On today’s episode of the Flex Diet Podcast, I talk with Dr. Scotty Butcher, aka The Strength Jedi, about the intersection of breathing and heart rate, HRV, self-regulation, and more. Enjoy the show!
Head over to miketnelson.com and sign up for my geeky, almost-daily email newsletter about how to add muscle, increase your performance, and improve body comp all without destroying your health.
Listen to hear:
-
[0:38] Intro to Dr. Scotty
- [8:19] How CO2 may be related to anxiety
- [18:35] How breathing is related to performance
- [23:45] Respiratory variability
- [34:37] Is over-breathing a trained response?
- [39:16] How to get more physiologic headroom
- [48:46] How breathing and performance relate to HRV
- [1:02:56] Human dynamic response
- [1:05:02] Tips for down-regulation
- [1:10:57] Favorite bands
Connect with Dr Scotty Butcher:
Referenced link:
- Flex Diet Podcast S2 Ep 13: Interview with James Nestor, author of “Breath: The New Science of a Lost Art”
About Dr Scotty Butcher:
I have been a Physical Therapist for 25 years and a University Professor for 15. I have advanced training in strength coaching, wellness coaching, mindfulness, meditation, clinical exercise physiology, and applied biofeedback. I practice, study, and teach strength training, biofeedback, exercise recovery methodology, and mindfulness. I have been fortunate to be able to pass my knowledge and skills on to others locally and across the globe.
Rock on!

Dr. Mike T Nelson
Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
Welcome to the Flex Diet Podcast, as you can tell this is not the voice of Dr Mike T Nelson, this is an AI generated voice as Dr Mike has been yammering too much in Canada and has lost his voice; but the show must go on. Today we have on the podcast Dr Scotty Butcher and we talk all about the intersection of breathing, heart rate, a bit on HRV, self regulation and more. Enjoy the show!
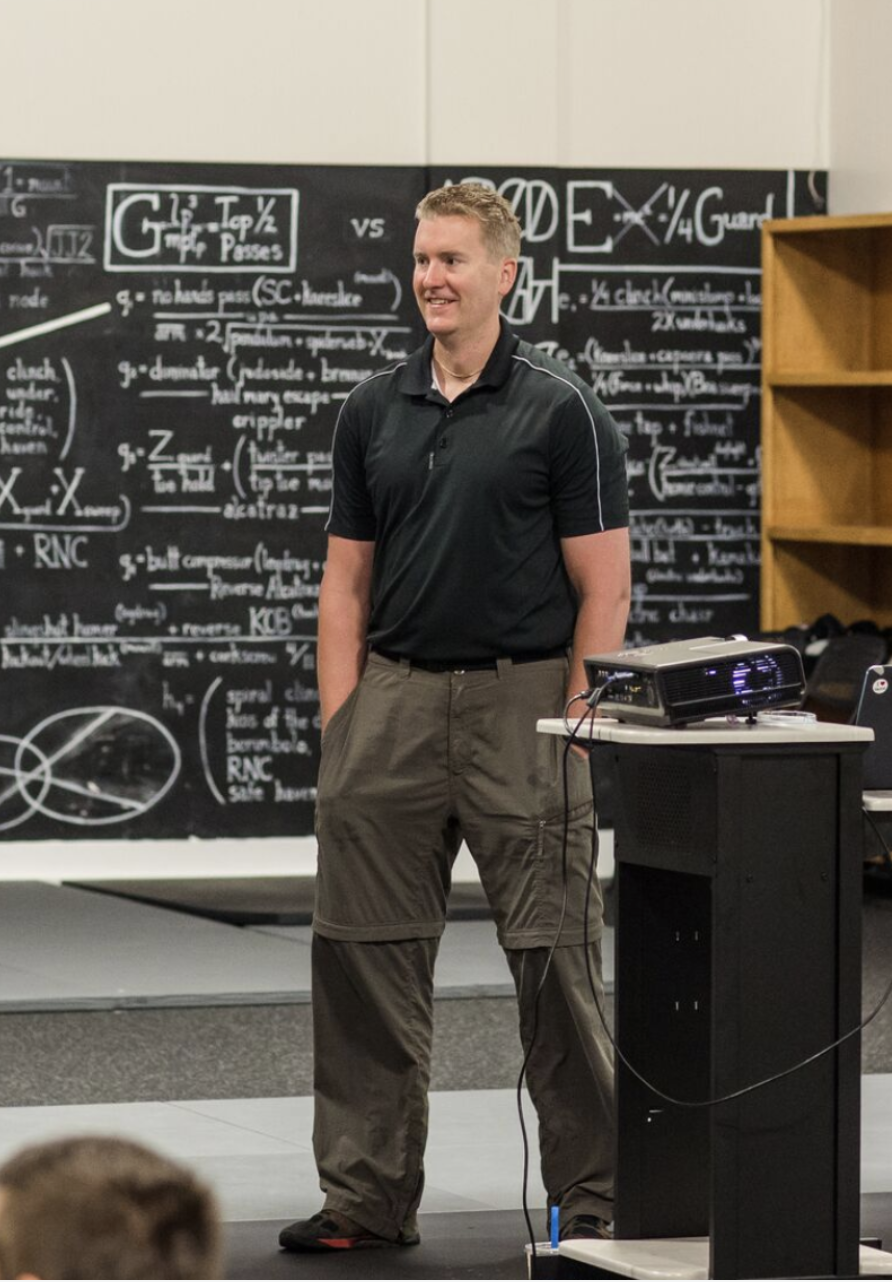
[00:00:21] [00:00:22] Dr Mike T Nelson: Thank you so much for being on here and we got to finally meet each other in person at the neuro sports conference in Florida a few months ago, which was great. And why don’t you give just a rundown of some of the broad view of the topics you were talking about there, cuz that’ll kinda lead into what we’re chatting about.
[00:00:38] Dr Scotty Butcher: Yeah, for sure. For those that maybe haven’t heard of me before, I’m a professor of physical therapy and I also run a a company that is mind body strength, but I go by the handle strength Jedi. And so I’m a physical therapist by background. I got a PhD in respiratory physiology and exercise physiology and blend all of that stuff together into a let’s put it a very personal journey over the course of my adult life that has really taken me into lots of anxiety with with diagnosis in generalized anxiety and social anxiety disorders.
[00:01:16] And a lot of that came back from a concussion back in my early twenties, but, What that led to, of course, is my interest in all things stress and stress, resilience and how we can look at stress and anxiety management. And so that’s where a lot of my research and my clinical practice has gone in recent years has been along those lines.
[00:01:37] And of course, me being a physiologist and not a psychologist I really wanted to delve into the physiological aspects of anxiety and stress management, which of course then led me to H R V as being one of the, one of the sort of universally well-accepted markers of of stress and recovery and all these other blanket things that, that’s under the H R V umbrella.
[00:02:02] And Then I, then it dawned on me that I also had to learn some psychology. So I’ve done some deep dive in the the psychophysiology side of things of breathing, which is something that I never learned in my in my PhD training. Taking the H R V and actually applying it in different contexts and around breathing and breathing behavior as being a big part of it and how we tie our emotions in with our, in, with our physiology and how I guess from a mindfulness perspective, that there’s very much a physiological effect and an anatomical morphological change that happens with mindfulness-based training which is where I’ve really taken my work is in biofeedback, and it’s so mindfulness-based, heart rate variability, biofeedback is the main thing that I’ve been focusing on over the last, I guess five, five-ish years.
[00:02:48] Dr Mike T Nelson: Very cool. And do you remember like when about you got into H R V? Cause I know you’ve been doing it for quite a while and I’m always curious to give someone I teach, I give a background in history because I think, especially not to rip on students nowadays, but you can run almost everything through your phone and that was not always the case.
[00:03:09] And so it’s sometimes I think, hard to appreciate some of the leaps in technology when you never had to suffer through the early versions.
[00:03:17] Dr Scotty Butcher: Yeah. You know what I in HRV I’ve, some of the physiology that’s out there, like I, I learned. Whew, I learned on a you not the digital graphing.
[00:03:28] So software and computer stuff. It was all on the in original stuff was on analog, but I wasn’t doing HRV at the time. It was breathing mechanics and the type of things that I was doing for my PhD and looking at respiratory pressures and pressure management and work of breathing. And tho that’s where a lot of my p early PhD work came from.
[00:03:45] But H R V actually got lucky enough when, as I was being introduced to it, it was just coming onto the market. I think commercially where you could get some of it on your phone, but Nice. It wasn’t at the level where, you can actually use the phone camera and like that stuff wasn’t there.
[00:03:59] I had to purchase some extra devices which of course I recommend now anyway. But had to go into actually the very first one I purchased was a core sense from a elite HRV. And so it’s the finger clip Martin in that. Yep. Yep. That’s right. And so that, so in terms of that deep level, I would’ve said I’d say that’s about four years.
[00:04:19] Yeah. Yeah. Very cool. That sounds about right. Yeah.
[00:04:21] Dr Mike T Nelson: Yeah. I know you’ve been doing a lot longer than that. I will refrain from doing the back in my day. But yeah, the short version is when I did my PhD stuff on HRV, we had $20,000 of used equipment and we had, so for people listening for HRV, one of the big issues was how do you take the EKG, right?
[00:04:41] So you’ve got the pointy, what they call the rwa, which is the top of the Q R s, the ventricular contraction, the electrical signal, and that top little peak pointy R wave, you have to find the distance to the next peaky pointy R wave. And that has to be calculated within just a few milliseconds in order for H R V to be accurate.
[00:05:01] So the earliest stuff, the hard part was picking off the peaks of the actual, what they call R waves. And then you had the r, what they call RR intervals. And then you had to make sure there wasn’t noise, and then you’ve got potentially the effect of breathing, whether you wanted to deal with that or not.
[00:05:17] And long story short, we had a 20 grand of use equipment. People had to come in the lab, they had to be rested, we had to do all these measurements. I then had to take that data, I had a custom write of MATLAB program to get the RR intervals and make sure they were accurate. I then had to upload that into a, another system called koos, which would then crunch all the numbers and stuff for it.
[00:05:38] And it worked. It was a pain in the ass. And so the beautiful part about having it on your phone, As we’ll talk about is you can do daily measurements. It doesn’t cost you anything. It’s free. It takes a couple minutes. And the one-off H R V measurement, eh, not super useful. We were using it in studies to see the effects of energy drinks, so we were purposely injecting something else into the system to see if it actually moved or not.
[00:06:04] But for day-to-day use, having that measurement most days outta the week makes it then practical and you don’t have to go to a lab in order to measure it. Makes it a lot more.
[00:06:14] Dr Scotty Butcher: That sounds a lot like the ins and outs of what I had to do. And here we are, the old guys talking about back in our day, you said you weren’t gonna do that, but we’re doing it. Yeah,
[00:06:22] Dr Mike T Nelson: the, yeah. But it sounds at
[00:06:24] Dr Scotty Butcher: this point, yeah, the the pressure management stuff and the work of breathing you can calculate areas of circles now. Yeah. And loops and things like that with good software. I was, I remember doing that manually with a really old school, what’s called a perimeter.
[00:06:40] And it’s one of those really old school map mapping functions or mapping tools where you can actually just, map out the area of something that’s on a piece of paper. So I had to get the scales right, print it all off in terms of these pressure volume loops, and then take the, this perimeter, which is basically like a, it’s almost like a microscope, but you have to like trace it so acutely that you’re like right along the line of it.
[00:07:08] And, oh my God, did I ever go bugeye? I lost my eyesight, but almost doing doing those, countless hours of that. But I guess that’s research too, is you got you get that aspect, but man, I would’ve loved the today’s technology
[00:07:19] Dr Mike T Nelson: back then. Yeah. Yeah. And talking about respiratory physiology and related to anxiety.
[00:07:28] What are your thoughts on I think with the book breath, that was I think probably one of the, maybe you could say Patrick McEwens stuff maybe before that. And there’s been people who have talked about it. But I think Breath by James Nester was on our podcast here. People can check out that episode.
[00:07:45] It was the first time people, I think, looked back into breathing again at a more popular level. And one of the things he talks about in there is the role of co2, so carbon dioxide and how it’s related obviously to exercise performance, but also potentially anxiety. And we were always taught that, co2, ah, it’s just a waste product.
[00:08:05] And then now we’re realizing that it does different signaling things. It does all sorts of stuff in the body. So any thoughts about how CO2 may be related to anxiety and what are potentially some of the mechanisms.
[00:08:19] Dr Scotty Butcher: Yeah, for sure. Great question. This is you know what I mentioned earlier about the psychophysiology piece of it?
[00:08:25] This is really where a lot of that comes from. And I was very fortunate to be exposed to some training in just about a year ago from a very in, in this world scientist, but not popularly well known someone that was really in the. The realm of the psychology piece of breathing named Peter Litchfield.
[00:08:45] And he is he runs the school of professional behavioral sciences. And I took a course on the certificate course on breathing behavior analysis, which really brings all this this in. And so this was honestly not my very first exposure to this of course, but it was my real deep dive where I really started to understand a lot of this.
[00:09:04] Cuz I, absolutely, you’re correct. Like I said, I did a PhD in respiratory physiology. And everybody back at that time was talking about how CO2 was purely a waste product. And so a lot of this stuff was never really obviously it had a role in acid-based balance for sure.
[00:09:21] And the respiratory system in terms of balancing the metabolic acidosis and from a clinical perspective as well as an exercise perspective. So there, obviously there were some, there was some recognition that CO2 had a a bigger function, but not to the level of what we understand now.
[00:09:37] And it’s really interesting cuz most of the research was done well before then it was done. Oh, yeah. Back in the seventies and eighties and even before where you’re getting a lot of that and a lot of that early research came from the anesthetic world where they were doing brain surgeries and other type of surgeries and they had to titrate the blood flow to the brain.
[00:09:56] And so this is the interesting link, or one of the potential interesting links is that, You can over breatha, right? We know that. We know that you can take in more air and expel more air purposefully because we are involuntary control of this involuntary system. The res respiratory system is seen to be involuntary, right?
[00:10:17] You can your sleep and you breathe. You don’t have to think about it, but you can think about it and you can manipulate it. So if you over breathe, what what a lot of people I appreciated actually your most recent one I forget what you called it. It was the, oh, the hardcore physiology one.
[00:10:31] Oh, yeah. Breathing. Yeah, I listened to that yesterday before I came up. Oh, thank awesome. Yeah. No. It was great. And Oh, shoot. Lost my train of thought from there. Oh over breathing. Yeah. So you go into over breathing and you can, you can’t really without increasing the pressure, as you mentioned, take in more oxygen.
[00:10:48] And the whole, the, all of the whim h stuff and the other people that are saying that, you’re hyperoxic oxygenating your muscles by over breathing and things like that, that’s totally bogus. But what it does do is it does lower your CO2 levels. So CO2 is titrated very closely with the amount of ventilation that you have.
[00:11:03] And so if you lower your CO2 levels in your blood by breathing heavily more heavily, or in the case of surgery, you have the the ventilation, the external ventilation that’s put on these people, you over ventilate them to drop the CO2 levels. What that does and what they knew from that is that drops the blood flow to the brain.
[00:11:23] So if you’re gonna do brain surgery, you’re not gonna want a lot of bleeding. You’re gonna wanna decrease that. And so there’s some evidence, and it hasn’t gone a lot into the clinical realm yet, but there’s some evidence to say that if you drop your CO2 levels there’s a couple stats that I’ve heard put around there that I think have some validity to ’em.
[00:11:42] Although take it with a grain of salt. Cuz again, these haven’t been validated clinically, but if you drop your CO2 levels by one millimeter mercury so normal range being 35 to 45. And so if you say you’re at the low end, 35 and you drop down to 34, some of the stats are saying that it’s about a four to 6% decrease in cerebral blood flow.
[00:12:02] Which also then relates to cerebral oxygenation and glucose delivery. If you can drop it even further there’s some estimates that you can get around 60% of a decrease in cerebral blood flow with dropping your co2. And that’s at the top end if you’re extremely hypo capic in, in that realm, if you, if again, this hasn’t really been.
[00:12:23] Looked at from a mechanistic perspective and how this relates to things like brain fog and anxiety and depression and other mental health or cognition or disorders. But there, we do know there is a correlation there. So if you have you take a, and there’s lots of good research on this.
[00:12:40] You take individuals that have anxiety and panic disorders and you measure their co2, their entitled CO2 s which is just a way of measuring the CO2 levels in the breath, but just at the end of expiration, which reflects the deep CO2 that’s right closest to the alveoli and the capillary. So it refl best reflects the the actual blood co2.
[00:13:00] And you can see that there is a very strong. Between anxiety and panic disorders and the severity of their symptoms with the amount of hypocapnia they have. We also know, and again, mechanistically I’m not willing to bet my life on the, or my career on the fact that if it, that it’s really the increase in CO2 that causes the change.
[00:13:21] But there is an association if you can change the breathing pattern to lower the amount of ventilation that’s coming in, which raises the co2, that actually improves symptoms. So it improves anxiety symptoms, improves panic disorders symptoms. Lots of good research in those areas. I would really like to see how this translates into multiple aspects clinically, because if you think.
[00:13:46] This, it’s not just it’s not just brain that we’re talking about and mental health that we’re talking about. I know you mentioned the bore effect in in Yeah. Your deep dive physiology, which is basically just saying that our, the level of oxygen saturation is related to the amount of oxygen that we have or the partial pressure of oxygen we have in our blood on a sort of a curve of linear relationship.
[00:14:08] And it’s designed to facilitate bringing oxygen into. Your blood at the lung level but getting it released from the hemoglobin at the tissue level so that we can actually use it. So the bore effect is, as is basically saying that let’s use exercise as an example. If you exercise where you heat the muscle, you provide more acid more acid environment, you and a bunch of other things that, that increases the c and an increase in co2, what that’s gonna do is that’s going to decrease the affinity for oxygen in the hemoglobin.
[00:14:41] So the oxygen is released more. The opposite effect happens, of course, when your hypo capic, when you go into an over-breathing scenario where your CO2 levels drop, is that the hemoglobin holds onto that oxygen more, there’s less ef there’s more affinity for for the hemoglobin to hang onto it, so there’s less oxygen being released.
[00:15:00] And of course we know that’s true of the brain because that’s where a lot of that research came. But it’s really interesting to think of the systemic effects of what would happen in an ex, an exercise scenario where you actually increase CO2 levels or increase ventilation, excuse me, and decrease CO2 levels where you’re supposed to be getting more oxygen delivered and and actually extracted from the blood into the working muscles where that actually doesn’t happen.
[00:15:30] And I can actually think of one scenario that has not been shown in the research to be to really be true yet. But I’ve seen this anecdotal, anecdotally. So if you’re, and this might be a real heavy physiology talk, but there’s, when we’re doing exercise and let’s say we do a VO two max test, there’s two anaerobic thresholds, right?
[00:15:48] There’s the first threshold, which is considered to be the point where we start relying a little bit more on anaerobic energy to produce the to produce the the a t p replenishment. And so at that point in time it’s called the buffering zone, where we start having some acid being produced.
[00:16:04] We buffer that acid with the primary buffering system being bicarbonate, and then we spit up more co2. So that’s a normal scenario, but we, but that’s within the realm of what we can buffer. There’s a point in time where we call this the second threshold. The second threshold is where we, we’re still, there’s lots of anaerobic energy happening.
[00:16:22] We’re producing a t p anaerobically. We get a lot of acid production, but there reaches a point in time where we can’t either buffer enough or buffer quickly enough. And what happens is the rate of CO2 just continues to go up. And this is whole body, whole CO2 that goes up.
[00:16:41] But what it ends up happening is this end title CO2 drops. And so at this second respiratory threshold, you have a drop in the end title co2, which again, is a correlate for the co2 that’s in the pulmonary capillaries that CO2 drops. But that’s also associated with a massive increase in ventilation and impending muscle fatigue.
[00:17:04] So what also happens at that point in time I’ve got some nears that I’ve tried this on, and I know you’ve you’ve got some Moxies and Yeah. I’ve used some Moxies for this sort of thing to look as well, again, not from a research perspective, just from an anecdotal perspective. And it seems to be that, that, that is the point where you tend to see an acceleration in the the drop in the seal or the the oxygenation.
[00:17:25] So it’s really interesting to think that that there’s a potential link there in this known phenomenon that we’ve had for a very long period of time. That might be because we are simply over breathing. Again, this is a theory, this is not mechanistic, this is not research based. This is just an interesting anecdote where this could apply beyond the typical situation.
[00:17:47] Dr Mike T Nelson: So if in practice, then, if you’re doing a. Absolute all out max VO two tests. So like I’ve done two K on a rover is a typical one that I’ll use, but there’s different forms, obviously step tests, et cetera. Would you get an increase in performance if you could control your breathing as you’re getting to that kind of absolute max point where everything is just burning, it feels horrible, like breathing feels like you just can’t get enough air.
[00:18:19] Would you be better off trying to do some type of controlled breath? But you don’t purely wanna limit the amount of air flow either because that’s gonna limit the amount of oxygen coming in. It’s gonna limit the model CO2 you’re getting rid of. Any thoughts on how you would find that happy medium?
[00:18:35] Dr Scotty Butcher: That’s a great question. Again, research wise, we, I don’t think that this has been studied, haven’t seen, to my knowledge anyway. Yeah. My, my thoughts are that there is a happy medium and finding it might be a bit of a challenge because of the reasons that you said. What I’ve done again, in just I’m a tech geek, and I love throwing, I love getting data.
[00:18:54] I love getting numbers. I’ve got a cap oter, which is basically a measure machine that you hook up with nasal prongs in, in your nose. So it’s just like the the typical cannoli that you would do if you were being delivered at oxygen. But what it does is it gets your CO2 levels and so what you do is you take the CO2 tracing, this is how you measure cap the.
[00:19:14] The hypocapnia or the normal capa those end entitle CO2 s And I’ve hooked myself up as well as a couple other of my test people not real research subjects. Just people that I’m playing around with. And we’ve tried some things like this and it’s it seems to be a good correlation with again, that second threshold where if at that point in time you try and just reduce the size or the rate of your breath just a tiny little bit, it brings the CO2 levels up.
[00:19:42] Now, whether that actually has a measurable I improvement in their exercise performance, I don’t know. But if you think of a lot of the subjective feelings that come along with that, that level of exercise, let’s face it, it’s a shit show when you get at that level, right? Yes.
[00:19:57] You’re trying to sustain it for a really long period of time. That, you feel like crap because your body is saying what the fuck’s going on? But. It, it’s, to me, I, and again, this is a post hoc fallacy, I think, and bias, to me, it felt better, and so I, I don’t know, and again that’s a really, from, two scientists talking about this. It’s I don’t know. It’s a theory and it’s something that I think would be worth exploring, but I think what it speaks to is it speaks to the idea that, a lot of the individuals that are talking about Controlling ventilation and learning to have some CO2 tolerance or build up your tolerance or what the breathing behavior analysis people Peter Litchfield would say, is that changing the behavior around and the habits around the breathing that you’re having so that you can, you learn that it’s actually a safe, easy place to be when your CO2 levels come up and we think of CO2 and CO2 tolerance from a purely biochemical perspective, but there’s emotional habits and triggers that, that come into that as well, that have to be considered.
[00:21:03] So it’s, when you say CO2 tolerance and trying to increase your C2 tolerance, it’s. It’s as much about the biochemistry as it is about the psychophysiology piece of it, where we have to decouple the habit of br over breathing to allow the CO2 to go up, to relearn that’s actually a safe place to be and that it’s okay to be there.
[00:21:25] And that the body actually eventually when people learn how to do this, the body feels better. You actually recognize in intercept that your your body feels better. So any symptoms you were having tend to decrease and that when you get into a norm, Norma Norma Norm epn, that’s what I’m trying to say.
[00:21:43] Dr Mike T Nelson: EPN area. Yeah. And one thing I’ve noticed with, after being in a lab and doing frigging God, hundreds of probably max tests of vo two tests of some kind, the people that seemed to do better were more controlled with their breathing all the way up to the end. The people who tended to do worse.
[00:22:04] And this could be just purely from, practice. These people tended to be higher level athletes, so they’ve got a lot more many thousands more hours into it. The people, you could just watch their breathing pattern and it would just become more erratic. You would see they couldn’t pick a strategy and they just would just go off a cliff where you could see higher level athletes, they would pick some type of pacing and they would try to hold that.
[00:22:30] So like what I try to do or tell clients is, when it gets really hard, yes the world’s gonna drop. So if I’m doing it on a rower, I’m just looking at that average watts because that’s gonna tell me, what performance wise I’m trying to hit, or the pace I’m trying to hold.
[00:22:45] And then kinda like with Brian Mackenzie stuff like pick some type of strategy. So start nasal breathing and then when you can’t hold that anymore, then I will nasal breathe and I will exhale, and then I’ll work on doing more of a forced exhale and at the absolute end. I’m gonna breathe in and out of my mouth, but I’m still gonna try to keep as best I can, some rhythm.
[00:23:05] And with rowing it’s a little bit more interesting cuz you have the handle and the movement going with it. Biking and running are a little bit different, so I’ll switch that to try to find some rhythm, whether I’m breathing one breath in and out, or two in and out. And I try to hold that as long as I can.
[00:23:23] And if I need to breathe more, I try to stay in some type of rhythm with it, which when you’re doing a max exercise at the end is like trying to hold two thoughts together is almost impossible. But if I can do that, it doesn’t feel quite as bad and usually my performance is better. Again, anecdotal.
[00:23:45] Dr Scotty Butcher: Yeah, it’s a great point, but I think, I do think that there’s some scientific validity to some of the things that you’re saying there because we know that there, there is we started this talk thinking about heart rate variability, which you haven’t really talked too much about yet, but That’s okay.
[00:23:58] There’s this thing around respiratory variability. And so there’s some, actually some interesting research on respiratory variability and that, the opposite is true with respiratory variability as it is with heart rate variability. You actually want less respiratory variability and you want to have more consistent ventilation.
[00:24:16] And so look, so those that are exercising and more erratic with their exercise ventilation, they tend to have less exercise tolerance and they tend to have more symptoms. And so I think there definitely is some validity there. It’s just one of those things that it’s okay, we’re cool.
[00:24:31] We’re at proof of principle. Kind of point in time in, in the research process, but we haven’t actually done the trials to actually see if we can manipulate this and change this. Cuz that’s the key question, right? Is it’s it’s cool. So this stuff is all associated, anybody that’s taken a basic science or statistics course knows that correlation does not equal causation.
[00:24:49] It’s it’s the point in time where we can say, okay, cool, anecdotally we see this and there’s some physiological reason to study this. And I think if you’re out there and you’re an athlete and you’re someone who is says, Hey, like I feel like my breathing’s erratic and I get these crazy symptoms, or maybe I’m suffering from anxiety and I know my breathing kind of throws, throws me for a loop or whatever.
[00:25:09] I think it’s worth. It’s not you don’t want to, as you said, you don’t want to try and completely hold your breath at a, at maximum at Max VO two, it’s your maximum exercise performance and do that consistently. I think that you’re, things are not gonna end well.
[00:25:22] But it, I think trying to regulate a little bit is a fairly safe way of looking at how to mitigate some of this stuff now. It, the, these are hard these are not hard things to do. You think about I’ve done a lot of work with patients with C O P D.
[00:25:37] And so when I teach my students that I, when I’m teaching them about exercise responses in c o t or in C O P D, it’s I get them to imagine breathing out through a straw. They can breathe in however they want, but then they breathe out through a straw, which is basically mimics what happens with C O P D at end exercise.
[00:25:54] It makes it extremely difficult. And so if you take that as an extreme version of what we’re talking about where you’re just slightly trying to. Decrease your ventilation and control it a little bit, you can go too far off the other side and then that would limit your exercise performance because then you have a, because of the change in the ventilation, you now have a self-imposed ventilatory limitation, which is what C O P D patients have just naturally because they have a top end of their ventilation that they can’t push beyond.
[00:26:25] Yeah.
[00:26:25] Dr Mike T Nelson: It would be like illegal there. A couple of people I’ve seen in the past, I’ve looked at their metabolic testing and I’m like, this looks weird. I’m like what type of breathing strategy were you using at max? Oh, I read all about nasal breathing and I was nasal breathing in and out.
[00:26:38] And I’m like, okay, so on a ma all out max, you’re actually limiting your airflow. So like you said you have a self-imposed limitation. You don’t have this from a disease process. It’s a mental thing where you can just get a lot more air in and outta your mouth than you can in your nose. Again, doesn’t mean you should never nasal breathe, you don’t want to be limited by airflow purely because you’re trying to breathe in and outta your nose during a max test.
[00:27:04] Yeah,
[00:27:04] Dr Scotty Butcher: exactly. If I were to do this and if I were to design a study around this, what I would do is I would, I’d have people go through varying trials of of exercise and I’d have them with the ome on and so that I can measure the end title co2 s And and this is what I’ve done with myself here is.
[00:27:23] Tried to maintain co2. So as I started to hit these thresholds and as things started to get harder, I first of all just did it naturally and measured at what point in time did the CO2 s the entitled CO2 S drop? So that was the starting point. And then the manipulation or the the intervention there is to be like, okay, let me just titrate my ventilation enough to keep a static end Tial co2.
[00:27:46] Cuz again, you don’t want, you don’t want CO2 S going through the roof. You don’t want to increase them because again, that’s gonna be as much of a problem as a decrease in co2. But what happens if you keep it relatively static? And again, this is where I thought I felt better.
[00:28:00] Maybe I had more exercise performance statistically or not, I don’t know. It’s hard to do with an N one. But. I think that would be the way that I would design that trial to, to try and keep so it’s really around titrating your ventilation rather than going purely to something like, Hey, I’m gonna nasal breathe, like you said the whole time, which is not within Brian Mackenzie’s gear system kind of concept, right?
[00:28:22] That you would you would do something that would just very gradually keep it at a at a steady level. So it’s a small titration, small change.
[00:28:31] Dr Mike T Nelson: Cool. So a couple more respiratory questions. We’ll transition into some HRV cuz they are actually related. What do you use as a definite two part question?
[00:28:39] What do you use as a definition of CO2 tolerance, which is a word that gets thrown around a lot and my bias is, I think there’s something to it, but if you ask like hardcore respiratory physiologist Dempsey outta Wisconsin, he’s I don’t even know what you’re saying. Because classically.
[00:28:56] It’s just not a thing. But what I’ve noticed is like doing a two K on the rower, there’s times where aerobically, I’m fit enough to get pretty close to my max or my pr, but I am just not used to sucking that bad. Like I’m, I feel like I’m just mentally, maybe just an off day, not prepared to suffer enough to do it.
[00:29:23] And so my thought pattern is one, practice, obviously two, maybe the increases in co2, there’s kinda like a gain system on the brain where oh, CO2 levels are going up. Oh, we haven’t been here for a while. Danger, ah. But over time, when you’ve done that and you’ve been there and you can control your breathing and it’s like a stress inoculation it’s not as, as threatening to be there.
[00:29:51] So is co2. Tolerance, maybe both. And maybe there is some type of gain on the system from more of a neurologic level.
[00:29:59] Dr Scotty Butcher: Great. Awesome question. I, I’ve obviously the guys like Jerry Dempsey and bruce Johnson and those guys like, like really informed a lot of the work that I was doing.
[00:30:08] Oh, yeah. A lot of respect for those guys, like
[00:30:10] Dr Mike T Nelson: the OGs in
[00:30:10] Dr Scotty Butcher: that area. Oh, they totally are. And you know what, they’re, they. Th they’re very highly versed in the in the literature as well, even the current literature. And that what’s interesting is that they do very much come from a physiological perspective.
[00:30:22] Cause of course they’re physiologists, right? Yeah. And this is where I think that the, if you are only thinking of biochemistry, and you’re only thinking of physiology, when you think of something that’s again, quotation mark, CO2 tolerance, you’re missing the boat because of the psychological aspect of it.
[00:30:38] And this is where I th I think there’s some significant value in looking at breathing as a habit and looking at breathing as something that is, you in tune your, you tune your brain into the habits that you develop based on the experiences you have. For example, I’m not thinking about exercises.
[00:30:59] I’m just we learned a lot of this in the context of of mental health and anxiety and emotional responses. But if you think of let’s just use the startle response as a, as an example. What happens when you’re startled, someone scares the crap outta you, right?
[00:31:11] You 10, first of all, you tense up, you gasp a breath in, right? And that’s your it’s a mini version of the fight or flight response, right? And so if you’re someone who has developed some emotional triggers or ties, and they don’t have to be trauma. I’m not talking about like major trauma, like it could be that, but it doesn’t have to be.
[00:31:32] It could simply be some fear around some aspect of some something that you’ve learned. So a habitual fight or flight tensing style response that impacts your breathing. And so if you’re exposed to that, then you develop a negative breathing habit. You develop a habit where your body says it’s safer.
[00:31:55] To be in this fight or flight response and where I am over breathing a little bit and that’s the norm, that’s where I’m safe. And you learn to habituate the level of ventilation at that level. And you know that you could translate that over to exercise and say what, if you’re, you have suffocation style response, you get a lot of people putting face masks on and feeling like they’re suffocating.
[00:32:17] Is that, is how much of that is emotional versus how much of that is biochemical and actually respiratory gas exchange, it’s probably very little to do with gas exchange and much more to do with the psychological side of things. And so if you think. Exercise and heavy breathing during exercise.
[00:32:36] From that lens, you could almost think of it as well. People will over breatha during exercise as a habit. Now, of course, I’m not saying you, you can exercise like, and then we, I think we talked about this is you can’t. Keep your nor your resting level of ventilation in an exercise to maximum, right? Of course, it’s gonna go up.
[00:32:53] So when I say over breathing, I’m not meaning hyperventilation. Hyperventilation can happen, physiologically and biochemically to match the demands of exercise, to bring enough oxygen in and to keep the acid based balance. But what I’m talking about with this over breathing is going over and beyond that from a habitual perspective where you’re actually doing just a little bit too much and dropping the CO2 levels.
[00:33:17] And so if you habituate to those low CO2 levels or that style of breathing this is where a lot of people, you do a bolt score, for example, to get back to, how do I think of this? Or how do I measure this? You look at the bolt score, the bolt test as a, as an example. Normal breath in, normal breath out hold, measure your time, and some people will come out of that with that urge to breathe with a suffocation.
[00:33:39] Feeling Right? That’s emotional, that’s not biochemical. That’s an emotional, psychological response to the feeling of your CO2 going up and you’ve habituated to, to saying if you have a low bolt score, it just means that when your CO2 gets to a certain level, your body says, whoa, that’s way too much.
[00:33:58] I’m suffocating. I need to breathe. I need to get more oxygen in. I need to get more air in. Which of course is the misnomer you need to get more CO2 out is what your body’s actually telling you, but you don’t know that. So I think that one of the things that we really need to consider is related to.
[00:34:13] What are the habits that, that people have developed and why? And this is where it’s, it gets super complex because, psychology and physiology don’t often talk to each other. And they absolutely in the, in this case, they absolutely should. And this is where my deep dive into the biofeedback has really taken me into the psychophysiology.
[00:34:31] And me not being a psychologist has been, whew, huge majority.
[00:34:37] Dr Mike T Nelson: Got it. And do you think the, if we go with the hypothesis that a lot of people are over breathing, do you think some of that is a trained response, paradoxically, because they don’t want to get too high in co2? And I think there was some studies I think that James Nester referred to in breath about testing where they were inhaling pure CO2 and looking at different responses.
[00:35:06] And I haven’t done that. I. It’d have to be in a lab situation, blah, blah, blah. But I’ve talked to people who have, and they said it was like the most panic inducing thing that they’ve like ever done.
[00:35:19] Dr Scotty Butcher: Totally. Yeah. And yeah I have done that in the past and it’s it’s incredibly hard. And for me, coming from a history of anxiety, it was like my bolt score is trash, and then, so I’m like, I’m trying to work on this, and it’s, again, it’s a habitual thing.
[00:35:33] And it took me a long time to be honest, to learn. So when I first got into this whole world and started measuring my own co2, s again, the normal range of 35 to 45 mills per or millis of mercury. And I was sitting at a an anxious rest. So still at rest, but like.
[00:35:52] Performance is coming, I’m being measured and things like that. There’s always that performance anxiety that comes into it. But I was done at 18 and Oh wow. Yeah. And then so first of all, I had to figure out, why? Am I tense anywhere? And then so it’s okay, yeah, I’m, I’m being measured, I’m being watched.
[00:36:07] Wow. I observe myself. I’m actually, I’m tense and had to figure out why am I tense? And then so once I got rid of that, even then I only got into kind of the mid twenties. And at that point in time, you do some breath manipulation to try and increase your CO2 s and these are all the methods that, that you’ve seen out there.
[00:36:25] The Brian Mackenzie methods, the shift, and it shifted in adapta methods. And, all these things where you’re trying to do nasal breathing, you’re doing breath holds, you’re doing trying to take smaller breaths. You’re doing prolonged installations. All of these typical things that would try to increase your CO2 a little bit.
[00:36:42] Any one of those. I bumped my CO2 up into even 26, 27, and I felt this suffocation response. And when I did the tests of having higher co2, breathing in more co2, I just, it was one of those things I couldn’t. Because I had habituated myself to thinking that being in this low twenties was normal.
[00:37:03] And and then I started noticing once, once I start, over time, it took me like three or four months to be able to change this. And then I actually very slowly got up to where I learned that it was okay to be up at around 35. And so that’s where I’m at now. It’s stabilized at this low normal, and I still have the tendencies to drop it.
[00:37:21] I can recognize it, but when I get to the when it first started pushing up into those levels couple things happen. One, again, there’s that panic response, there’s that suffocation response where it’s oh my God, I’ve gotta breathe more. I have to, but even though my CO2 was at the low normal the other thing that I started noticing as I was allowed myself to get into this scenario, and we see this all the time in with this style of biofeedback, is that people start going, oh you know what?
[00:37:47] I actually noticed when my CO2 S drop that I get this tingling in my hands. What is that? And it’s something that they’ve had their whole life or they’re, ever since they developed this habit, whenever that happened, and once you start getting up into a normal range, you start seeing some symptoms that you didn’t really recognize cuz you habituated to those symptoms too.
[00:38:07] Start, they go away and it’s oh, this numbness that I, or this tingling that I had in my fingers when I get above whatever millimeters of mercury it is, I don’t get that anymore. And it’s super interesting because you know that this is exactly the type of thing that that I noticed and that the clients that I work with notice is oh, you hit a number and it’s 31.
[00:38:28] When I’m at 31 or lower, I get tingling or I get a headache or I get some blurry vision. Things that you just habituate and you think are normal and then you normalize your CO2 and they go away and it’s oh. Maybe I was supposed to be up at this level and, but it’s hard to get up there because you habituate to the lower CO2 s it it makes it a huge challenge and that suffocation response is real.
[00:38:53] Like you, it’s a primal response, so to, of a need to breathe. So it doesn’t feel good.
[00:38:59] Dr Mike T Nelson: Yeah. So would you agree that the way out of that then, paradoxically, is to expose yourself to slightly more and more CO2 to change the endpoint of the system that because your physiology is always survival based, right?
[00:39:16] So it says, okay, if I can’t handle an endpoint here, I’m gonna artificially squash you down lower so that you don’t ever get close to that endpoint that we don’t like at all. So paradoxically, the way around it, Is to slowly move that hard end point up, which kind of gives you more like physiologic headroom in which to operate so that your normal levels can rise back up to a better area.
[00:39:42] Is that correct?
[00:39:43] Dr Scotty Butcher: Totally right. Yeah, a hundred percent. I think that is the challenge. And again it’s, some people can do it with purely, purely biochemical aspects where you’re simply looking at changing the CO2 levels and you don’t have to tie in with any of the psychology piece.
[00:40:01] But I, in my experience and that of those that I’ve learned from is that that’s very rarely the case that more often than not, it’s the CO2 that drives that suffocation response. But it’s the habituation emotionally and psychologically that causes your body to go into that that threat mode.
[00:40:22] And. Yes, paradoxically, the way to get around that is to love, love this quote if for any physios out there that know a guy named Greg Layman, he’s a physio and Greg or No, from Canada, right? Yeah. He is. He’s from Ontario. He’s physio in Chi chiropractor and physio.
[00:40:37] Did his did his master’s under Stu McGill if I’m sure that’s a name that most people would recognize
[00:40:42] Dr Mike T Nelson: as well. Yeah. He came out years ago and had a bunch of stuff about core training and why it was bad and what was different. And I remember years ago I remember reading it, looking at him going, what?
[00:40:50] This guy’s an idiot. And I started reading it and looking at it and reading the references he had, and I was like, whoa. This is brilliant. Yeah,
[00:40:57] Dr Scotty Butcher: exactly. That’s usually how it goes. You push the needle on something and you’re crazy until it’s oh, wait a minute, maybe he’s not crazy.
[00:41:03] Yeah. But anyway, Greg is he and I don’t know if he originally this, but this is where I’ve consistently heard this from talking about he does a lot of work in pain and and movement related to pain science and that, and he talks about poking the bear, right? Yeah. And I, I don’t know where this analogy comes from, but it’s the idea is that you’ve got a bear in the cave and the bear’s blocking your way and you gotta get out.
[00:41:24] So what do you do? You don’t punch the bear in the face cause the bear wakes up and eats you. What you do is you just gently poke the bear and, not enough to wake it up, but enough to get it to shift a little bit. And maybe if you just gently poke it enough, you, it’ll shift enough that you can get your way out.
[00:41:41] I look at, and we use that a lot as physios. We use that a lot in in pain care, the, where you’re trying to do movement, where you just touch on a little bit of an increase in pain. And it’s exposure therapy really from the psychological perspective.
[00:41:53] Behavioral perspective is that we’re really exposing it’s exposure therapy. So really this is the same thing in my opinion, is that you touch on the CO2 levels where you start. Briefly, a little tiny bit to feel the urge to breathe. And then you keep practicing that and you keep working on that.
[00:42:11] And then very gradually you move the needle a little bit by, you poke the bear and it moves enough that eventually that level goes up. The key with that though, that most people don’t do when I’ve looked at a lot of the people that are doing a lot of the CO2 tolerance work is that they’re not stopping soon enough.
[00:42:30] I think that a lot of people will get people to push through panic and push through this suffocation response and try and desensitize it. That may work for some, but I think that for a lot of people that have some sort of emotional habit that they’ve developed around their breathing that has caused this to, to happen, that has caused the hypocapnia, chronic hypocapnia to happen is that you induce again, of course, as soon as you induce a suffocation or a fight or flight panic response, it’s that sympathetic activation, and so your body perceives that as threat.
[00:43:04] And so if your body’s gonna perceive that as threat, it’s gonna develop or reinforce that habit. That says, no, don’t go there. Don’t go there. So exposure therapy is good, but you’ve gotta be, I think you have to be a bit careful about how quickly you push into that. And so what we do in when I’m doing my biofeedback and the people that I’ve been working with is again, we pu we, we just poke the bear just a little bit, right?
[00:43:27] So it’s okay, go hold your breath just as long as you, you feel just an initial urge to breathe, but not a panic. And then you let it go and then you just keep pushing and see if you can move the needle that way. Same thing if you’re, you try, for anybody that’s never done nasal breathing during like basic exercise, like walking or whatever it’s that same sort of, if that’s the starting point I think for a lot of people is just, do nasal breathing and see, go to the point before you start feeling like, oh wait, I’m not breathing enough.
[00:43:54] Then just allow yourself to breathe however you want and then go back to it, right? And then just that repeated exposure without inducing that panic and suffocation response, I think is the way forward. And that’s the the experience that that I’ve had with the clients that I’ve worked with as well as those that that have taught me.
[00:44:09] Yeah.
[00:44:10] Dr Mike T Nelson: Yeah I, in the search and everything, I use the eustress/distress model, like all the time for everything, right? So tress EU stress, so stress you can generally recover from relatively fast because I think a lot of, like what you were saying is people assume even with exercise ah, I gotta, raise Mike men ghost from the grave and go, four sets beyond failure.
[00:44:31] And yeah, some people might get away with that, but I think the risks you run are a lot higher and it’s not needed. To me, it’s the interest example is crazy. Let’s say, you start lifting day one, I got crushed by the bar in high school, let’s say your max is 95 pounds for a one rm.
[00:44:48] You can go to the gym and do 75 pounds for maybe sets of four or five and do sets of that, and then 85 pounds for maybe two or three, and then you retest your max and oh my gosh, it’s a hundred or it’s 110, but. You never did the, you never did 95 pounds ever in, in training, right? So you have this transfer by doing, going up to it, coming back, going up to it, coming back, going up, coming back.
[00:45:16] That because of the adaptation your body gets, it’s like, uhoh, is idiots gonna go do this again? We better build in some more headroom. We better, change and get some of these positive adaptations because this guy seems to wanna keep doing this, so we better add capacity or we’re gonna be in a world of hurt.
[00:45:33] But it’s, to me, it’s just fascinating that you never went and you never even had to touch that thing specifically all the time either. Yeah.
[00:45:40] Dr Scotty Butcher: I love that and I love that analogy, Mike. It’s we, very true from a training perspective as it is from this perspective, the body really does a great job of adapting to eustress.
[00:45:51] I, I, I really see that in, in every aspect of what I’m doing. And, I come from, obviously as a physiotherapist, I’ve done a lot of research on strength training, which we haven’t really talked about, but that’s my bread and butter is around that. And, in, in rehab I look at I look at individuals that are going into doing strength training.
[00:46:08] And they’re trying to use these guidelines that are based on, say, the NSA’s guidelines, the rep ranges and percentage of rep maxes and things like that. Like the major flaw that a lot of that has is that they’re constantly assuming that you’re going at a hundred percent effort.
[00:46:25] That when you are done, you’re set you’re a 10, outta 10 for exertion. And most people, and especially in the rehab. You don’t want to be at a 10 outta 10 for exertion. No. Like you want to be in the eight, maybe nine range for the vast majority of what you’re doing.
[00:46:40] And as, as you said, you never touch that 95, but your body adapts to be able to do more after that. I don’t see this as any different. Absolutely. I see this as your body recognizing, oh, this idiot’s gonna try and push me up to a CO2 that wow, I don’t really want to be at. So I better adapt to that, and I better make it so that it’s okay to be up there.
[00:47:00] And then, that’s part of the again, the exposure therapy. So I guess I never really thought of strength training as exposure therapy physiologically, but I guess it really is the same sort of thing.
[00:47:08] Dr Mike T Nelson: Yeah. And last point on that is, if you go super hard into distress, sometimes you can have massive amount of pain, you can be injured, and then sometimes those systems, the gain gets changed to be so hyper aggressive.
[00:47:23] To prevent you from even getting remotely close again, like you’ve ever worked with people who’ve had like actual frank heat stroke, they become incredibly heat and tolerant almost like overnight. It’s Hey, you idiot, you pushed so hard that we’ve started literally shutting you down and you could have died.
[00:47:41] So now we’re, we, were gonna put this massive buffer zone in so that you don’t even get remotely close to that again. And so then you gotta go through the kind of exactly what you said, the eustress heat acclimation process over many months to try to rebuild that. So I think there’s a danger if you go too far into the distress too.
[00:48:00] Totally.
[00:48:01] Dr Scotty Butcher: Absolutely. And that’s the, that’s the smart thing that we say about, listen to your body. If your body is telling you don’t do it, maybe there’s a reason you shouldn’t do it. At least now, at this point in time for that reason. And the, again, that’s the.
[00:48:15] Punching the bear versus the poking the bear concept.
[00:48:17] Dr Mike T Nelson: Yeah. And where are you at for a time? Do you have to take off or where are you at? No, I’m good, so I know. No, I’m good. Whatever. All right, so I got about another 15, 20 minutes. So how this relates to HRV, which we’ll touch on and we’ll probably have to have you back on again cause this has been super fun.
[00:48:30] I get to ask all my super geeky questions. Nice. Awesome. This podcast is more about me than anybody else, so who cares?
[00:48:37] Dr Scotty Butcher: Why? It’s your podcast, man. You do what you want.
[00:48:40] Dr Mike T Nelson: Yeah, it’s why I don’t have any sponsors either. It’s eh, whatever. I don’t care if I piss someone off, whatever, it’s me. I don’t care.
[00:48:46] Yeah, that’s right. So the nice part about HRV is that it gives you a way of monitoring that response from the system, right? So we’re talking about CO2 tolerance, we’re talking about exercise, we’re talking about all these things. And to me, what I find the best about H R V is that everybody’s response is gonna be a little bit different.
[00:49:04] And yes, you can look at that with output and training and other stuff. But to me it’s just almost fascinating that you can figure out what the response of the body is, at least on the autonomic nervous system by doing a measurement, one time in the morning and then that allows you to figure out, oh, hey, maybe I did go a little bit too hard on that CO2 tolerance, or maybe my exercise intensity is too high, or my sleep is crap, or I’m not even enough calories, or, all these other stressors you can figure out where they’re at, which was what I find if you don’t have that information, it just takes you a lot longer to figure out what’s going on.
[00:49:44] Because a lot of people are not super in tune with their body, but I think you can learn that attunement a lot faster by having some feedback. It was like learning on any other skill, like if you wanna learn Olympic weightlifting, Yeah, get an in-person session with a coach who can tell you immediately, okay, that was good.
[00:50:03] That sucked. Do this. Instead of, having to even wait for video a couple days or a couple hours removed. Like the sooner you can get feedback to the process, you can iterate a lot faster. Yeah.
[00:50:15] Dr Scotty Butcher: To totally that is, that really is the process of this biofeedback that that I’ve really taken on as my sort of clinical skillset over the last little while is is that concept.
[00:50:27] The trick is of course, as is that you can’t just say, okay, my H R V is. I dunno, whatever. It’s, and again it’s relative to a, an established baseline, not a single number. Like you said earlier, it’s, you can’t just say oh, my h I v, is 24 milliseconds.
[00:50:43] What does that mean? That doesn’t mean any, yeah. What’s the context? Is it, are we talking about a trained person? We’re talking about someone who’s a little bit older, someone who’s younger, someone who has some sort of chronic disease, someone who has, some mental health disorder, someone like, it’s, you can’t just look at that.
[00:50:57] So you have to look at that baseline over, over at least a week, I think, as a a sort of relatively normal week where, there’s not too much extra stress in that. And then look at those changes. But even. Even looking at daily changes isn’t super relevant without the context of what the hell was going on.
[00:51:13] Yep. What were they eating? Did they eat late at night? Did they, what was their sleep like? When you look at all of these factors put together and that’s where it’s a great tool. It’s a great number to use. And I love, like I said, I’m, being a tech geek, I love numbers and I love getting data.
[00:51:28] And, but you have to pair it up with those subjective, what else is going on, kind of things. And to get that picture. So it’s, it is super interesting. What I really love about it from a biofeedback perspective is, you do that tracking, but what you can do is very acutely change that h r V level based on things like breathing and the way that you’re breathing or the stresses that you’re feeling.
[00:51:51] And so going back to some of the stuff you, that you asked me about when I presented in in Florida at neuro Sports is looking at acute changes in H R V based on exhibiting different stress responses or relaxation responses or meditative responses in that. And so you can, depending on what H R V metric you use, you can definitely see some changes as you induce either a stressor or say a breathing intervention that would trying to optimize or maximize the H R V response.
[00:52:21] And you can acutely see that go up and down and it’s immediate. It’s a very fast response, which is super interesting. But it also then relates to, okay, what was your, how did you collect your baseline measures? So if you’re looking at baseline measures over a week, as you said, it needs to be under really controlled scenarios and situations to be right.
[00:52:39] Cuz even if you just change your breathing, that’s gonna change your H R V number significantly, even if you’ve done nothing else. It’s a it’s good, but it, again, it has to be within the context of what’s going on. Yeah. Do you wanna explain
[00:52:52] Dr Mike T Nelson: a little bit about that in terms of how breathing can change H R V?
[00:52:56] So the app, I use full disclosures through athlete. I don’t really make any money from them, but they’ve been super awesome. I’ve used them for a long time. I’ve got a heart rate variability course. They’ve designed with them and one of the things they do on their app is they’ve got a little circle that goes out and goes in.
[00:53:11] So when you do it, they do something called paste breathing. So you’re breathing at the exact same rate. So every time you do the measurement, your breathing is the same. And because your breathing is the same, it doesn’t really factor into the H R V analysis. And you’ve got other groups that are like you’re adding this artificial parameter to it.
[00:53:30] So you’re not saying that the true underlying H R V because breathing can affect it. So you wanna explain just at a basic level, what is R S A, respiratory sinus arrhythmia sounds bad. And how breathing can acutely change. H R V.
[00:53:44] Dr Scotty Butcher: Yeah. Great. Great question. Super important as well. I will explain that to answer your question, but just to comment on the, the pacing when you’re doing your baseline.
[00:53:53] I love the concept. I really love it. And I think that is a very important aspect because like I mentioned before, you will, and I’ll, as I’ll explain, you will see significant differences, especially when you transition from a normal range of 12 breaths a minute, up to 18 ish, within that range, down to below eight.
[00:54:13] And so when you get in those level of changes that’ll happen. It might even happen even just with saying, Hey, just, I’m gonna take your measurement. I just want you to lay down and relax. I never tell people to do that when I’m measuring H R V, because as soon as you say, lay down, There’s a connotation of rest.
[00:54:28] As soon as you say relax, people then do things that they find relaxing, and often that is changing breathing rate down to a lower breathing rate. So that completely changes the H R V. So I like the concept of pacing, but the only comment I wanted to make on that it relates back to what we were talking about before with over-breathing and.
[00:54:47] There When we think of ventilation, of course there’s two components. There’s one, there’s the rate or the pace of breathing, but then there’s the depth. And so what you’re not controlling when you’re controlling the pace is the depth. So I love the concept of controlling the pace. I think that people need to be very careful when they do that, though, that they don’t then take excessive breaths in terms of the size of the breaths because then your ventilation is an over breath.
[00:55:11] You drop your CO2 s that becomes a stressor response. And any sort of a distress style of response that you’d see there is going to impact your H R V. So I think it’s, you have to look at it as, okay, sure. Pace your breathing, but your breaths need to be really normal breaths, and it’s hard to, it’s hard to know what that is without actually measuring it.
[00:55:31] But but that is one of the, I think, one of the flaws of that approach. Having said that, I do agree with you that’s better doing that and just trying to have these easy breaths where you’re, the instructions aren’t, take a breath in or control your breath. It’s about just allow the. So it’s just differences in the way that you approach things and the way that you say them. But but anyway so I, but I do like that and I do controlling the pace with with doing my baseline measurements for sure. Now rsa, so the respiratory sinus arrhythmia, again, arrhythmia, as you said, sounds different or sounds bad.
[00:56:02] When you go to the hospital cuz you’re having chest pain and they say you have an arrhythmia, not a good thing. This sort of arrhythmia is a good thing. It’s basically saying that your heart rate for, is not a metronome. And it’s basically saying that you shouldn’t have the exact beat to beat differences that is exactly the same across, your, across a minute’s worth or whatever of of time that you do want fluctuations.
[00:56:25] And that is a good thing and it’s representative of a healthy. Autonomic nervous system that is resilient to changes. And it’s a really good reflection of that. And so heart rate variability has multiple components as we know. One of them is related to something that’s called a barrel reflex.
[00:56:45] And it’s basically the reflex that happens in your in. Your art arterial and venous systems, mostly the arterial systems where what you’re doing is you’re measuring the beat to beat changes in your blood pressure and in order to maintain both blood pressure and cardiac output, when you have an in a small increase in blood pressure because of a s a beat of your heart, then that changes obviously the pressure inside the inside your arteries and your aorta.
[00:57:13] And so what happens is that pressure goes up, your heart rate goes down to compensate for it, right? So that you have this sort of, Fluctuation that happens where your barrel reflex goes allows your blood pressure to go up, your heart rate goes down, and then it reverses your blood pressure goes down, your heart rate goes up, and this cycle averages out at about 10 seconds.
[00:57:32] And to go through that full cycle. And so we look at that as a, the barrel reflex timing of of the changes in heart rate. And so if you were just to look at the barrel reflex, we would see that your heart rate variability would change significantly across that 10 or your heart rate would change significantly across that 10 seconds.
[00:57:50] Now what respiratory. Sinus arrhythmia is the other main component of heart rate variability. And basically what that says to, to put this very simply is when you take a breath in, your heart rate goes up. When you take a breath out, your heart rate goes down. Lots of reasons for that. We don’t need to get into the nitty gritties of the physiology, but it does relate to cardiac output and the pressures on the ventricles of the heart and things like that with different in inspiratory or expiratory pressures.
[00:58:16] But basically that’s what we’re talking about is when you breathe in, your heart rate goes up. When you breathe out, your heart rate goes down. And so we tend to look at it from a very simplistic perspective in saying that your increase in heart rate with an inspiration tends to be more sympathetically dominant, whereas the decrease in heart rate with an expiration tends to be more parasympathetically mediated.
[00:58:40] Although there’s lots of complexity there, it’s, but that’s the, that’s what we tend to think about it. So the idea is that, If you are trying to. Enhance your parasympathetic or your vagal drive or going to the Vagus Nerve Gym, or the Mind Gym is my my one of my H R V mentors, Jay Wiles from Haunting.
[00:58:59] Oh, yeah. Yeah. He he talks about the mind gym a lot and so going to the Mind Gym, what we’re trying to do is we’re trying to strengthen the functional connectivity in the brain to allow that vagus nerve to respond better, to respond faster, to respond more appropriately to the different stressors that are coming on.
[00:59:17] And so this is where we try and do these prolonged exhalations. You see this a lot in practice where people are doing things that involve a prolonged exhalation with the idea of basically saying that’s training the vagus nerve. And so that’s the concept behind what we’re talking about.
[00:59:34] A lot of these breathing techniques are designed to really do that. But we do have to think that, again, the parasympathetic system is good and having a good responsive parasympathetic system is important. But I always get caught when people start saying, or I get caught up when people start saying it’s all about the parasympathetic system.
[00:59:51] It’s no dummy we have a par, we have a sympathetic system for a reason. Like your heart rate needs to go up in periods of stress, in periods of eustress or distress. It needs to increase. You need to have that fight or flight response. Or we’re not gonna be able to run away from the bear.
[01:00:05] It’s one of these things
[01:00:07] Dr Mike T Nelson: Block, go ahead. Blockers feel like people on beta blockers feel like just absolute crap. Yep. Massive parasympathetic increases on beta blockers. Cuz that’s happened to me a couple times where clients haven’t told me and I’m like, what the hell did you do?
[01:00:18] I went to my dock and I got, they put me on a beta blocker. How do you feel? I feel horrible. I feel tired all the time. Yeah. Look at parasympathetic overreaching or over-training frank, over-training syndrome. Like super high levels of parasympathetic activity and people feel like
[01:00:33] Dr Scotty Butcher: trash. Yep.
[01:00:34] Yeah. And that yeah, very much there’s, and there’s really some interesting stuff about sympathetic outflow when you’re in a state of distress. Where sympathetic outflow, the, actually the change in sympathetic out. Is that a chronically high level, but you don’t get, you can’t ever reach maximum.
[01:00:51] Where people have taken pt there, there’s some research that I remember reading on P T S D. So women with P T S D were they were doing some sort of a exercise task. I can’t remember exactly what it was, but it was like some sort of a muscle contraction task. And they were looking at the muscle sympathetic nerve activation and and the responses.
[01:01:10] And they had this high level of sympathetic activation, but they couldn’t actually push into where they needed to be. So they actually had a reduced total sympathetic. So it’s when you get into. When you start looking at H R V and responsiveness and whether you have a healthy autonomic nervous system and a responsive or resilient nervous system it’s, you, you’re both your sympathetic and your parasympathetic systems need to be responsive, right?
[01:01:35] So you want sympathetic system to increase, but then when the stress is gone, you also want it to decrease, and you want the parasympathetic system active. So you want within what polyvagal theory would call a window of tolerance. For your nervous system, for your autonomic nervous system where you can fluctuate within your day at a normal level where you know, you’re at a really good baseline you’re not under any real stress, but then when you are under stress, you go up to match the need and then you come back down when the, when you don’t need it anymore.
[01:02:06] The problem is that like our lives are not based on that these days, with so many different things around sedentary and around all the technology and the dopamine little dopamine blitzes of scrolling through through your Facebook or your Instagram or whatever it is and being like chronically activated, right?
[01:02:26] So this chronic activation causes a stagnation, right? So it’s not just that, that we’re too sympathetic, right? We actually need to be more reactive in both systems. So anyway, that was a, long way we were, you originally asked me about R S A and sorry, I went do a lot of other stuff in there, but it’s all related, right?
[01:02:43] It’s all related to if you have a responsive nervous system, then your, you will respond better. Your heart rate variability, your heart rate will change more. Your heart rate variability will go up as these systems are
[01:02:56] Dr Mike T Nelson: more responsive. Yeah. I have a concept I haven’t talked a whole lot about, but I probably should again, as I just called it H D R human Dynamic Response.
[01:03:05] So how far on both ends of the spectrum can you go and how fast can you transition? So metabolic flexibility is a concept of H D R, human Dynamic response. You’ve got carbohydrates in one and fats another end, back and forth. You have your nervous system, whether you’ve got sympathetic, parasympathetic on the other side, you have muscle contraction.
[01:03:24] You have your bicep and your tricep, right? So it applies to these duality of systems, which appears to be how a lot of physiology is set up. Even like neurology, you’ve got sarcos, you’ve got antipsychotics, like the, it always seems to have these pairings and most of them end up being a two-way street.
[01:03:42] And on almost every scenario it’s like, how far can you go to one end? How far can you safely go to the other end? And how fast can you go back and forth
[01:03:49] Dr Scotty Butcher: as needed? Yeah, totally. Yeah. And that’s so true of multiple physiological systems. Yes. And really just human systems, right? Is, is the ability to react when needed as appropriate, not overreact, not underreact, react appropriately, and then come back down to react to the fact that you’re not under that stress anymore. And that, what’s really clear to me as I guess a a sort of summarizing message is that it isn’t just about the physiology, right?
[01:04:16] It’s about the whole human experience of the psychology and we, and emotional responses. And I haven’t even touched on which I don’t usually touch on the spirituality piece of it as well, but there’s also that comes into the holistic human response. So yeah, flex that flexibility.
[01:04:31] You’re, you’ve really done a good job of coining those those phrases and metabolic and physiological flexibility, cuz it’s really, I think that’s what it’s about. So I totally agree with you there.
[01:04:42] Dr Mike T Nelson: Thank you. As we wrap up, like for people who don’t have access to your clinic, don’t have a lot of, technology, what would be some tips you would give them based on your work on biofeedback and working with a lot of clients that I find most people need to down-regulate first to try to get some range into the system.
[01:05:02] I don’t know if you’d agree with that, judging by your head Nodding, I’d say yes. Yep, totally. What would be like some of your top, like two tips for people listening to, to do that, that you found have been pretty efficacious and let’s assume they don’t have any technology to really use.
[01:05:17] Dr Scotty Butcher: So assuming that they don’t have a smartphone, which is like a pretty shitty reception but let’s assume that anyway.
[01:05:22] Yeah. That’s fine. Yeah. Or the, maybe they do, but they’re just not willing
[01:05:25] Dr Mike T Nelson: or warning or they need some time away from their phone too. Sure. Totally. Yeah.
[01:05:29] Dr Scotty Butcher: So this is a bit of a loaded question because my short answer in terms of top tips is, Get some sleep.
[01:05:38] Look at your sleep hygiene. Are you being physically active? And is your diet not that you’re eating like an asshole, yeah, totally. Those are three but really like top end things in terms of physiological and mental flexibility and having heart rate variability be higher and having this autonomic nervous system being reactive based on what we know in the literature.
[01:06:01] Those are three of the top things that you can do. So when I’m working with clients, I, you have to address those. You can’t ignore them Now, The problem with that is everybody knows that. Everybody knows, oh shit, I should be sleeping better. I need to be eating better. I need to be exercising more.
[01:06:16] So it’s yeah, you can say that and you can give, try and give them the skills to do that. And that’s, I have a new program on stress resilience for healthcare professionals. That’s nice. A mentorship program that’s gonna be re released in about I’m hoping in about three weeks.
[01:06:29] Where we really go into that and I try and provide some support to do that. But, like I said, it’s not new news for anybody. The added piece from a biofeedback perspective is you actually don’t need. Tech to do quality biofeedback. What you have to do is you have to learn to tune into your body.
[01:06:46] And so what I really recommend as a very first step I agree with you completely. Downregulation tends to be the hardest thing, but it’s also important to get out of the way before you start looking at how you reregulate or how you up, up-regulate in that. So that downregulation is super important, but in order to do that, especially if you don’t have tech, you really need to develop what’s called interoception.
[01:07:09] And that’s just the sense of looking inwards at what your body, how your body responds to varying stimuli, varying situations. And one of the easiest, best way best ways to do this is through learning mindfulness meditation and that sort of thing. And not I understand fully that many of your listeners are probably like, oh, you just said mindfulness.
[01:07:29] That’s air fairy crap. I, I used to think that way too until I actually looked at what happens physiologically and anatomically when you do mindfulness, it is not, I’m just thinking better. You actually change your body, you change your physiology by doing that. But one of the easiest ways to do that, and even if you don’t wanna call it mindfulness and you don’t wanna call meditation or whatever, just tune into how it feels to breathe.
[01:07:54] Simple, easy. Like just you don’t think about meditation. Just find a place where you can chill you’re comfortable and you can chill. And then just what does it feel like to breathe? And then just tune into your breath. And that’s really all that you have to do. If you find yourself then thinking about something else, just come back to your breath, right?
[01:08:10] And then just really thinking about that. And then you can change it. Meet. So one day you do your breath, and then another day you can I feel my heart rate? What’s my heart rate doing? Focus on the heart rate each beat, right? And then when you find yourself thinking about something else totally normal, just come back and rethink about it and just do that.
[01:08:25] Build up your tolerance for that. I find that as an initial step is crucial before you do really any of the other deep work. The second, so that would be the first piece. The second piece would be just work on some slow breathing. Slow. Let your breath. So again, I don’t wanna say relaxed because I don’t want you to think relaxation with this.
[01:08:47] This isn’t about necessarily relaxation, it’s about trying to allow the breath to happen at a slower pace. And so you might use a pacer, but again, that uses tax. So re really all you need to do is think about, take a slow count of four or five in and a slow count of, let’s say six or seven out, something along those lines.
[01:09:07] Just prolong that exhalation. Do it a little bit slower allow that breath to happen. Don’t be so caught up at what the exact pace is. You’re, again, you’re not forcing the breath. You shouldn’t hear your breath. It should be just nice and easy. And then you can combine those two things. The focus on the breath with the slower, easier breath.
[01:09:24] If you’re looking at a down regulatory practice that doesn’t require tech, that’s about as simple as it gets.
[01:09:30] Dr Mike T Nelson: Cool. That’s awesome. And that matches a lot of I did a Zen meditation retreat several years ago in Costa Rica, so shout out to Dr. Ben House’s dad, Mr. Kim. And we get there.
[01:09:42] And I’d never done anything like that before. I’m like, oh, this’ll be fun. The perfect location, great teacher. And so we get there, it’s day one. He’s okay. So we’re all excited. We’re like, what do we do? He’s okay, here’s the position you sit in. Find a nice soft gaze in front of you, and if thoughts come in, just let them go.
[01:10:00] Okay. Practice. And I’m like, is that it? Is there anything else? He’s no, that’s it. Now do, yeah. I’m like, how long do we do this? He’s we’ll do this a lot for several days. And then you do it for years and decades. Yeah, that’s it. Yeah,
[01:10:17] Dr Scotty Butcher: that’s right. And it’s so simple, right?
[01:10:20] And again, like for those of us that are like, really geeky into data and shit like that, ju it’s what the fuck am I doing? Yeah. I’m not doing anything. But that is the point is that to basically teach yourself how to not be so engaged in all of these other things in the world so you can actually be engaged with yourself, which is, like you said earlier, people are so disconnected from their bodies that is the source of or one of the sources of many of the issues that we have now.
[01:10:47] So the learning how to do that, super important.
[01:10:50] Dr Mike T Nelson: Yeah. So last question in the last two minutes here. I hear you like some good music. What are some favorite bands you recommend? This, give
[01:10:57] Dr Scotty Butcher: you a whole show, but this could be a fantastic show. You know what, I’m really digging. So I’ve always been a Metallica fan.
[01:11:03] I’m really digging the new releases from their new album. It’s good album. Yeah, I like it so far. It’s really good. Yeah. Yeah. No I’m quite happy with it. I really liked a lot of the earlier not early, early releases. Yeah. But, the ones over the last decade or so that have come out, this one has a different feel to it, but it also harkens back to hardwired and some of the real hard rifts that they go into.
[01:11:23] My favorite song is oh shoot I’m forgetting the actual name of it. It’s If Temptation had a sun. Yes.
[01:11:29] Dr Mike T Nelson: I love that one. That’s my new favorite off the album so far.
[01:11:31] Dr Scotty Butcher: Yep. It’s totally my new favorite too. And I can’t wait for the full album to be released if you’re, when, depending on when you’re listening to this.
[01:11:37] Yeah. It’s prior to the release right now and there’s only four songs released. But yeah, loving it right now. You can’t go wrong with with any, five Fingers, slip, knot. What else am I listening to these days? I’m actually like some Vbe V beat’s pretty good. Yeah.
[01:11:50] Dr Mike T Nelson: I love the vocalist for Volbeat.
[01:11:51] He does just a very cool vocal style. That’s just I just, I like it.
[01:11:57] Dr Scotty Butcher: Yeah. And I appreciate you sent me over some links of the, some of the stuff you’re into and it’s oh yeah. I touch on the more death metal stuff a little bit, but I’m more into I’m more into the, more I guess the mainstream mainstream metal hard rock kind of stuff.
[01:12:09] So I’d say that’s what I’m, that’s what I’m digging these days.
[01:12:12] Dr Mike T Nelson: Yeah. Are you excited to see the Panera I wouldn’t say Reunion or whatever they’re calling it, I guess now what,
[01:12:18] Dr Scotty Butcher: whatever it is. Yeah, exactly. No, that’ll be awesome. Yeah, absolutely. I yep, I have my, my set of tickets for Metallica coming out the you had to buy them like four years, no, two years in advance.
[01:12:29] Yeah,
[01:12:29] Dr Mike T Nelson: it’s crazy. It’s 2 24 in fall, I think. And obviously Panera and Five Finger Death Punch are supporting on that.
[01:12:37] Dr Scotty Butcher: Totally. Yeah. No I’m super pumped about that. Einstein Kills is actually really good too. They’re yeah, they’ve got a different feel to them. They’re newer, but they’ve yeah, they’ve got a, they’ve got a different feel to it.
[01:12:45] And there’s one one other I was thinking of yeah. Anyway that, that’s most
[01:12:49] Dr Mike T Nelson: of it. Yeah. And I’m excited. I’ll be able to see Luna Shore Gojira in Mastodon in Minnesota actually live outside, which is gonna be pretty crazy in August. Oh, song. Oh, that’s awesome. Je I
[01:13:00] Dr Scotty Butcher: love Gojira. Gojira is yeah.
[01:13:02] Super
[01:13:03] Dr Mike T Nelson: cool. Yeah. Awesome. Where can people find more about you?
[01:13:06] Dr Scotty Butcher: Okay. Easiest way is on Instagram at the Strength Jedi. And we have not even talked about Star Wars. That’s my first Star Wars reference to this podcast. That is a travesty. That is blasphemy. Mike, we didn’t even hang up Star Wars again.
[01:13:23] Yeah, totally. We, cause we didn’t really even get into a lot of the H R V stuff too, so I’d love to, I’d love to come back and talk at more depth about a lot of that stuff. But yeah. And Star Wars too.
[01:13:31] Dr Mike T Nelson: You tell us all about Darth Vader’s breathing patterns.
[01:13:34] Dr Scotty Butcher: Yep, exactly. And how I think the force is related to interoception and it’s all to me, I’ve got it all connected in my head.
[01:13:42] So anyway, the Strength Jedi is where you can
[01:13:44] Dr Mike T Nelson: find me. Okay. And then website
[01:13:45] Dr Scotty Butcher: also website is actually my company is Mind Body strength.ca. Cool. But I have links to that on if you just remember the Strength Jedi, you can find the links there.
[01:13:56] Dr Mike T Nelson: Awesome. Thank you so much for all your time today.
[01:13:58] We’ll definitely have you back. I appreciate you answering all my crazy respiratory physiology questions and hopefully had some useful stuff for people out there too because it’s easy to get stuck in the weeds, but like you said at the end with just doesn’t have to be complicated when you actually do it, it can be extremely simple, even though there’s a lot of complexity under the surface.
[01:14:19] I don’t want that to scare anyone away from not doing anything. But I think if you’re especially a trainer or a coach or someone working in the field, you can understand some of the mechanisms. It allows you to get to better simple action items that people can do and get better results. So yeah, thank you so much for all your time.
[01:14:34] Really appreciate it.
[01:14:36] Dr Scotty Butcher: No problem at all. Thanks for the invite and yeah, happy to be on anytime. Yeah, this was super fun.
[01:14:41] Dr Mike T Nelson: Cool. Thanks again.
[01:14:44] [01:14:44] Ethan: Thank you so much for listening to the podcast today. Big thanks to Dr Scotty Butcher for being on the show and make sure to check out all of his great stuff in the links below. I appreciate your patience with the AI voice here as Dr Mike will be back talking again soon.





Leave A Comment