted, and to ensure that, or to practice not using the floor of the mouth to create the lift.
And that can lead to some profound benefits. There’s good research showing that going through bouts of malfunctional therapy can reduce snoring and improve sleep quality in, in some individuals. It just depends on the severity of the sleep disorder. If you have fairly bad sleep apnea, it’s probably not gonna be the fix, but all of that’s assuming you have room.
And that’s really where I think most people, just because of us being a post agricultural revolution society are missing. .
[00:21:42] Dr Mike T Nelson: So would you say most people have a narrow upper pallet, both potentially width and depth, or is it more width or is it hard to say
[00:21:54] Zac Cupples: it? I would say most people, although there will be differences, have a reduction of side to side and front to back.
So if you’re someone who’s got an underbite, I think that’s a very clear example of, so an underbite or under jetjet would be where the b where the mandible sits ahead of the maxilla, the top part of your teeth. So in that case, most people have a reduction of A to P dimensions up top, interior to posterior.
Yep. Yep. So front and back. If you’re someone who’s got a more of an overbite or an overjet where the front part of the mouth is a little bit ahead of the back or of the lower. . The, some dentists would argue that you’re back on both. So the top of your mouth is sitting further back, but so is the bottom.
It’s just the bottom has gone even further back. Much further back. Yeah. And again, that’s likely due to us living in a agricultural revolution, society less breastfeeding genetics, because a lot of this is generational. And I’m mean, if you read Western Price’s book , you can see how fast the,
[00:22:58] Dr Mike T Nelson: yeah.
So two or three generations, I think they saw changes. I believe
[00:23:02] Zac Cupples: they saw they saw changes in tooth structure in the first generation. Now first Wow. Switch. Yeah. So it’s there’s a lot of factors at play. And then it’s, once the genetic predisposition is there, then it’s, even if you do everything right, you can still have these issues.
So most people have underdeveloped faces. Now the question is to what extent. . So what age do you catch that and intervene, and if you wait, to what extent do you have to utilize different strategies to try to increase those dimensions as much as possible so you have enough room for your tongue to sit up on the pallet and breathe through your noses?
[00:23:41] Dr Mike T Nelson: Yeah. Interesting. I, one of the other times I was talking to James Eser about this too, is my buddy Dr. Kevin Boyd, I met him at the Ancestral Health symposium years ago. They had a dentistry panel there and listened to him, and I was talking to him afterwards and I said, oh, what do you do? He is oh I’m a dentist, but I treat primarily kids with adhd.
And I’m like, hold on. Oh wait, what? You said you’re a dentist and you’re treating kids with adhd? It’s yeah, we image their airway and we find that a lot of kids who present with adhd, at least the people he sees in his clinic, their airway is like super reduced because everything has just been jammed.
Back in their face and they present as ADHD because their brain is literally not getting enough oxygen. So they become very sympathetic, they become very stressed, and ADHD is generally just diagnosed by the symptoms that you have. And he does a, more of an oral surgery approach, especially on younger kids.
And he said his success rate is almost like a hundred percent. And I’m like, oh, you mean they present with ADHD because their brain is literally not getting enough air? He’s yeah. I’m like, whoa that’s so crazy. And you think of all the kids who are on different medication, different things like that, who’ve never even had their airway image to see is that potentially an issue or not?
Again, it might be. It might not be. So that was probably maybe six or seven years ago, right? On the same time I was doing some of the p I stuff. And yeah, to me that was just, Fascinating. And now, fast forward it’s becoming more and more common, at least for people to have airway imaging. And I know when you went in, that’s one of the things they did with you was to look to see how much, volume you have in your airway also.
[00:25:24] Zac Cupples: .
Yeah. I think the we already know the wide range effects of sleep deprivation. Yeah. And while we’re doing a lot of things on a environmental or even behavioral aspect to improve upon that I think we’ve, over the years, been missing the importance of structure and that seems to be something that’s very under underappreciated, I think, because it’s still in its infancy in terms of how to best address this stuff.
But it’s so impactful. And I know for myself as I’ve gone through this, I haven’t been as stringent about the sleep environment, but my sleep quality’s been getting. dramatically better still. So it does make me wonder to what extent that’s really the driver of a lot of these issues compared to other things.
And to piggyback off what you said on adhd, there’s a research study that I read a few years ago where they did treatment for people with PTs D poster max stress. And it was just an oral appliance to help basically improve the airway dimensions while they slept. Symptoms reduced. Yeah. And it’s the same thing.
If you’re not getting a lot of oxygen, brain perceives that as a threat. ADHD sy, or not adhd, but PTSD symptoms may be increased because of that. Yeah. Yeah.
[00:26:42] Dr Mike T Nelson: And then I even wonder, I was doing some research on this, just reading stuff and there’s some preliminary data showing that if you have a traumatic event, what quality of sleep you get after that event may determine, do you get PTSD or do you get potentially post-traumatic growth from it?
So I’ve often wondered in that case, if you have someone who already has poor sleep because of facial structure, whatever else, they have a traumatic event, they have a history of getting very poor sleep. Now they get poor sleep for the next few nights after that, which messes with the amount of REM they see the processing of different brain and neural circuits.
So potentially is someone who’s gonna be put into a stressful environment, them having poor sleep quality going into that. Does that now become even a risk factor for them having a higher risk of developing PTSD once they have it? Like you were saying now they’re even more sympathetic at night and they can’t get into that more parasympathetic state.
So it’s just more like a downward spiral at that point then too, in terms of symptoms. Yeah,
[00:27:48] Zac Cupples: That would make, obviously I’m bias, we’re all speculating there. A lot of . Yeah. But I think even if there’s no link to that, With how important sleep is. Yeah. From a health perspective I, if you have the capability to do all in your power to improve, that, the effects on your health are gonna be wide ranging and probably worthwhile.
And that doesn’t mean that, as soon as you get an oral appliance, you can fire your, psychiatrist. Yeah. . But no, I’m gonna try this instead.
[00:28:20] Dr Mike T Nelson: Yeah. I’ll sleep my way through it, bro.
[00:28:25] Zac Cupples: that’d be awesome. But I still think it, it makes a lot of sense to at least do something to improve that, that the issue now though is there’s a large barrier from a cost perspective to get get. That’s really the hardest thing, I would’ve never been able to do this.
I would’ve loved to do this when I was running or even as a kid, but, with student loans and. , not growing up rich. I, there’s no way that this could happen. And it took me getting rid of my debt to be able, even able to think about going down this route, just cuz it gets costly and especially if you’re someone who maybe needs the surgery for the fix.
[00:29:04] Dr Mike T Nelson: Yeah. The surgery’s crazy expensive. Even like in, in Jodi’s case, like the first orthodontist we went to, just for the orthodontic, type procedures, that’s not putting in the implants or anything else. The person we’re seeing now, which I think is much better and much more holistic approach is literally three times the cost.
, so you’re, but I think it’s worth it. But again, to your point, it’s okay, so that’s an extra, $9,000 and that’s without having, one, two, or three implants put in. Yeah. That’s, this is not having a surgery, this is just doing, more of a full rounded, orthodontic type procedures too.
So it gets. Stupid, expensive, fast .
[00:29:45] Jodie Nelson: And the re part of the reason we, we chose who we did was twofold reasons. So the guy, the orthodontist that we went to originally, mouth breather, complete mouth breather. So it’s okay, so you know how to put the teeth to make ’em straight, but is there anything else you’re doing?
And the person that we chose she had to go to extra school and you remember what it is?
[00:30:14] Dr Mike T Nelson: Yeah. So she did orthodontic procedures and then she actually went back and did almost all of the school to be an osteopath on top of that. Wow. Yep. Wow. Yeah. Which is super interesting cuz those, even those two thought patterns are almost.
Bipolar of each other, yeah.
[00:30:30] Jodie Nelson: And the recommendation came from a friend that Mike knew way back in ZHealth days. Yeah. And he had I don’t know, was it from a fight or was it from his just lots of stuff. Structure was, his chin was totally to the one side of his face.
Lots
[00:30:47] Dr Mike T Nelson: Of that’s a cranial kind of torsion you can see. Yep. Yeah. But he
[00:30:51] Jodie Nelson: is, he’s been working with her for years and since his kids to see her as well. So she, I was just amazed by what she did, taking pictures of my whole structure, taking a picture saying, oh, you have this shoulder goes down and your head tilts this way, and checking all my cranial sutures, which I’m like, no dentist has ever touched my head, checked if my shoulders were tight, I’m like, this is a whole nother level of checking in the body then.
Hey, let’s just slap some braces on you. So that was a very interesting
[00:31:27] Dr Mike T Nelson: experience too.
[00:31:28] Zac Cupples: That’s very cool. And I think that’s, goes to show the power of this stuff when it’s done well. But also how you have to look at a lot of a lot of areas that could potentially be impacted by changing the structure of the mouth.
So the fact that your dentist is looking at airway as well as your movement and, cranial function. That’s huge. That’s huge.
[00:31:53] Dr Mike T Nelson: Yeah. I’ve even seen on a few online clients, obviously we’ve worked together on those. I’ve consulted with you on that with Sam and some other ones. Even on stuff I’ve worked with Dr.
Tommy Wood on for just generally just blood work stuff, like I’ve noticed more and more, and again, maybe it’s just because you’re only looking for what you’re quote unquote educated in. , like lots of weird stuff for hematic Red would be like super high. Like we had one client just ridiculously high hematic red.
Her aerobic performance was good, but not amazing. And we looked at it and Tommy agreed also that she probably has some obstructive sleep apnea that she’s becoming so hypoxic at night, right? Her body’s going, oh my gosh, hypoxia, let’s, crank up the epo. We need more blood volume to try to, fix this.
And she’s had, some sleep issues and different things like that. So she’s in the process of getting a formal sleep study and going through a physician to see what’s going on with that. But even then it’s the general physician she was seeing is oh, don’t worry about it.
You’re fine. And I emailed Tommy and I’m like, dude, I don’t know exactly what I’m looking at, but this makes no sense to me whatsoever. I’m like, there, I’m pretty sure there’s something going on and. He looked at it and he’s is she a cyclist doing epo o ? I’m like, no. Cause her medic grid’s like sky high.
So yeah, you can see weird stuff like that.
[00:33:20] Zac Cupples: Did you notice anything with like glucose measures at all on the camera? They were border,
[00:33:24] Dr Mike T Nelson: if I remember it. They were borderline high. They weren’t like diabetic and very active person drawing, very active, very high performer, high level job, but it’s, yeah, it’s just fascinating how some of those underlying things in terms of stress, HR V is, eh.
Okay. Not amazing. It’s always hard to tell cause everyone’s a little bit different too. So I’m excited for her once she gets a sleep study just to see, what’s going on and what can be done with that. Cuz I have a feeling, same thing, she’s reporting and being more tired in the afternoon.
And again, that can be related to a whole host of things too, but, Yeah. So even again, going back to the whole comprehensive thing of just looking at all the different markers and trying to think holistically of, what could possibly be going on. Okay, if we think it’s this, okay, then obviously talk to your doc about getting a sleep study.
If it is, then you know what to do. If it’s not, then you can rule it out and go down to the next thing. Yeah, for
[00:34:22] Zac Cupples: sure. And one thing when you’re getting the sleep day, cuz I’ve run into this when I recommend it with some people or if they go through their physician, is a lot of times they will only be looking for sleep apnea, only score the the ahi, which is the Apnea Hypopnea index, which basically the, such a bizarre system. But if you have a period of 10 seconds or more where you’re not breathing, that’s considered one APNIC event. And if you have over five of those per hour, that’s when you get a diagnosis of sleep apnea.
And then the degree of that is based on severity. . But now the issue is what if you have several that are five seconds Yeah. , or you just desaturate for a moment. Your brain still thinks, I’m not getting enough oxygen. I need to wake up. . And a lot of times that isn’t measured on conventional sleep safe.
And that’s where the R d i, which is the respiratory distress index, is so important because it catches those . And so someone might not have a lot of APNIC events and they might not have sleep apnea, but they could have upper airway resistance syndrome, which is basically a reduction of blood fl or upper reduction of oxygen.
But not to the degree of apnea. And if you compare U A R s, upper airway resistance syndrome to mild sleep apnea, the symptoms are actually worse in that compared to sleep apnea. But you can’t catch that. We had this issue with one of my colleagues his wife, Almost said one of his wife, he’s only got one
But she got this one sleep study and her AHI was only three, but she’s got horrendous sleep waking up, very frequently throughout the night. And she’s a fit young woman, which is one of the risk factors for having upper airway resistance syndrome. So they did not score the RDI on her.
So we had to get another one to make that a case. And then the other issue too is you can also have some people who have perfect sleep studies, but there could still be something wrong. And if there’s a cool video on Dr. Ziggy’s website where he had this kid who was just, couldn’t sleep major issues, sleep studies were totally fine.
They ended up doing a dice procedure on him, which basically what that is, is they put you under and they look at your airway to see if there is a physical collapse. While you’re sleeping. And this kid, gosh, this video’s crazy, but he was just like violently moving. His legs were kicking up in the air.
So even then if your sleep study’s clean, you could still potentially have an issue. And that’s where something like a DICE procedure can confirm if there is a legitimate airway obstruction. So it’s again, even like a sleep study isn’t exact science in that regard, or doesn’t catch everyone.
[00:37:19] Dr Mike T Nelson: Yeah. Wouldn’t they get that on a, I guess I’m thinking of the at-home ones where they use an accelerometer monitored thing. Would that show up on that and it’s, the data may be there that they’re just not used to looking at it then? Or how does that work?
[00:37:33] Zac Cupples: That I’m not sure. That, I’m not sure. Yeah, I know Zaggy uses the watch Pat one, which is the one.
With most people because that one’s gonna get your AHI and your rdi. I it’ll get both. It does. Which is why it’s great. Whereas I don’t know if it would pick up something
[00:37:48] Dr Mike T Nelson: like that. Got it. Yeah. And so for people listening, the watch pad is something that they can recommend or they can ask their physician to get a prescription for and it’s done at home.
Cause I know one of the restrictions I have with a lot of clients is when they go to their doctor and they ask about it, it’s like to get a, a poly full psg, polys, sonography sleep study, it’s expensive. You have to go into the hospital, you have to spend an overnight there.
Sometimes insurance covers it, sometimes it doesn’t. But I think using something like the watch pad where you can do it at home and then have a physician read it, makes it a lot more doable than it has been in the.
[00:38:25] Zac Cupples: Absolutely. And the really nice thing is now with the wonders of the internet, you don’t even need to go to your doctor to get it done.
You
[00:38:32] Dr Mike T Nelson: have someone else read it. .
[00:38:34] Zac Cupples: Yeah. I literally, I, gosh, I should have bought stock in ’em, but there’s a company out of Reno called I Sleep that I send all of my people to get their sleep study through. And it’s only like with the discount code, it’s 225 bucks. But I’ve even seen the watch Padd on Amazon now.
I
[00:38:50] Dr Mike T Nelson: saw that too. I was confused. I was like, what? And it wasn’t that expensive, if I remember right. No,
[00:38:55] Zac Cupples: no. Compared to a couple thousand when you’ll get, you’re gonna be sleeping in your own bed. Yep. And you can get most of the stuff that you would need to make decisions. And I also think too, just Mike you do an intervention with someone and maybe you’re using Aura Ring or anything to test, retest to see what works.
. That’s a super easy test, retest. So you, yeah. You get your watch pat, you do some intervention and then you get another one just to see where it’s at. To me, I think it’s a no-brainer for most people just because the barrier is low to at least get a baseline. And in your case, did
[00:39:33] Dr Mike T Nelson: Difference in H R V or Aura or in addition to your symptoms of not being entired in the afternoon?
Did you see any change on any of those metrics? I’m more just curious.
[00:39:44] Zac Cupples: So the one thing that’s improved since I’ve gotten this done, because really like my HR V and all, that’s been fairly good, but I have had an increase in REM sleep. Not a lot cuz I still am 20% or more on both REM and deep.
Okay. So it’s, that’s pretty good.
[00:40:04] Dr Mike T Nelson: I
[00:40:04] Jodie Nelson: have a weird question on that. So I’m noticing something strange, and I don’t know if this is, has to do with any of this at all. , but my dreams are more real in the sense that I can read in my dreams. I can feel things in my dreams that I’ve never felt before. And one of the people that I’m working with, she said, you may be getting more REM sleep, which means you may be dumping, your brain is doing a better job of it, dumping things out, but it’s a lot more concise.
Real vivid, very vivid. Did you notice any of
[00:40:44] Zac Cupples: that? It’s funny you mentioned that, cuz Yeah. I was someone who rarely dreamed or at least rarely remembered my dreams. And I’m not consistent yet, but the, I do remember my dreams a lot more and I feel like I’m dreaming more than I was, which is really cool.
I remember there’s a week where I dreamed or dreamt almost every night. And I can’t remember, it’s. Probably been over a decade since that’s been case. So yeah, I think it makes sense to me. If, you improve positioning needed to breathe through your nose it would make sense that you would probably have better rem and subsequent dream memory.
And that was, when you look at my sleep study, that was where I had most of the APNIC events and the respiratory distress was during rem. Interesting. At yeah, my deep sleep’s great, huh. But REM is just not good.
[00:41:38] Dr Mike T Nelson: Yeah. Cause I often wondering about that on, I have one client in particular, I’m thinking about who, I’m probably watched this and send me an email about it, but and again, it’s off of Aura and you never know, is it just that person and has a hard time differentiating between REM and non rem.
Because it’s, again, it’s. $300 device is not a hundred percent sleep stage differentiation based on what they’ve published, maybe 70%. So it’s good, but you also know that if you extrapolate over enough people, you’re gonna have abnormalities that it’s just gonna have a harder time dealing with too.
So I always look at those with a little bit of grain of salt, and then I try to use it more as a comparison on that person. Not take the absolute numbers, but say, okay, is this person getting better on rem? Are they getting better on deep sleep? Not looking at it going, oh my God, it says you only get 40 minutes of REM sleep.
Oh, how horrible are you? Bad human being it’s if it says 45 and then you consistently getting an hour and 20 minutes, you know that’s probably a real difference. And then you can look to see how do you feel? Do you have more vivid dreams? Do you recall stuff better? Do you feel less tired during the day?
And try to correlate it that way because I think. There is, I’ve gotten, I don’t know how many emails from people who are like, oh, my r v is so horrible on, on Aura, I’m, ah, I don’t know what’s going on. And it could be a whole bunch of things. And I’ve got another client who, his athlete HR V is pretty good, but his Aura, H R V for whatever reason, is just super low and everything else is pretty good.
Performance is good, everything else is fine. So I’m like, eh, probably don’t worry about it that much. We’ll keep, trying and playing around with some other stuff to see if it, it comes up. But who knows? Maybe you’re just one of those weird anomalies too, so I don’t like people to take data and completely freak out and be convinced that there’s something that’s wrong with them now, even though they felt fine before too.
[00:43:34] Zac Cupples: Yeah. That’s one issue with measuring all of this stuff is
[00:43:37] Dr Mike T Nelson: yeah. And as you measure enough stuff, you’re gonna see something that’s outta line. You do enough blood tests, you do enough tests of anything. Just by the law of statistics, something is gonna be off. That’s just the way it goes.
[00:43:50] Zac Cupples: Yeah. And that’s, in my realm, in physical therapy, we see that a lot with just imaging of the body. Oh yeah,
[00:43:56] Dr Mike T Nelson: definitely. When you measure
[00:43:59] Zac Cupples: back imaging anything, yeah, back imaging when, depending on what research study you read and what age group you’re in, 30 to 80% of asymptomatic individuals can have an abnormal finding.
And that’s not even considering. There’s this really cool study, I forget how many radiologists they
[00:44:15] Dr Mike T Nelson: had reading. Listen, sent them all the asymptomatic people. , yeah. And it
[00:44:20] Zac Cupples: was like, I think it was like 10 different radiologists. I remember. Seven. Yeah, it was a few and it was like 35 different diagnoses.
Yeah. For one mri. So with. When you’re measuring anything, it’s not exact science. You have to take that into consideration. But then also, like you said, Mike, what are the symptoms or the outputs that this person’s feeling? And then you try to meld a story together, putting all these things together and then trying to, use your clinical experience and judgment to make whatever seems to be the best decision for that person.
Realizing that it’s, we call it practice for a reason. And sometimes this stuff, you might think you made the best move and it might not be for that person.
[00:45:05] Dr Mike T Nelson: Yeah. And that’s what’s hard too, because like different things will have different outcomes and different people, right? So you can’t say, oh, maybe you have a super narrow palate.
If you have this done, then your H R V and sleep and everything’s gonna be amazing. Me maybe not. Like in, in Jodi’s case too, like we did some stuff Some more hands-on work for, the trauma you had in surrounding, drowning and that kind of stuff. And that was done at the same time as you’re doing a lot of the myofascial stuff too. So it’s hard to say which one of those things had an outcome that made it better. But at the end of the day, I don’t really care all that much because it’s better. , yeah. If I was trying to design a perfect study, then of course you wanna try to figure out, okay, we’ve got the one intervention, we’ve got the placebo control.
Doing a sham over here, and your whole goal is to figure out what is the mechanism. But as a, an individual level or even like in your practice, I would imagine your outcome is more, okay, how do I make this person better? I wanna understand a little bit about it, of course. But the end result is, are they better or not?
Even if that means, I’m gonna give up knowing exactly why they are better doing it too. . Yeah.
[00:46:14] Zac Cupples: Yeah. Your sleep deprivation doesn’t care if the evidence
[00:46:17] Dr Mike T Nelson: no.
[00:46:19] Zac Cupples: to do this. You want symptoms to improve. Yeah. And I agree with you a hundred percent on that. It’s just, the issue is you’re playing with probabilities that you don’t necessarily have the exact percentage success rate for a particular intervention.
And so that’s what’s tough. But it’s also I think, part of dealing with the difference among individuals. , Jodi, you and I could have the very similar sleep studies and similar impairments, but we could need completely different interventions to get to where we want to go. And then where we want to go is even different.
Like your goalposts might be different than mine. Yeah. And that’s what makes working with people challenging. .
[00:47:02] Jodie Nelson: And it’s also, yeah. And it’s also challenging even working with trying to diagnose, so when we had all the imaging done for my airway, they told me I had a voluptuous uvula that was blocking part of my hair,
They didn’t say that, but that’s
[00:47:19] Zac Cupples: how I’m gonna use that as a pickup line. Roll up
[00:47:21] Jodie Nelson: to us uvula. Yeah. I had inflamed turbinates and what was the other thing? There was one more
[00:47:27] Dr Mike T Nelson: thing. I think that was it, wasn’t it? There’s one more thing. Okay. I’ll think of it.
[00:47:31] Jodie Nelson: But the dental person that I’m working with sent me to see the ear, nose, and throat specialist that she usually refers people to go get checked.
And he is ah, nah, you’re fine. There’s nothing right here. Go get some Flonase. And no, you’re not bad enough to need surgery. So that’s okay. I don’t want something really truly invasive, but part of it is that I’m not, don’t have any severe enough symptoms in their eyes, or I’m not reporting it as dramatically as I need to get the response that I want or that I need, which I don’t know if that’s what I need.
So that’s the interesting part too, even with when you’re getting diagnosed by the people you’re trying to trust to do this process, it’s very interesting and that’s what makes it also hard. I think for anybody who is the lay person. I would’ve never been down this road and I decided to just go get my teeth yanked and put back in.
So yeah, it’s just, it’s an amazing, weird. Trying to decide what’s better and best as far as interventions. Especially if I’m, they’re gonna be taking something in or out of my throat that will take a while to get better from.
[00:48:52] Zac Cupples: Yeah. Did they measure your throat dimensions in terms of the airway size there?
[00:48:57] Dr Mike T Nelson: I believe we have that on the I don’t remember what they were though. I don’t
[00:49:00] Jodie Nelson: remember. We’ve got the scans that show that, show it all, and it does show that the airway is a little bit restricted by what’s in my throat structurally. So we do have it, I just don’t know off the top of my head what, like the measurements or whatever it
[00:49:18] Zac Cupples: was.
Yeah. Because I think, the issue with turbinate inflammation is that can happen for a variety
[00:49:25] Dr Mike T Nelson: of reasons. Of reasons, yeah.
[00:49:26] Zac Cupples: , so then, and it, this probably goes a little bit out of my scope. . But it I, my thought would be, if I had to do all this all over again, especially considering the relationship of the palate and the oral the throw posture in terms of airway dimensions, I might have gone that route first.
Instead of going nose first and then everything else. Because if you image me right now, I still have turbid inflammation. And I’ve tried Dr. Zaggy, I remember I, when I saw Dr. Hawk for the consult, he just texted Dr. Zaggy and said, Hey, because I still had some crap in my sinuses, and the turbines were inflamed.
What do you think of this? Does he need to see you? He said, ah, just give him some drugs, . And, but these, it was insane. because I, it was a budesonide where basically you put that, it’s just a corticosteroid. You put that in water and you shoot it up your nose. And instantaneously my nasal breathing was significantly quieter.
My, my partner at the time, she was like, I don’t even hear you. And she would always say, Zach, you’re breathing so loud through, we’re sleeping. So it’s, yeah, it was crazy how fast that worked. But again, I had the surgery, so why is it that my terminus were still getting inflamed? And I wonder if the roof of the mouth has such a, such larger real estate on nasal breathing, if that’s not the best area to address first.
But then again, if you have a restriction in the throat or the cervical spine, that’s limiting the dimensions there. Do we need to do something there to improve those dimensions and then that makes everything easier. And that’s where, I don’t know, but my suspicion would be that’s probably the first place you’d wanna look.
Yeah. Because what they don’t talk about with like septal deviations or things like that is a lot of times these go back. And the
[00:51:27] Dr Mike T Nelson: question is why, so there must be some type of local pressure or some type of stress that’s then maybe driving it that direction Could be, yeah.
[00:51:39] Zac Cupples: There’s some research showing septal deviations with people who have scoliosis, who have connected those two things.
Yeah. So are there some movement influences that are potentially driving that? Sure. That there could be movement influences that are driving the dynamics of the cranium. And the pallet as well. And that’s just where there’s a lot of uncertainty, but, in, in my mind, I think addressing the oral posture is probably something I would do sooner rather than later.
Just because of the amount of real estate that it affects from a nasal breathing standpoint. I’d be curious, what did what did Dr. Nester say in that regard in terms of addressing specific areas? Did he have any thoughts? Cause I know he’s messed with a few different things in his book. Yeah,
[00:52:29] Dr Mike T Nelson: The only thing he talked about was what he had done where he added more actual bone mass to his, and I’m trying to remember what was the device he had?
Wheel block. Yes. That’s what it was. Yeah. And so he actually had CT scans before and after showing that he actually added, was it three pennies worth I think of more bone mass than he had before, and said his nasal breathing and everything else got significantly better. . So that’s the only thing I remember from that per se.
But yeah, it’s super, super interesting, right? Because most people looking from the outside would say, if you’re older, there’s no way you’re gonna add more bone mass to your skull. What are you talking about? That’s crazy. But it’s just fascinating to me how if you apply the right stressors, your body is always gonna adapt, right?
You look at the studies of people who are in their eighties and nineties, they start strength training, they get stronger, right? They get stronger at the same rate as someone who’s younger. Granted, they’re not gonna add as much muscle mass cuz they may be just, bicep curling, a soup can’t, right?
So they’re not lifting as much load, but in terms of percentage of progress, they can still make significant progress over their baseline. So I’m always just fascinated by that. Your body almost never loses the ability to adapt. So I worked in medical devices for 12 years. We had devices to treat congestive heart failure.
So we’d have these people that were emitted, like these huge, like basketball sized hearts, right? Instead of the blood getting pushed out, it’s just moving back and forth in this kind of like hula hoop type thing. So we put a little wire down on the left side of the ventricle, a little wire down on the right side of the ventricle, and then they would time the impulses.
So now the heart’s actually working better. It’s ejecting blood ejection fraction acutely goes up, 10, 15, 20%. One of the very early cases a guy was, , literally sleeping with three pillows a night cuz he had so much fluid backing up in his lungs. And 3, 4, 5 months later, something like that, he like rode his bike across the state, and granted he was a very hyper responder to the procedure.
And all the cardiologists and electrophysiologists were just fascinated because the heart actually remodeled in a lot of cases smaller again. Because now you change the stress completely, you make it more efficient and the dynamics of that change, and these are people who were really like bad off like probably a couple months from dying in a lot of cases.
And even then, with the right stimulus, which are the 24 7 stimulus, the body’s able to re remodel back to something that’s better. So that to me is always fascinating if you’re talking about facial structures, even if you’re older, having an appliance, having something in there that’s literally applying a small amount of pressure can start to reshape everything again.
[00:55:20] Zac Cupples: Yeah. Yeah. I mean it, yeah. The adaptability of the human body is quite amazing in regards to the bone growth and bone development that even, especially in the mouth, is still a bit controversial in the dental field. It’s funny cuz so much of this is political in many respects. , yeah, just like in physical therapy, but you just have all these camps that are selling their particular appliances Oh, sure.
Certain claims. And to my understanding the bone that you can change is most likely alvear in nature, which is what basically moves when you get braces and things like that. You have to be mindful of people who claim that the palatal bone can change with an appliance because that might not necessarily be the case.
Interesting. And yeah, and not only that, sometimes they’ll claim that while I’m moving, the teeth to a very far range, but basically all they’re doing is they’re pushing the teeth as far as they can out in the velar bone. And then, they potentially have some damage to the roots and then problems ensue.
So you really have to have regardless of the mechanisms, you have to have someone who’s a skilled practitioner who’s taking into consideration all of these factors. So it’s, yeah, it’s just something that is, it’s interesting to see how there’s similar battles in all fields in terms of what mechanisms are going on and what’s also most effective.
[00:56:53] Dr Mike T Nelson: Yeah, and it’s like anything else too, like how much you can change is probably debatable, but if you can change it , then your next question is what direction and how much. So that comes into the, the skill of the clinician or doctor, physician, whoever you’re working with, to say, okay, in my experience, I think we need to go this direction where someone else could say, no, I think you need to go in that direction.
And that’s where it gets, I think, especially for someone from the outside looking in, extremely confusing, , . And now you’ve got, you’re talking about a crossover of realms of, physical therapy to myofunctional, osteopathic dental. You have all these areas that are overlapping each other, and that gets even more confusing because everyone kind of has their own progression and they have stuff that they’ve seen and things that, that work too.
So it, it gets to be hard. It
also
[00:57:44] Jodie Nelson: is hard for the person. . Cuz I think self-awareness is such an interesting thing to try to have when we all have stuff that’s messed up, right? Even in, just in talking about this, one of the things that I could complain about for much of my life is fear being the overwhelming.
Not that I thought I, I was always a cheerful and hopeful and optimistic person, and yet the, an overriding emotion that constantly came up is fear. Why? Multiple reasons. Including having a trauma. So that’s the hard part when as people are sorting through this, which direction do you go first?
I don’t know which is the biggest screaming thing, because that’s one thing that’s interesting is watching as I’m doing different things, getting my gut health back, doing all of this stuff in my teeth and my mouth and the cranial stuff. just watching how much more cheerful I am as a person and watching the level of that emotion that I didn’t understand why I was there going down or at least muting a little bit.
So that’s the hard part too, is what is the person going to do? And also how is there self-awareness to know? If you’re scared all the time, are you gonna make the best decisions? Probably not. Yeah. So how does that affect, it’s just a big ball of trying to figure it
[00:59:12] Zac Cupples: all out, . Sure. And you’re lucky in your case, Jodi, because you have a clinician who’s looking at a lot of different areas under one, one set of eyes or, at least under one model. Whereas think about if you have. Your dentist, and then you have your osteopath, and then you have your malfunctional therapist, and they’re all looking at it from their lenses, but they don’t have anything that unifies them from their approach. You think about the fear that’s going on in that regard because this person’s saying this and this person’s saying that.
And it really just it says it takes a village to raise a human. I think it, it takes a team to really get people to be optimized, and if the team isn’t talking together, then that’s, it’s hard to get that. And I think that’s probably the overarching theme with all of this is hard to find a bunch of people who can work together to help that person.
Get to where they need to go. My, my friend Joe is very lucky in that regard because Dr. Hawk teams up with Dr. Zaggy, who’s the E N t, who then they both team up. They have an oral surgeon Dr. Mova had, and then Joe and several MALFUNCTIONAL therapists who all are looking at this from.
One with one goal in mind, and that’s, how can I make this person’s airway as good as possible? It’s hard to find that, in one place, let alone every state in the us
[01:00:36] Dr Mike T Nelson: Yeah. Yeah. Because if you’re one of the professionals in that group, right? And someone like I come in and go, yeah, I need you to help with this and I’m gonna work with this cranial person.
I’m gonna work with this myotherapy person, and they don’t know any of the people I’m working with. They understandably get fearful. It’s whoa, what are you doing? You’re gonna muck up my results and you’re now, you’re doing this and that. And I think it takes a very special kind of open-minded person to figure out, okay, what exactly are you doing?
What’s going on? And then they have to be a little bit educated enough to know what you’re talking about in that area. And so finding a group that is all coordinated with each other and each know what they’re doing. and knowing how that’s gonna help the person in the end I think is super helpful.
Also, unfortunately, very rare. .
[01:01:22] Zac Cupples: Yeah. Yeah. And that’s the group that I’m referring to, one lives in San Francisco, one lives in la and the other lives in St. Louis. . Yeah. It’s been, in that case, you’re still picking people from just across the US and unfortunately for most people, that’s probably not feasible to, to go and fly to all these places, especially, when there’s a pandemic going on.
Yeah. And you want to minimize travel.
[01:01:47] Dr Mike T Nelson: Yeah. So as we wrap up, if someone’s listening to this and they’re like, cause in most of the time this podcast is about different aspects of, performance and body comp and trying to increase your health at the same time. Again, the reason we wanted to have you on is just to not necessarily dictate where people go, but just give them some other ideas when they get yeah, I’ve reached a plot too. Everything else seems to be pretty good. Oh, maybe I should talk to my physician or look at eye sleep to try to get, some type of sleep study. Maybe I should, get at least an evaluation from, a dentist or orthodontist or professional in that regards.
Maybe they’ll recommend some, imaging of the airway, things of that nature. Where would you recommend people, if they want to go down this sort of path what steps would you recommend? Like where should they start?
[01:02:37] Zac Cupples: I think the first thing is a no-brainer.
[01:02:39] Dr Mike T Nelson: And get a sleep study. Yeah. That’d be my thought too.
[01:02:42] Zac Cupples: Yeah. Because once you have that data, it allows you to have conversations that you might not otherwise be able to have. . Yeah. And that’s really where you gotta go. And then once you have that, I think the first place I would go is likely. finding someone who can get you some type of airway imaging.
If you can find a dentist who is someone who promotes more expansion based stuff. So if you talk to your dentist and they say, yeah, I think pulling teeth is okay. I use retractive orthodontics, which is basically where they pull the teeth back into place to, to make the smile look good and fit.
Or they don’t recognize that there’s other sleep disorders besides sleep apnea. That’s probably not the person you want to go with. You wanna find someone who appreciates the airway, uses things to, or appreciates oral posture and malfunctional therapy. Maybe that’s one of their referral sources.
Uses things to expand the mouth structure collaborates with multiple practitioners. That’s the type of person I think you really want to try to seek out. . Unfortunately, that’s where you gotta do a little bit of research on your own to see if you can find that person and realize that many times that’s not, you might have to go out of state to make that the case.
But we spend a third of our lives sleeping and it’s I think it would be who view, especially if you have the capabilities to do something, to get that taken care of. Even if the best you can do is get a CPA or an oral appliance that’s still better
[01:04:20] Dr Mike T Nelson: than nothing. And was the referral one, one I sleep, was that one of ’em?
You said that if people are looking for a referral source?
[01:04:29] Zac Cupples: Yes. I sleep hst.com. I
[01:04:32] Dr Mike T Nelson: sleep hsc.com. H
[01:04:35] Zac Cupples: H as in Harold, S as in Steven, T as in Tom. Tom. Okay. Yep. And if oops. Hopefully they’re cool with, this’ll go . Just that. If you type in HST 10, you’ll get a 10% discount code. And that’s been least expensive that I’ve found for the watch Pat one.
And the other thing I would say, if you end up getting a sleep study through them, make sure you get the watch pat one. Okay. Cause they have another one on there. One of my colleagues got the other one. Yeah cuz you have the Yeah, the watch pat one disposables the one you want. The other one does not measure the rdi.
Oh. And
[01:05:10] Dr Mike T Nelson: that’s interesting.
[01:05:10] Zac Cupples: Yeah. So that was the problem that we ran into. . So get the watch pat one, it’s a little bit extra, but it’s gonna give you way more data. So you want to, you wanna get that one and they’re pretty good. But also too, if you’re like, ah, I wanna just get it on Amazon, you can get ’em there as well.
[01:05:28] Dr Mike T Nelson: Cool. And I know you’re doing work online now and what kind of work and services do you provide and how do people get ahold of you? .
[01:05:35] Zac Cupples: Oh, yes. The place to find me is zach couples.com. It’s Z a c u p l e S. I do a lot of different things remotely. I do movement consultations cause I’m a physical therapist, so doing things to improve your movement capabilities.
If you’re someone, maybe you have some neck restrictions and that could potentially impact your airway dynamics. Or you have difficulty getting your tongue into an appropriate posture to breathe through your nose. I can help you with that remotely. I also offer online training as well where we, where I basically design fitness programs that help you get your fitness goals while also respecting your movement capabilities and improving movement simultaneously.
Because in, in my eyes, what I try to do is I try to get people a, the largest movement baseline that they can possibly get, so then they can go and do whatever they want. So if you have hip restrictions, that’s gonna limit all the tasks that you can do. , I’ll try to do everything I can to improve upon that.
And then the other thing that I offer online is mentoring. So if you’re, a coach or a clinician and you want to do some of the things that I do, whether it’s airway or improving someone’s movement capabilities, because I think that goes hand in hand with airway, I can help you with that.
And also too, if you’re someone who is thinking about going down this pathway and you’re unsure where to start, you can always go ahead and reach out and I can help guide you to see if there’s someone in your area.
[01:06:58] Dr Mike T Nelson: Yeah. And my advice, if people are listening, even just paying you to do a consult, to help guide them in the direction or to limit, okay, this might be a good idea, that might not be a good idea, start here if this, then that.
To try to help them map it out a little bit. Because it’s the old thing, when you get into new areas, it’s like you don’t know what you don’t know. Yeah. And I’m looking to know you. So with some of the stuff I was able to reach out to you and I’m like, , dude, you need to talk to Zach cuz I know enough to be dangerous and I know there’s a whole bunch of shit that I don’t know anything about that he’s gonna be able to at least help us or say, yep, this was good, eh, look for this.
Make sure you get this type of airway imaging, make sure they do this, and this. But for me was like super helpful, so thank you for all your help on
[01:07:44] Zac Cupples: that. Yeah, of course. Yeah. And and that’s the thing too is a lot of times you might work with a practitioner and they’re not gonna get all the things necessary to make good decisions.
Like I’ve, I’ve had some people where they’ve gone to the dentist and they just did the teeth imaging and didn’t do a sleep study. It’s like, how do we know Yeah. If what we’re doing is gonna be effective or not. So you really I’ve made some of the mistakes myself or I’ve had colleagues who’ve made the mistakes.
So I would definitely try to help you get that as streamlined as possible so you can hopefully get the
[01:08:16] Dr Mike T Nelson: best outcome. . Yeah. And I would say if you do find you need some of these procedures, as we’ve talked about they’re really not cheap. And paying your fee to do a consult is in the end is probably gonna save you a ton of money anyway.
Much less the peace of mind to have a little bit better direction to go to. So yeah. .
[01:08:34] Zac Cupples: Yeah. Yeah, for sure. Yeah. If you don’t have to spend $60,000 on a surgery that’s always good. .
[01:08:42] Dr Mike T Nelson: Yeah, . That’s my new thing now cuz I’ve had a couple people that have come to me that I think are a little bit too excited about having the surgery and I ask ’em like, do you really know what happens with that?
They’re like not so much. I’m like, eh. So yeah, I usually send ’em over to you or try to talk them out of it or just get ’em to chill out a little bit before they start having everything rearranged in their face overnight. , .
[01:09:08] Zac Cupples: Yeah. Yeah. Absolutely. I. The surgery is always gonna be definitive, but even the ones that, that we look into, which might be like a one where they advance the maxilla and mandible forward and mma that only accounts for front to back dimensions.
And then, what, if you’re someone who needs a lot more side to side maybe that’s an appliance, maybe that’s a surgical procedure for that. But, if I can help you guide you down that path and hopefully get you in the hands of a skilled practitioner then you’re gonna have better success of finding what’s best for you.
And I think this is one of those cases where the process is still too muddy to do appropriate me search to find out what that is. . Yeah.
[01:09:50] Dr Mike T Nelson: Yeah. I think anything else I probably would argue after anything. Yeah. Yeah. I always do surgery as the last resort. It’s yep, we may get there.
It’s definitely an option. I’m not an expert in that area, but I also know it’s expensive. It’s time consuming and it’s really hard to reverse. Yep. Some of the worst cases I’ve seen of people just working with other physical therapists and people like yourself is people who have had various surgeries of, we’ll say questionable quality
Yeah. And you feel bad for ’em. And that’s not an expertise in my area. But yeah and then I always have ’em, okay, go back, ask your surgeon and if you wait two months, are you gonna make anything worse in that process? Or you’re gonna make it really hard to fix if you do opt to have surgery, whether that’s a knee, hip, face, whatever.
And if they’re like, no, you just may have some pain, you’re not gonna make it any worse. Cool. Okay. Now you know you have a set period of time to try some other stuff and see what affects it. You may end up. Needing the surgery. That may be the only fix and then great. Then that’s the fix. But yeah, I just get nervous if that’s the first and only option.
Yeah. Makes me a little, makes me a little nervous personally.
[01:11:01] Zac Cupples: So unless it’s Catherine Plants and you always gotta go with that one. .
[01:11:05] Dr Mike T Nelson: Yes. Yeah. And that bumps right up to the top of the list. You definitely don’t pass a go on that. You
[01:11:10] Jodie Nelson: guys are silly. I’ve always wanted smaller caps. , what are you talking about?
[01:11:15] Dr Mike T Nelson: Oh, you suck.
[01:11:16] Zac Cupples: Wow. We call that a unicorn. Where I come from. You got the big cabs.
[01:11:20] Dr Mike T Nelson: Yeah. Awesome. Thank you so much. Z couples.com. I also recommend people get on your newsletter. Great stuff. Always some good hip hop recommendations in there too, which I always appreciate finding good new music, which is awesome.
Yeah,
[01:11:35] Zac Cupples: and I’m definitely like backed up on my research in that regard. I need to, I might need to take a day off of work just to catch up on hip hop, but Yeah. I, yeah I’m glad that you are. I always enjoy the the occasional response of sending me some metal that I haven’t been exposed.
Oh, yeah. Yeah.
[01:11:49] Dr Mike T Nelson: Good exchange there.
[01:11:51] Zac Cupples: Yeah. Yeah. And the hip hop you sent me the other day was yeah, RT j’s
[01:11:55] Dr Mike T Nelson: very good. Oh, yeah. I’ve been getting to run the jewels lately. I don’t know why. Everyone has been in them forever. And just like one of those bands where it’s yeah, I liked them before and then I forgot like how good their stuff actually is.
It’s oh. And then lately I’ve been kiteboarding a lot, so I’ve been listening to ESOP Rock a lot. Oh, nice. Every time before I go kiteboarding, I listen to him. So it’s my neuro anchoring when I don’t feel like I’m in a good mood. I listen to that and it makes me feel good again, , that works. Yeah.
[01:12:21] Zac Cupples: And anything in 2020 to make yourself feel good’s good? Absolutely. Definitely. Yeah. If there’s one thing that has been good in 2020, it’s been the music and the memes.
[01:12:29] Dr Mike T Nelson: Those are, that is true. Yeah. That is a plus, especially with all the artists, you can, to me it’s a stress test of even artists, right?
You can see who is like a legit artist and found a way to, to produce music or do something creative versus a lot of the other artists who just disappeared, and I get that, money is tight and it’s a really hard time for a lot of artists, but you can see the people who, as part of their dna, they just, they have to put something out regardless of record companies or money or anything else.
And so for me, that’s been super fascinating to watch in a kind of weird way. . Yep. I hear you. Awesome. Thank you so much. Really appreciate you coming on the podcast today. Thanks again. Thank you for having me. It’s been fun. Thank you so much for listening to the podcast today with my buddy Zach. Big thanks to my wife, Jodi, for being on and sharing some of her experience that she’s going through right now.
Again, I would highly recommend if you have questions in that particular area. Please reach out to Zach. Tell him I said hi. He does a great work. It’s been an honor for me to consult with him with different clients. If you are a trainer, having people in your referral network for areas that are outside of your expertise is extremely helpful.
One, because you don’t have to be an expert in all areas, which you’re never going to be. The biggest key is knowing who to send them to get good and accurate information. And in the land of physical therapy and especially this area, Zack is definitely at the top of my list and he’s got great stuff via his newsletter too, which I would recommend that you check out.
So thanks again for listening to this show. Thanks again to Zach for all of his time and sharing so freely of his knowledge. Thanks to my wife Jodi, for sharing her experience also. And be sure to sign up to the Flex Diet certification. The next round will be probably, it looks like around January right now, 2021, depending on Monday.
You’re listening to this. Go to flexdiet.com. You can get on to the newsletter there. That is the main newsletter. Depending upon when you are listening to this, if you’re listening to it right as it comes out, you will notice via the newsletter, I have another certification coming out on the physiologic flexibility.
So how do you incorporate all these kind of new and potentially sexy recovery metrics and methods such as breathing methods, cold water immersion, heat interval training, cardiovascular? Glucose in terms of should you avoid large influxes of glucose as carbohydrates or how does your body handle them?
What about differences between nasal and mouth breathing? We cover all of that, and again, a complete physiologic system to make you a more robust human being, be able to handle more stressors and recover faster. So for now, you can just get on the newsletter that’ll have all the information for both.
Go to flexdiet.com. You’ll see a little button there that says Join the wait list. That will put you onto the newsletter and you’ll get all of the updates for free. So thanks again, greatly appreciate it. Any comments at all, please let me know. And you can just send an email to questions flexdiet.com or as always, leave information in them, reviews in iTunes or whatever your favorite.
Podcast player is, we greatly appreciate it. It does help drive the show, and I want to deliver things that are useful to you. Thank you very much. Talk to you again soon.





Leave A Comment