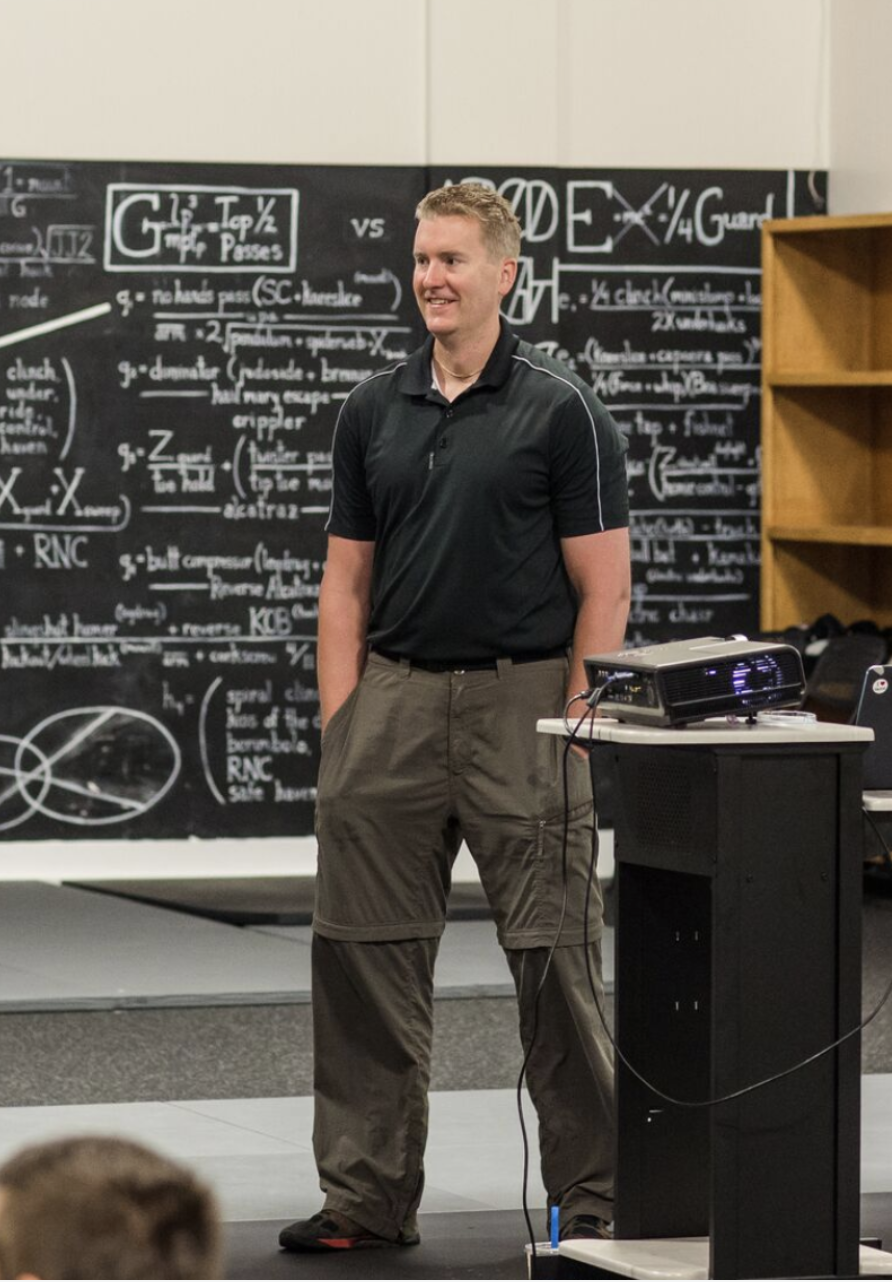
This episode of the Flex Diet Podcast is a rebroadcast of a live interview with Dr. Tommy Wood from 2020. Coming to you from the jungle of Costa Rica, Dr. Wood and I discuss insulin and its role in the body while sorting fact from fiction.
Listen in to hear:
-
[6:21] Dr Wood’s carnivore diet experiment
- [9:38] The commonly accepted theory of glucose and insulin
- [12:02] Insulin and the liver
- [15:28] Blood sugar
- [18:43] Healthy fat tissue as a metabolic buffer
- [20:56] Fasted cardio, carbs, and the insulin switch
- [29:01} Helpful blood tests
Find Dr. Wood
About Dr. Wood
Dr. Tommy Wood is a UK-trained MD with a PhD in physiology and neuroscience. He received an undergraduate degree in biochemistry from the University of Cambridge before attending medical school at the University of Oxford.
After working as a junior doctor in central London, he moved to Norway for his PhD work and then to the University of Washington as a postdoc, where he’s now an Assistant Professor of Pediatrics.
Tommy’s work and research interests include the physiological and metabolic responses to brain injury and how that impacts brain health across the lifespan, as well as developing easily-accessible methods with which to track health, performance, and longevity in both elite athletes and the general population.
Rock on!

Dr. Mike T Nelson
Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
Hey, what’s going on it is Dr Mike T Nelson back with the Flex Diet Podcast. And the wonderful wife and I are still in south Padre, Texas as of this recording, but we will be headed back home very soon. And I wanted to get a podcast out to you. Got a bunch more guests coming up in December and especially at the start.
[00:00:30] Of the new year. But in the meantime, I’ve got a rebroadcast here I did with my good friend and he is also an M3 one-on-one client training for strong man, which he has been doing awesome. the one and only doctor Dr. Tommy Wood. We were able to see him briefly in Austin, Texas on the way down.
[00:00:55] He was in town then for the Formula 1 race that he does some consulting for. And we happened to be passing through at the same time. So we went out and had some epic barbecue at Black’s barbecue, which it was crazy busy that night, but it was awesome to share a protein-filled meal with him. So in this rebroadcast, this is the intro before the short intro.
[00:01:22] It was recorded live at our good buddy Dr. Ben House’s place at the Flo retreat center in Costa Rica. We talk all about glucose and insulin. The reason I wanted to rebroadcast this. Was, I think this is a super important topic. And there’s a lot of great information out there on the, and there’s a lot of pretty horrible and just flat out wrong information out there also.
[00:01:47] So enjoy this podcast with the one and only Dr. Tommy wood.
[00:01:55] Dr Mike T Nelson: Hey, what’s going on? It’s Dr. Mike T. Nelson here, back on the Flex Diet Podcast. And today I have a very special interview from my buddy, Dr. Tommy Wood. This was actually recorded live from the jungles of Costa Rica when we were down there this past March. So you will hear some jungle noises in the background.
[00:02:22] Hopefully it’s not too annoying. I tried to edit them out as best I could, but we talk all about the glucose, health parameters, insulin resistance, sumo wrestlers, how you want healthy fat stores, and a lot more. Dr. Tommy is a wealth of information here, and if you like more information in a complete system of how to use all of.
[00:02:49] Check out the Flex Diet to go to www.flexdiet.com. Here’s the interview with Dr. Tommy Wood. How’s it going? Good. Good. We’re here in the Costa Rican jungle with dr. Tommy Wood, and you want to give us just a little bit of background on here? I guess we should just say why we’re down here. We’re down here at Dr.
[00:03:10] Ben House’s place at the Bro Research Center in the middle. Costa Rica jungle, and you give a super cool talk. One of ’em is, which we’ll get into here about glucose and insulin, probably not what people are thinking about. What is your background for people who live under a rock?
[00:03:31] Dr Tommy Wood: Probably not under a rock
[00:03:32] I’m not that well known, which I quite like actually . So I currently work as a research assistant professor, so research faculty at the University of Washington. Most of my work is in brain injury. Before then, over several years, I did an undergraduate degree in biochemistry, went to medical school, worked in London as an in internal medicine for a couple of years, moved to Norway for my PhD, which was in physiology and neuroscience.
[00:03:58] And then moved over to Seattle where I am now. So I have two main hats. One being looking at a brain injury, particularly pediatric or neonatal brain injury. And then another one where, Several years. I worked with a lot of athletes as a, I guess a journeyman coach, so as an athlete myself, first as a rower.
[00:04:19] Then I started to do more coaching when I was in med school. Interested in all aspects of performance, so just researching that kind of on my own. And then slowly over time have been integrating that more and more into my sort of active research. So I still work with some athletic groups, some personal clients, and then some sort of larger athletic groups.
[00:04:38] Now there’s a more formal part of my research in addition to all the brain stuff that I do.
[00:04:43] Dr Mike T Nelson: And you are the CSO of Bro Research Center. Is that correct?
[00:04:47] Dr Tommy Wood: Yes. You confirm this? I can confirm this. I confer the of the title of CSO on myself. I. Used it as a Chief snake officer because the first time I came here to the jungle I was bitten by a local venomous snake.
[00:05:01] But Ben has then kindly said that it can also be the chief scientific officer. We’ve just finished analyzing our first study that you helped out with and took part in as well. You were both a scientist and a subject. Oh, that’s fine. And hopefully we’re gonna publish that soon.
[00:05:14] So the first of many things like research projects we’ll work on together.
[00:05:18] Dr Mike T Nelson: Yeah. And that, what I like about it too is that it’s very real world based. Yeah. Everyone’s oh, we want more research and we want it actually in lifters. But there’s, as not a lot of budget for that and different things happen.
[00:05:32] And even just trying to source subjects for this study is lots of people are like, yes, I want to do this. And then you’re like, Hey, here’s your opportunity. Maybe you should volunteer. Oh, I’m busy, bro. I got life. I got stuff going on.
[00:05:47] Dr Tommy Wood: Yeah. Yeah. Most sports science research is done either in sort of sedentary populations as part of like public health efforts, or it’s done in undergrad.
[00:05:57] Students who you can convince to come into the lab, and you have a lot more experience doing that than I do, but it’s not particularly representative of some of the populations that we work with or that. Ben who runs this place works with, which is the, very experienced lifters who can lift a lot of weight.
[00:06:13] How do different factors affect their performance? And that’s hopefully, or, and long term health. And that’s something we can hopefully look at. Yeah.
[00:06:21] Dr Mike T Nelson: Awesome. And before we talk about insulin and glucose, I just have to poke the bear on this one cuz I, I heard a rumor you’re gonna be doing a carnivore diet for a while.
[00:06:31] Dr Tommy Wood: Yeah, I’m gonna, I’m gonna do at least a month, probably six to eight weeks of a carnivore diet, and I’m gonna do it with somebody else in this health arena. I’m not sure whether he wants to be called out on it publicly,
[00:06:42] Dr Mike T Nelson: Yeah, I just texted him today, but we’ll leave him anonymous
[00:06:45] Dr Tommy Wood: for now. We’ll leave him anonymous.
[00:06:46] And part of it is just to get an idea of what it’s like. I’m good friends with Paul Saladino, who is the, he calls himself the Carnivore md. I just fyi, I’m not a big believer in the idea that plants are out to get us or any, or that carbs are bad or anything like that. Broccoli is gonna get you, bro.
[00:07:04] Yeah. Broccoli is gonna trash my thyroid and all this sort of stuff. But it’s an interesting thing. I like being able to try these things out so that I have real world experience in them. I’ve done pretty much every, I’ve done paleo, various low. Low carb, keto and it’s just nice to be able to tinker with those things.
[00:07:21] So yeah, see what it ends up doing. I’m gonna do some, I’m gonna do just for you, mark. I’ll do a 500 meter row before and after to see whether anything happens to my glycolytic abilities. No.
[00:07:33] Dr Mike T Nelson: Two K. I heard the two K was voted down,
[00:07:35] Dr Tommy Wood: man, no way. I will do.
[00:07:36] Dr Mike T Nelson: you used to row competitively, so you know what, like a balls out two K is like Yeah,
[00:07:40] Dr Tommy Wood: and there’s two parts to it.
[00:07:41] One is that I know if I sat down and did a 2 K now I would suck compared to what I’ve done it previously. That’s gonna be really hard for me. But also I know how painful it is. I would much rather do a Cooper run test to than a two K anytime. So maybe I could probably stretch to doing that as well.
[00:07:56] And then we can test my systems and see where the carnivore did anything particularly vegan diets haven’t worked well for me because I tend to undereat so I’m just not hungry and then I find it hard to maintain mass. And I don’t think that’s specifically a vegan diet thing. I’m just not eating enough calories.
[00:08:12] Yeah. And so I’m gonna, I know I’m gonna have to work hard at that on this diet too, but we’ll see what happens.
[00:08:18] Dr Mike T Nelson: Yeah. I, any predictions or do you just wanna hold them until you’re doing the diet and done?
[00:08:24] Dr Tommy Wood: I think I’ll, I think I’ll probably lean out a bit and maybe lose, lose a bit of both, but I, my guess is I’ll probably get leaner, my protein intake will probably go up my, to my total calories will probably come down a bit.
[00:08:35] So my guess is I’ll lean out a bit and I don’t think it will have a huge effect on my performance particularly. Cause I don’t train specifically for performance. So I don’t think much is really gonna happen. And previously when I’ve carbs or something. I’ve, I don’t notice anything I like, I feel.
[00:08:49] Dr Mike T Nelson: Okay. Yeah, that’s my guess. If I were to guess is that you may not see a huge change. It’s pretty cool of you to do that. And I think you started doing some labs before and
[00:08:58] Dr Tommy Wood: after. Yes. I’m planning to at least the basics. If I really wanted to do all the stuff that I wanted to do, I’d be out a couple of grand.
[00:09:04] Yeah. And I’m not, that, I’m not that committed or at least to the testing side. So I’ll do a bit of that and I’ll certainly do blood sugar ketones, although, cause I have all the equipment to do all that stuff. So I’ll do a bit of that as well. Cool.
[00:09:16] Dr Mike T Nelson: Awesome. Speaking of blood ketones and glucoses, you have.
[00:09:20] Gave a great talk down here. That was awesome. Loved it about glucose and insulin. So if you wanna, how do you think your perspective is different from what is commonly taught? I guess we should clear up for the listeners, what is the common accepted theory of insulin and glucose?
[00:09:38] Dr Tommy Wood: So everybody thinks of insulin as the main hormone that regulates glucose, and they think that it does that by.
[00:09:47] Binding to the insulin receptor, which then increases transportation of glute receptors to the surface of the cell for glute four in the skeletal muscle, for instance. And then there’s more transporters more channels for glucose to go through, and more glucose goes into the cell. Insulin directly increasing uptake of glucose into cells and.
[00:10:09] I talked about why I think we think that, and it’s because of the way insulin was discovered. So it was discovered as the hormone that is missing and then required for survival in type one diabetics. So people who can’t make insulin because they lose the beta cells in their pancreas. And this was discovered in the early 1920.
[00:10:30] For some decades before that, people had just been, they knew it was something to do with the pancreas. So they were injecting animal pancreatic extracts into people with diabetes type one diabetes and seeing some benefit improved sugar control. And they’ve mainly tested that by how much glucose is ending up in the urine.
[00:10:46] And so we’ve always thought about insulin being this thing that, you give externally and then it goes around the body and it pushes glucose into cells. And when you use it that. That’s true. However, if you think about how insulin actually acts in a normally functioning body where it’s produced in the pancreas, it has like a series of effects that where and then the final one is that it in high doses, is that it pushes glucose into cells.
[00:11:12] So it’s made in the pancreas. The first thing that it does is it buy, is it active? It inhibits alpha cell production, so insulin made in beta cells, glucagon made in alpha cells, and it reduces or inhibits the release of glucagon, glucagon being one of the hormones that antagonizes insulin or raises blood glucose.
[00:11:33] So it’s one of the hormones that tells the liver to increase glucose production through glucogenesis, stimulate some of the breakdown of tissues to. Push that process forward.
[00:11:43] Dr Mike T Nelson: So basically get fuel from whatever
[00:11:44] Dr Tommy Wood: source is possible, from whatever storage you have. So either glycogen in the liver or.
[00:11:48] Protein in the muscles or fat tissue, cortisol does something, is part of that process as well, potentially. And so the first thing it does is it shuts off glucagon and then it goes to the liver through the portal vein. So there’s a vein that connects the pancreas to the liver.
[00:12:02] It’s where that’s where all your food gets absorbed too. So it goes to the liver. And then the high insulin and low glucagon act on the liver to stop glucogenesis. So to stop the production of glucose by the liver through that process that we were just talking about. So the first thing that insulin does, if you eat and your insulin goes up, the first thing that it does is tells the body to not make any of its own glucose.
[00:12:29] That’s one of the most important things that it does. And then from there, it goes out into the systemic circula. and depending on the dose, and people have done some very cool dose dependent studies, they’ll isolate an arm or a thigh or look at the whole body and they’ll infuse insulin. So they get insulin at a certain level, and then they’ll look at glucose, they’ll look at amino acids, and then they’ll look at fat acids.
[00:12:53] And you see the first thing that insulin does at very low, a very low level, the mid range of what you might get after a standard meal, is it turns off the breakdown or the release of fats from fat tissue. So it inhibits hypothesis, and then at the same time, it’s also inhibiting pro sis, so it’s inhibiting the breakdown and muscle tissue so systemically, I think of insulin as an anti catabolic hormone.
[00:13:17] So the first thing is it’s doing is it’s stopping the natural breakdown of tissues. So your tissues are actually continuously turning over. They are continuously breaking down and being built up, and it’s in this continuous flux. And so when insulin shows up the uptake of, amino acids into cells lipids into fat tissue basically stays about the.
[00:13:38] And then insulin just stops the other half, which is the breakdown. And so if you think about it as like a bathtub model, right? If you wanna fill your bathtub, you can do two things. You can block the water leaving it, or you can open the tap. And most people think that insulin opens the tap, but what it actually does is it puts a plug in the water coming out, and then you get a net accumulation of either amino acids or fat tissue because.
[00:14:04] It
[00:14:05] Dr Mike T Nelson: doesn’t high levels of testosterone, dramatically blunt catabolic effects too is a side note.
[00:14:11] Dr Tommy Wood: Oh, yes. Yeah, it does. So insulin is by no means the only player, right in the system.
[00:14:15] Dr Mike T Nelson: Which may explain why if you go into bodybuilders, why they use exogenous amounts of insulin, testosterones, other drugs.
[00:14:22] Not that we’re recommending that we’re just saying from demonstration of physiologic effects. If you go to the way end of the.
[00:14:29] Dr Tommy Wood: Yeah. And so there are, as you then increase insulin levels beyond that, you do start to stimulate. Glucose metabolism. So the oxidation of glucose for energy. And then finally you stimulate glucose uptake.
[00:14:41] So insulin does do that, but just at higher levels. And if you administer very large doses of exogenous insulin. As a body builder might do, and you also make sure to eat enough carbohydrate with that, because that’s the dangers you can drive bloke glucose very low. Yeah. If you do that, potentially die and potentially die.
[00:14:58] Right. You go into a hypoglycemic coma and that, that has happened. But if you do that, then potentially at super physiological levels, insulin may be antibiotic. But in general, day-to-day life, it’s not, but you can, as with everything, manipulate the system to, if you’re trying to.
[00:15:15] An extra bit of masking, which probably most people listen to this, would not be wanting to do.
[00:15:19] Dr Mike T Nelson: So just by eating my two poptarts, I’m not gonna get a high enough release of insulin to get close to that super physiologic level, correct?
[00:15:28] Dr Tommy Wood: No, absolutely not. So what’s happening when your blood sugar spikes and then comes down after you eat your pop tarts, the the blood sugar going up is coming from your, largely from your pop.
[00:15:39] But the main thing that insulin is doing in that scenario is telling your liver, Hey, we don’t need to make any glucose, because there’s Pop Tart’s on the way.
[00:15:47] Dr Mike T Nelson: So that’s the first. So it’s shutting down the production. Yeah. It’s not necessarily a. I’m using my little error quotes here. A disposal agent.
[00:15:55] Exactly. Because that’s what’s classically taught, right? Yeah. Oh, I eat Pop Tarts, insulin comes out, woo. Insulin shoves all this stuff into tissue. Yeah. Which is true at a high enough level, but it’s also having another effect.
[00:16:09] Dr Tommy Wood: Yeah. And and the other effect is by like on a day to day basis, and a healthy person is by.
[00:16:14] The vast majority of what insulin is doing. And it’s interesting because if you then get into a state like type 2 diabetes, where you’re insulin resistant, you have high levels of circulating blood sugar. The majority of that is unregulated glucose production by the liver. It’s not because insulin isn’t shoving glucose into cells and glucose uptake into cells in types of diabetes is actually high.
[00:16:36] Those cells are still taking up loads of glucose. It’s just there’s so much coming out of the liver that it’s, the system isn’t regulated. So most of it is happening. Like it’s extra glucose that you are making, which you shouldn’t be. Like that’s the big effect that’s causing high blood sugar in type diabetics.
[00:16:51] It’s not that the cells aren’t listening to the signal or not taking up the.
[00:16:55] Dr Mike T Nelson: And so that’s why certain drugs that affect the production, that the liver are effective for type two diabetics.
[00:17:00] Dr Tommy Wood: Yeah. And so anything that you can do to improve insulin sensitivity pretty much in any cell will buffer that process.
[00:17:09] But yeah, so any, so something that improves metabolism of the liver will definitely help. There was a class of drugs called the Glitazones. Yeah. Which were PPAR agonists,
[00:17:19] Dr Mike T Nelson: weren’t they from? Are they ones from the lizards?
[00:17:21] Dr Tommy Wood: No, that’s the, oh, I’m mixing them up. Yeah that’s exenatide, which is a G which is, yeah.
[00:17:26] So Exenatide is from the, and that is, that’s a GLP one. GLP one, okay. You’re right. Yeah. But, so these is a P part agonist and it increased insulin sensitivity. But then what happened was because people’s fat became more insulin sensitive, they were really, then they, their cells were much better at taking up more fat.
[00:17:44] So like the amount of fatness that you can get is like your metabolic buffer in this whole system. And so one of the downsides of making a tissue more instant sensitive, particularly if it’s the fat tissue, is that it will get fatter. And then there would, the reason why they don’t use those drugs is cuz some of them cause cardiac issues, but, so you can create insulin sensitivity.
[00:18:03] But that’s not always a, that’s not always a good thing if you’re then trying to think about, overall weight and other things.
[00:18:08] Dr Mike T Nelson: But we would actually want to take fuels and have more, I think of it as sinks to dispose of it in, right? If we can take these fuels and drop ’em into the liver, if the liver was low on glycogen, The muscle or fat tissue is if we start having fat tissue, that is becoming more insulin resistant.
[00:18:30] So we’ve taken that away as a sink to put substrates, right? Things floating around in the blood. We may potentially get leaner, which is debatable, but then we’d start having health consequences because of that.
[00:18:43] Dr Tommy Wood: Correct. Yeah. So I think of our fat stores as our main metabolic buffer and pretty much.
[00:18:50] All of the data, I can’t say all, but most of the data in this arena suggests that having healthy fat tissue that isn’t full, like you haven’t filled your stores, and what constitutes the capacity that you have, there are multiple different things that feed into that. But soon as your fat stores are full for whatever that is for you, that’s when you’ve lost your buffer and then you start to see this over spill.
[00:19:15] You’re not able to store anything and then fats just end up getting stored wherever they can get stored. So sometimes they’ll on top of the liver, the pancreas, the muscle tissue and so you’ve lost that sink. You can buffer that again with physical activity. So that’s obviously something Yeah.
[00:19:28] That is very protective. And yesterday we talked about sum wrestlers. Have stored vast amounts of body fat, but being so active in training so frequently their muscles are a huge sink for glucose and actually keep them metabolically healthy while they’re still active. And even in most people, the vast majority, so it’s 75% of all glucose uptake goes into the muscle tissue in people eating a standard mixed diet.
[00:19:53] At least 75% of that, but potentially more is non-insulin-dependent. So it’s basically, it’s just stimulated by the movement of the muscle tissue. And so just activating the muscles causes the translocation of glute four to the surface. So you don’t need insulin to do that. And I would argue that you’re probably gonna be in much better health overall if you’re not relying on insulin to do that.
[00:20:16] You are just doing it because you’re activating the muscles through whatever exercise or movement it is you’re doing, and then having more muscle tissue is gonna potentially give you a bigger buffer. Yeah.
[00:20:25] Dr Mike T Nelson: What are your thoughts about My bias is also movement, right? So first, move as much as you can.
[00:20:31] Don’t worry about what fuel you’re using. Don’t be so hyper specific cuz most people just don’t move enough. Don’t. Yeah, but what about a population that’s doing that pretty high frequently? Their step count is good. They’re doing formal exercise. Do you think it’s of a benefit to do something like fasted cardio or ways to increase the burning of fatty acids?
[00:20:56] So that you’re, in essence pulling more fuel through the fat cell to allow that to be a little bit bigger buffer if
[00:21:05] Dr Tommy Wood: needed. Yeah, that’s a good question. I think that’s my bias, and you can tell me if it sucks. No, I don’t. I don’t think, I don’t think it do suck. It does suck at all. And I was soccer tour and I’d definitely am a.
[00:21:16] A proponent of your idea of metabolic flexibility. I certainly agree that you should be able to use the right fuel at the right time for the right, for the job that you’re trying to do. And so that requires capacity at both ends of the spectrum. And most people again, if we, so going back to general population, most people just aren’t.
[00:21:35] Giving that aerobic system time to really rely on fat, you’re continuous, you’re continuously suppressing lip lysis by just like continuously eating. And it’s not necessarily because you know it’s the carbs or the carbs make you fat, but if insulin is high enough, you’re not relying on those body like tissue stores to then run the system.
[00:21:53] And so doing periods of that, I think definitely gonna be beneficial and when I’ve worked particularly with endurance who are gonna rely a lot on that system. Fasted cardio sleep low, those kind of tactics to stre not stress, but you push or you use that system.
[00:22:09] I think it definitely beneficial in terms of the overall adaptations. Yeah.
[00:22:12] Dr Mike T Nelson: Yeah. Cool. What about this line, which is a quote I stole from Jeff Volek and I’ve used it a lot, but I always wonder in my head about simplistic codes, and maybe I made it too simplistic. But the insulin is a fuel selector switch.
[00:22:28] . So higher levels of insulin kind of pushes you to use carbohydrates or glucose. Lower levels push you to use fat. Yeah. From a, would you agree with that? Just from a fuel selection standpoint? Obviously insulin does more
[00:22:40] Dr Tommy Wood: than that. Yeah, so I think it’s it’s definitely it’s like an, it’s an integrator of fuel metabolism largely via the liver.
[00:22:49] And that’s def you know, and that’s definitely, you just think about all the things that it does, even if it’s not pushing glucose into cells. What it’s doing is it’s reducing the availability of endogenous substrates, which are largely gonna be amino acids and fats. Once you, particularly, once you get.
[00:23:05] Whatever liver glycogen you might have. So it is then putting you into a state where you’re going to be using carbohydrates as your main fuel source. So that’s, so where insulin acts in that system maybe isn’t so well understood, or I don’t think it’s described as accurately as it could be, but in reality that is what it’s doing.
[00:23:25] Yeah.
[00:23:26] Dr Mike T Nelson: Cool. What other parts do you think are misunderstood about insulin that are useful to the average person listening?
[00:23:33] Dr Tommy Wood: So I think the most important thing to me, what, other than just, having a better idea of what it does and when it should be doing it, is that I spend a lot of time in the low carb sphere.
[00:23:50] And insulin is definitely the bad guy, right? Like it’s boogeyman, right? It’s the boogeyman and it does, it does. So it’s, it is elevated insulin is associated with, or it integrates with a lot of other pro-growth pathways, like the IGF one pathway and they integrate through different mechanisms, but like through mTOR and if you are continuously stimulating that you potentially increase risk of cancer and some other type two diabetes as, as well.
[00:24:13] And yes, that’s definitely true. However, insulin and normal insulin signaling, including potential spikes or, some peaks in insulin are very useful. So you need normal insulin signaling for various good things to happen in the brain. And just like saying, getting your insulin as low as possible, I think is very unhelpful.
[00:24:32] And in. That same space we talk about in, or people talk about insulin resistance as a root cause of modern disease, and it is. So insulin resistance, so which would be anything in the spectrum of dysregulated glucose metabolism, basically. That’s the easiest way for us to measure it. At least.
[00:24:49] So elevated fasting blood glucose, elevated C peptide, anything like that triglyceride ratio. You can all use these as proxies. All of those things, insulin resistance is associated with Alzheimer’s disease, cardiovascular disease multiple types of cancer, like I said. And so people think of it as this like core central thing, but in reality, insulin resistance doesn’t just happen.
[00:25:12] So what annoys me is when people say insulin resistance is the problem, but what is it that caused the instant resistance? I think that’s much more interesting and much more I. So you can’t just stop at insulin resistance, say hey, we know what the problem is, it’s insulin resistance. Cuz usually then the answer is eat less carbs.
[00:25:28] where is, but there could be many other things feeding into that. So that’s the most important thing that I think people need to know is that, Insulin resistance isn’t the end point. There are things that feed into it and the answer isn’t always eat less carbs, although that can absolutely help.
[00:25:43] Dr Mike T Nelson: Yeah. But I think, I always think of the eating less carbs as what context a person we’re talking about. Yeah, absolutely. If it’s Bob who’s looks like a couch coach, then who doesn’t move at all and is eating like seven 11 Slurpees with no. Yeah, cutting back on the carbs is probably gonna help Bob. Yeah.
[00:25:59] If it’s a CrossFit athlete doing two a days, I see them like not eating enough carbs to even fuel their exercise. Yeah. And those two populations are completely different, right? You’re talking about one who’s pretty healthy, physically active, one who may even have underlying pathologies, not physically active.
[00:26:18] And it seems especially in health and fitness, we wanna conflate both of. And we always just talk about the thing and not necessarily the context of what it actually means in each area.
[00:26:29] Dr Tommy Wood: Yeah, and I think what I’ve seen a lot of is people who work in Populations with a pathology, obesity, types of diabetes.
[00:26:39] They have these strategies that may include extended fasting. Some of them are anti protein for whatever reason, carbohydrate.
[00:26:47] Dr Mike T Nelson: It’s a whole nother podcast,
[00:26:48] Dr Tommy Wood: I’ve actually seen clinicians. prescribe protein levels that I thought would probably should constitute malpractice. But that’s like a whole different.
[00:26:58] And so like they’re using these tools in sick people when they can be, where they will act, absolutely be beneficial in for some period of time. So you need to move on to the next thing. But the people who are listening to that message are not those people. They’re the people who are hyper focused and hyper interested in their health.
[00:27:16] So you’re right, we, I’ve worked with CrossFitters who. I need to eat a low protein diet cuz protein causes cancer. I need to eat a low carbohydrate diet because that will make me the optimal fat burner, and or I should intermittent fast because auto course top, bro. Yeah, because auto and then you’re eating, you’re averaging like 1500 calories a day on a guy who wants to train 20 hours a week, like good luck.
[00:27:38] What do you expect is gonna happen? Yeah. Then he, he turns up thyroids trashed libido completely in the, in the toilet. And that’s exact, so that’s, I think that the problem is, The message is coming from people who work in pathological populations. And the message is being listened to by people who are active and trying to do everything at the same time.
[00:27:56] And then that combination often, really hurts the listener.
[00:28:00] Dr Mike T Nelson: Yeah, I’m in the same argument cuz I get hate mail from like everybody now about ketones that like, people are like, oh, you’re so anti ketones, you don’t like the ketogenic diet. What context? Yeah. So for a while I had the ketogenic, the CrossFit people who would come in and eight weeks would go by and they felt great and all of a sudden they felt like they got hit by a truck and they can’t figure out what’s going on.
[00:28:21] Yeah. But if you look at actual pathologies, type two diabetes, maybe TMI or TBI head trauma. Yeah. Bunch of other things. Like I think a ketogenic diet could potentially be amazing. Yeah, absolutely. I don’t always see it go the other way. Just because it’s really good for some type of pathology doesn’t mean that it’s gonna be the cat meow for performance and vice versa.
[00:28:44] Yeah. Yeah.
[00:28:44] Dr Tommy Wood: So just because anything works in any in one population and that’s great and we want as much of that information as many of those studies as possible. But then to generalize that is I think is a big misstep that far too many people are doing. Yeah. Yeah.
[00:29:00] Dr Mike T Nelson: Cool. So as we wrap up two question.
[00:29:01] One, you had mentioned a few blood tests. Are there some simple blood tests or other markers, performance things if people are listening to this and trying to decide, do they have any insulin resistance and how would they
[00:29:13] Dr Tommy Wood: know? Yeah, so I think the. The things we mentioned, fasting blood sugar is a good one.
[00:29:18] What number
[00:29:19] Dr Mike T Nelson: do you wanna see for that?
[00:29:20] Dr Tommy Wood: Under 90? Under 90 is ideal. It’s 80 to 90 is ideal. Okay. If somebody’s on a ketogenic diet, it may well go lower than that. Sure. But in some in populations eating a mixed diet, 80 to 90 seems to be the sweet spot in terms of disease. Triglycerides HCL ratio, ideally less than two if you’re working milligrams for deciliter.
[00:29:38] Yeah. Closer to one if possible. A lower threshold, maybe 1.5. In populations who aren’t Caucasian they tend to see less of an increase in triglycerides when they start to become insulin resistant. You can certainly look at things. If you are willing to spend a bit more c peptide gives you an idea of how much insulin was released the whole 24 hours before.
[00:29:55] We talked about before. Yeah, fasting insulin isn’t as good, but it’s another measure might be easier to get. Then I think one really nice thing to do is just like tracking your own. So you don’t need to do this on a lab test. You just get a gluco to have at home. So we talked about, how high is your blood sugar spiking after a.
[00:30:12] Ideally it shouldn’t go up by more than, definitely not more than 50, ideally not more than 30. Okay. So say it’s it’s 90, you have breakfast, it goes up to 1 20, 1 25. Within an hour to 90 minutes it’s back down closer to where it was initially. That’s great. Anything where the peak is a lot higher than that.
[00:30:32] So the peak is more than 50. So say it’s, initially it was okay, so maybe you were like 95 to. But then it goes up to 1 45 or one 50. It takes a little bit longer to get down, not to two hours or a little bit longer. Then you’re maybe thinking, okay, this is this is where your, maybe there are some issues going on.
[00:30:48] So that’s all super easy stuff to get. You can, like any primary care physician would give you a fasting blood glucose and a basic lipid panel where you can get triglycerides to HTL ratio and a glucometer can be like 20 bucks. So it’s definitely super easy to start looking.
[00:31:04] Dr Mike T Nelson: And if you were to add something, like if you think you’ve got high glucose excursions, like a glyco mark test might be useful.
[00:31:10] Dr Tommy Wood: Yeah, that’s definitely useful in populations eating a mixed diet. Glyco mark is one five and hydro gluco. And it, you get it in the diet, you get it in your food, and it competes for reuptake with glucose. So when glucose go typically above 180 milligrams of deciliter. So when your glucose goes above that, you start to lose glucose in the urine.
[00:31:30] And then what happens is your glyco mark goes down. So if your low glyco mark that’s a kind of a sign that you’re getting big glucose spikes. It doesn’t seem to work in people eating low carbohydrate diets, cuz they’re actually consuming less of the one five anh. So it artificially lowers it.
[00:31:44] So when I’ve, we’ve seen a lot of ketogenic people eating ketogenetic diets is always low, but we know they’re not spiking that quite. Oh, gotcha. We didn’t mention hba A one C. Okay. That is a decent, and again, any primary care physician would get you that. It’s a decent marker as long as you’re testing against yourself.
[00:32:00] Yeah. So it’s something to track over time rather than say you get a one off and that’s good or bad. Yeah. Unless it’s like very high, like six, six or something crazy. Six or above six. If it’s like in the five somewhere or if it is above six, and you do something about it, watching it track over time and having your own days to compare to is useful.
[00:32:19] Having like my 5.5. compared to your 5.5 in terms of average blood sugar, all that kind of stuff is completely different. It doesn’t necessarily it’s not comparable between people, but within yourself is useful. Fructo is another one that’s like a shorter term. Its like a short term HBO one c like 30 days rather than three months.
[00:32:37] So those things too. But, I’m I always. I always think of, are these all different ways of turning you the same thing? And probably they are. So if you get a couple, if you get a couple of them and they agree, then you probably have an idea of the picture without having to do all of them.
[00:32:50] Cool. Awesome.
[00:32:51] Dr Mike T Nelson: Thank you so much for your time today. I don’t know, do you still do any consulting work? Are you pretty much full or how would people find you or. Maybe you just wanna hide in the jungle Costa Rica and not be found . Yeah,
[00:33:03] Dr Tommy Wood: I people can find me on Instagram at Dr. Tommy Wood. Usually, I’ll post stuff on there a couple times a week.
[00:33:09] I mainly do full-time research now and then when I do work with people, it’s usually through somebody else. So there’re a handful of physicians who will reach out to me if I can help interpret some labs or come up with some ideas to help. Help their clients or patients. So I’m, I act more, more and more as a consultant rather than a direct a direct physician.
[00:33:29] But if somebody is certain that I might be of use, they’re always welcome to message me on Instagram or my website is dr ragner.com. And find me on there. And that’s
[00:33:39] Dr Mike T Nelson: literally your middle name? It’s my middle name,
[00:33:41] Dr Tommy Wood: yeah. Yeah. So people just always I don’t get it. So that’s my middle name.
[00:33:44] It’s also my handle on Twitter, but by the time I, I. Like succumbed to Instagram, somebody had already taken it, so that’s why the handler is different. But yeah so any of those if I can answer any questions I definitely will.
[00:33:56] Dr Mike T Nelson: Cool. Awesome. Thank you so much for being here today.
[00:33:59] Thanks. Greatly appreciate it. Yeah.
[00:34:02] [00:34:04] Dr Mike T Nelson: So big thanks to Dr. Tommy Wood there for a wonderful interview. Again, recorded live in Costa Rica at the Flow Retreat Center. There big thanks to Dr. Ben House for having myself down there along with Dr. Tommy and everyone for two weeks this past March. You can go back and also listen to the podcast I did with Dr.
[00:34:31] Eric Hos. We talked about our experience there in Costa Rica, and he talked about also some work on a periodization for training. So this podcast has been brought to you by the Flex Diet Certification. If you want eight different interventions for training and nutrition recovery to use both with yourself and with your.
[00:34:55] Based on the concept of metabolic flexibility and flexible dieting, check that out www.flexdiet.com. And if you enjoyed this drop us a review on the old iTunes or whatever your favorite podcast listening device. We will read each one of them and do our best to incorporate your feedback.
[00:35:21] So thank you very much, greatly appreciate it. Talk to you soon.
[00:35:27]







Leave A Comment