Join me on the Flex Diet Podcast as I sit down with the esteemed cardiologist Dr. Michael Twyman to tackle the vital subject of cardiovascular health and the power of early risk detection. We discuss the significance of functional testing and specific scans that could revolutionize your approach to heart disease prevention.
Listen in as Dr. Twyman shares his transformation from invasive to preventative cardiology and learn about the essential tests he recommends for gaining invaluable insights into your heart health.
For Dr. Twyman’s top 4 takeaways, go to https://miketnelson.com/flex4. Special thanks to Flex Diet Podcast sponsor LMNT. Choose LMNT for all your hydration needs. Check out https://drinklmnt.com/mikenelson.
Episode Chapters:
-
(0:00:00) – Cardiovascular Health and Early Detection
- (0:06:22) – Cardiovascular Risk and Plaque Development
- (0:12:37) – Understanding Heart Health and Cholesterol
- (0:19:13) – Understanding Lipoproteins and Cardiovascular Health
- (0:27:54) – Functional Testing for Arterial Health
- (0:36:32) – Nitric Oxide and Arterial Health
- (0:44:18) – Understanding the Calcium Score Test
- (0:50:34) – The Importance of Circadian Rhythms
- (1:00:47) – Optimal Red Light Therapy Parameters
Connect with Dr. Twyman:
Rock on!

Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
[00:00:00] Dr Mike T Nelson: What’s going on? It’s Dr. Mike T. Nelson here, back with the Flex Diet Podcast. And today on the program, we’re focusing a little bit more on the health component. I have cardiologist, Dr. Michael Twyman, and we talk all about the top things you need to do for cardiovascular health. Everything from the functional testing to blood work to Different types of scans and other things you should do to make sure that cardiovascular disease, which is still one of the top killers in at least the U.
[00:00:39] S., if not the world, that you’re doing everything you can to reduce that risk. And as a side note, that’ll also help your performance, too, because there’s a big overlap between those. You’ve probably seen some of the data looking at your aerobic capacity or VO2 max. in relation to a massive risk reduction in cardiovascular disease.
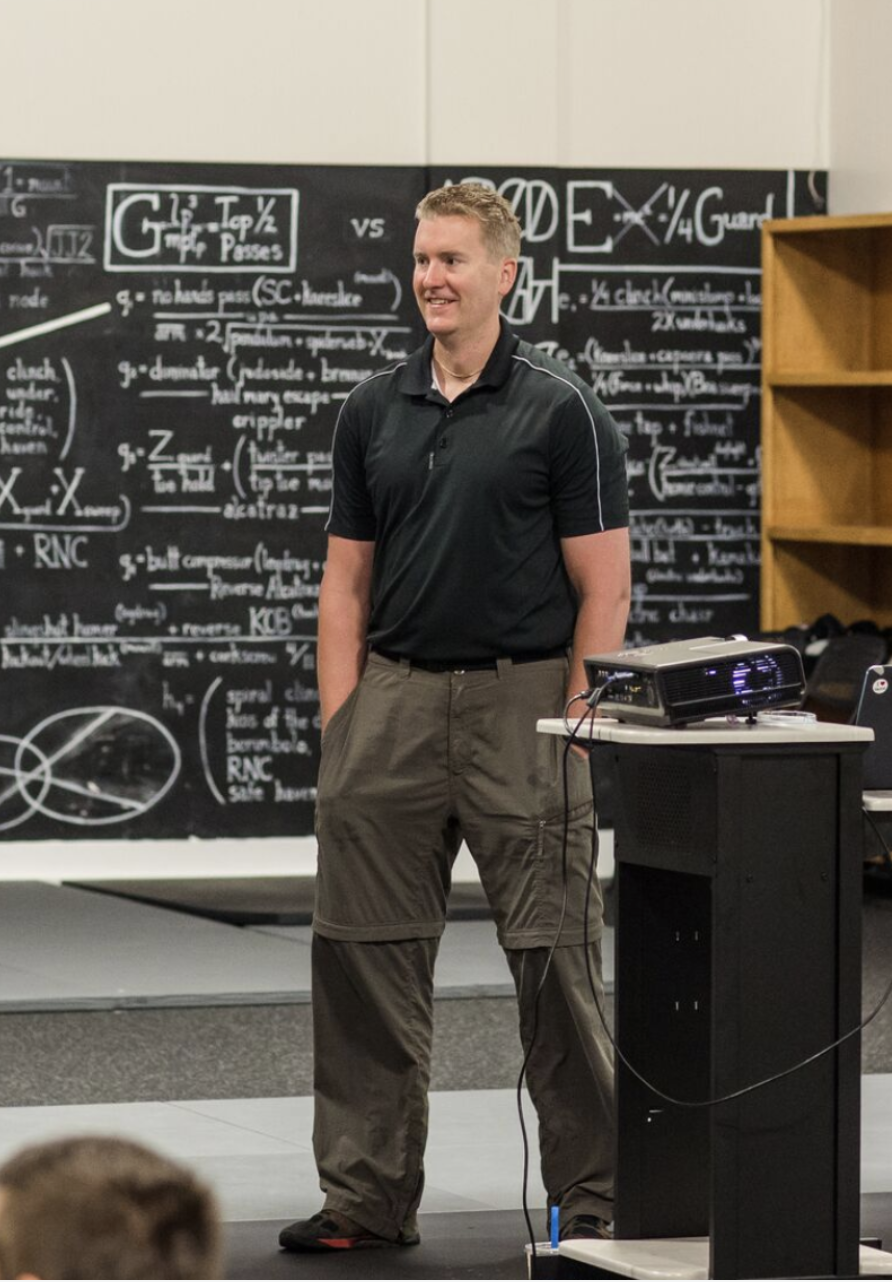
[00:01:04] So I first got to meet Dr. Twyman at the wonderful seminar that Alli Gilbert put on, the Silverback Summit, which was in Austin, Texas this past year. We got to go there. It was great. If you have the ability to go to Alli’s seminar coming up again this fall, the Silverback Summit. We’ll put a link in the show notes here, would highly encourage it was an awesome time, nothing to disclose.
[00:01:31] I don’t make any money off of the link or anything like that, but I would highly encourage you to go. So Dr. Twyman was there and I had to wrangle him on the podcast here, which he was kind enough to spend a bunch of time going over a functional testing such as similar to FMD or endopath to a whole bunch of other great stuff.
[00:01:52] So a lot of cardiologists I find are actually really good, but I was always been looking for someone who looks more at functional tests. So how is your body actually performing? Blood work and everything else is definitely extremely useful. But since my background is more in exercise phys, I always like to look at what is the current output of your body.
[00:02:13] And how do we know when we should be doing the right tests? to ensure that keeps working as best as possible for as long as possible. If you want to know his top four tests check out the flex four, go to miketnelson.com/flex4. At the end, I asked him what his top four tests would be to do, and you can get that exclusive information there.
[00:02:41] That also puts you on to the insider newsletter. So if you’re already on the newsletter, you will get those top four items. If you are not go there now and you will get instant access to them. Also, our other sponsor here is LMNT. We are still down here in Mexico as of the recording. We’ll be headed back home in just a day or so.
[00:03:05] So you may hear some random noises in the background here. And we brought a bunch of LMNT, which has been super nice to have. Especially when it’s been warmer here, being outside doing a lot of kiteboarding. One thing I realized with kiteboarding is spending time in the water, which is amazing.
[00:03:23] I forget how much I do actually sweat in the heat, because it’s hard to tell. And what I’ve realized is drinking more Element has made a huge difference to just overall performance, and then especially how well I feel afterwards with energy level. So it is Affiliate Link. I do make some coin off of it.
[00:03:42] So go to miketnelson.com/flex4 if you want the top four tests, Dr. Twyman would recommend, and then go to drinklmnt.com/mikenelson electrolyte drink. We’ll have both of those in the note section here of the podcast and enjoy this podcast all about cardiovascular health.
[00:04:12] [00:04:13] Dr Mike T Nelson: Welcome back to the Flex Diet Podcast and thank you very much for being here, Doc.
[00:04:17] I really appreciate it.
[00:04:18] Dr. Michael Twyman: Thank
[00:04:19] Dr Mike T Nelson: you for having me. Yeah, we got to see your wonderful talk at the Silverback Summit. So shout out to Ali for putting that together. That was great. I’m always curious, like, how did you get in contact with Ali and we’ll get into the topic talking about cardiovascular risk and a bunch of other stuff here.
[00:04:38] Sure,
[00:04:38] Dr. Michael Twyman: so my practice is focused on the early detection of atherosclerosis, and there’s a novel way to look at the coronary arteries called the CLEARLY scan, and HAlli was actually interested in that scan, and she reached out to us and said, could you help us get us that scan? So it was a mutual friend, Jim, that put us in contact.
[00:04:56] Dr Mike T Nelson: Oh, very cool. Awesome. And what made you go down the route of early prevention? Because I remember when I talked to you at the conference, I loved your talk. I thought it was great. We chatted for a while after. And I know a lot of you. I don’t want to say standard cardiologists, and there’s a lot of, good things you can do and exercise stress tests and we’ll get into all of that, but you’re like one of the first people I talked to that was actually trying to look at very early on detection and not when sort of stuff is already lack of a better word, broken.
[00:05:27] But what are the factors leading
[00:05:29] Dr. Michael Twyman: up to that? Yeah, I got interested in, preventive cardiology back in my original cardiovascular training. I was a invasive cardiologist for many years but always was interested in trying to get to the root cause of why these people develop plaque, because it was much more than just them having high blood pressure, high cholesterol, high blood sugar.
[00:05:50] Obesity. The same patients kept coming back and we thought we were treating all their risk factors, but then eventually discovered the world of functional medicine and then took the best of that. I eventually found kind of the biohackers and the health optimizers and took, that’s the circadian rhythm glasses come in and just pieced it together and said this is how the body really works.
[00:06:08] I’m much more interested in how to optimize it than treating it when it’s completely broken. That was worthwhile to help people when they’re having a heart attack in their time of need, but I thought there had to be a better way. And so I just got curious and just kept diving down those rabbit holes.
[00:06:20] Dr Mike T Nelson: Very cool. And so now your clinic is in St. Louis, correct me, and is primarily focused on early detection,
[00:06:27] Dr. Michael Twyman: correct? Correct. Yeah. My office is in St. Louis. We have patients from the local area, but, since I’ve been on this podcast circuit for the past couple of years, certain patients hear this and it resonates with them.
[00:06:36] And, we’ve had people as far as away from Hawaii, Canada, the Bahamas, they fly in to see us. And we use our novel non invasive test to look at the health of the arteries. We basically tell them are they aging faster than their biological age. And then, we can do some blood work drawn from our office.
[00:06:51] And then the follow up visits, we do telemedicine with them.
[00:06:55] Dr Mike T Nelson: Awesome. Yeah, we’ll definitely get into the testing that’s done, but for most people who aren’t familiar, I guess the two part question is, tell us a little bit about why they should care in terms of overall cardiovascular risk, especially if, people listening to this audience are generally a little bit more on the healthy spectrum already, doing some exercise, trying to eat well.
[00:07:16] And the follow up question is, which may tie into it is a little bit about what exactly is plaque and how does it develop and why is that associated with
[00:07:25] Dr. Michael Twyman: the risk factors? So the first one is, if you’re into exercise, that’s great. It’s the best anti aging drug that you’re going to be able to ever take.
[00:07:34] Vascular disease is still the number one thing that takes people out earlier than probably they’re ready to. And so just because you exercise does not mean necessarily that your cardiovascular system is completely healthy. So this is that analogy of test, don’t guess, which we’ll get into. Approximately every 40 seconds, somebody dies of a heart attack, and just because you look fit on the outside doesn’t mean you necessarily so fit on the inside.
[00:07:56] What that means is it’s generally a plaque that ruptures when that happens. And plaque is, just think of it as blockages in the arteries develop over time and eventually one of those blockages ruptures like a pimple. And then
[00:08:10] Dr Mike T Nelson: they call it vulnerable
[00:08:11] Dr. Michael Twyman: plaque. Is that correct? Like the vulnerable plaques.
[00:08:14] Cause sometimes I talk about plaque, more like an iceberg. The majority of the plaques just going to be growing in your artery walls, asymptomatic for many years. You can’t feel it. But if the, the plaque grows big enough that starts occluding the lumen where the blood is flowing, then people might start having some exercise and do symptoms.
[00:08:29] They might have tightness in their chest, shortness of breath or, Hey, this exercise used to be easy. Now it’s really hard. I can’t do it anymore. They may have a fixed diagnosis or blockage in the artery that’s driving that. Those can be treated with medications, stents, and sometimes surgery, but it’s the non obstructive lesions that more than half the time actually cause the heart attack.
[00:08:49] And the scary thing is that oftentimes we have zero symptoms until one of those plaques ruptures. So that’s why you got to start looking for them before you start having symptoms.
[00:08:57] Dr Mike T Nelson: Yeah, which I always thought is Interesting because people I’ll say guys in general, don’t go to the hospital unless they’re just about ready to keel over.
[00:09:07] And, but yet we have lots of good data showing that it’s not necessarily how much of that lumen, that vessel is being occluded. It’s the fact that occlusion area, the plaque is not stable. So part of it just falls off and then it flows further downstream and just basically logs off a whole area and can destroy part of the muscle.
[00:09:28] Dr. Michael Twyman: Correct. Correct. And it’s like some of it’s the the distal thrombosis, but it’s also a local event. So again, think of like the plaques on your arteries is like little pimples. You have nearly 60, 000 miles of blood vessels. When you have a heart attack, it’s often just a very short area of the artery where the plaque ruptures.
[00:09:46] And then the interventionist goes in there and puts in a stent to prop open the artery, but they didn’t treat the rest of the 60, 000 miles of blood vessels. So if you never got to the root cause. It’s like a game of whack a mole. They may just keep developing other plaques along that lining of the artery.
[00:10:01] And the plaque, when it ruptures, the blood will clot, because basically the body thinks it’s bleeding to the outside. So platelets clump together. And that blocks all the blood flow downstream so the tissue downstream doesn’t get oxygen or nutrients and will start to die. But some of that kind of fibrous material and platelets, that does shower downstream and you have these distal emboli as well.
[00:10:22] Got it. So it’s
[00:10:23] Dr Mike T Nelson: actually both. It’s the area because the body is thinking, Oh my gosh, we have a I’m doing my air quotes here. Like a hole in the pipe. We gotta plug this. We gotta make sure that this doesn’t happen, but then that unfortunately causes blood flow issues further downstream from it too.
[00:10:40] And that probably explains why I worked for a cardiac device company for a while and I did an internship with a company that made stents. And so we would see patients that would come in, Multiple times like they get one stent and then a year later they get another one or we had a few cases where I remember talking to the one intervention cardiologist and I said what was the I was just observing cases and I said, Oh, what’s this guy in for?
[00:11:05] He’s ah, he gets a full metal jacket. I’m like, what’s that? He’s like multiple stents in a row. And he showed me You know the picture and you can just see it like three stents like pretty long ones lined up just over the course of just the whole vessel, but it was interesting, talking to a lot of those physicians and doctors and cardiologists that it seemed like once you got one cent, your odds of getting another stent were pretty high, which I thought was.
[00:11:30] Interesting. So it’s still almost like you were saying, an acute thing that you’re trying to go fix these little fires that just keep showing up, but you’re not getting to the root cause or the root source of why they keep
[00:11:42] showing
[00:11:42] Dr. Michael Twyman: up. Correct. And that’s the challenge is that like the, the hospital system, it’s really good for emergencies.
[00:11:49] Those guys are well trained. If you’re having a heart attack, that’s where you want to go. If you break your leg, you want the orthopedic surgeon, the trauma guys to put you back together. But the hospitals are not the greatest place to figure out how to live healthily or how to live well or how to prevent chronic disease.
[00:12:02] That’s not their model. And so while they can, treat the acute fire, they’re not so great at initially telling you like, Hey, you got to change your nutrition, your exercise, your stress, your sleep. And then, oh, there’s these 395 lab things that you could look at that maybe it’s genetic. Maybe you have lipoprotein A or you have APOE4.
[00:12:20] They just don’t have the time or the bandwidth to talk about that in those kind of acute care settings. And so that’s why you got to work with somebody who will look to get to the root cause, because, as you said otherwise you end up with full metal jackets. And, in that instance, if you’re having a heart attack, you absolutely want to stint.
[00:12:34] You want the stint to stop the heart attack. But if it’s not in the setting of a heart attack, the majority of stints, they may make your symptoms better. You may have less. exercise induced angina, shortness of breath, or exercise intolerance, but the stent does not make you live longer, and the stent absolutely doesn’t reduce your risk of having a heart attack.
[00:12:53] That’s the big myth that people think they got a stint and they’re good to go. They got new plumbing and whatever it doesn’t matter. It’s no, you now have to basically baby the stints. So the stint doesn’t become a problem by forming a clot inside the stent or scar tissue inside the stent. So since I often sometimes joke their band aids, they work, but you have to fix the underlying problem.
[00:13:11] Yeah. And that was one of the big
[00:13:12] Dr Mike T Nelson: issues in the one company I worked for was the restenosis rate. This is before drug eluting stents and different coatings and all that kind of stuff that you would put this foreign material in there and the body would have this reaction to it and over time it would start closing back down again.
[00:13:32] What is the, what are some of the reasons that black is being formed actually in the vessels itself? I would assume that this is more of a protective type response of the body or what is the kind of the
[00:13:45] Dr. Michael Twyman: gist of that. But the thought is that it always tends to start with some called endothelial dysfunction.
[00:13:51] So the lining of the arteries have a layer called the endothelium, and it’s one cell thick. If you were able to strip out the endothelium from your arteries, it would be approximately the surface area of six tennis courts. It’s a very large secretory organ. And one of the major things that the endothelium does is that basically acts as like an air traffic controller.
[00:14:10] It determines what stays in the lumen where the blood is flowing and what has access to the arterial wall underneath the endothelium. One of the things that the endothelium does is it releases a gas called nitric oxide. Nitric oxide is a very short lived gas, it’s actually a signaling molecule. Way to think about it is that nitric oxide dilates the arteries, so it keeps things flowing very well.
[00:14:33] But nitric oxide almost acts like a repellent. It prevents the cholesterol particles and other things that are floating through the blood from sticking to the artery in the first place. So if the endothelium, if it’s injured, and it’s often injured because there’s a top layer above it called the glycocalyx, it’s a protective gel coat.
[00:14:49] If those gel coats get damaged, then the underlying endothelium is getting damaged. And so it’s like having a Teflon surface that’s scratched up. Once I, and that’s due to infections, heavy metals, lipoproteins, there’s many things that can scratch up that coating, oxidative stress, inflammation.
[00:15:07] Then the lipoproteins, which are faring the cholesterol, the triglycerides through the blood vessels, they get retained in that artery wall, like Velcro, and then it kicks off this immune response. Much if you sprained your ankle and it gets red hot and swollen, the layer underneath intima, starts getting swollen.
[00:15:25] As the white blood cells come in and investigate what’s going on? Are we getting invaded by bacteria? And then the white blood cells start gobbling up these lipoproteins, and they get engulfed with all this cholesterol. And that’s basically like a baby plaque that starts to form these foam cells.
[00:15:39] If you stop doing the damage, the body will take care of that problem generally pretty easily. But if there’s still ongoing damage, And much like a pimple or a volcano, it just keeps growing and growing, and this can go over many years, and then boom, the plaque ruptures, or it’s not as the event.
[00:15:55] So you want to start looking at things that break your nitric oxide pathways. Do you have healthy endothelium? Often in my office, I talk about being like your force field. If you have your force field up, you’re probably not doing that much damage. But if your force field is down, you got to make some type of intervention.
[00:16:10] And you can start damaging this protective coating in your teens, 20s, but you generally don’t show up to a doctor, you start having symptoms. There’s things that you can be doing in the meantime to repair it. And that’s what our whole practice is focused on is trying to find it early enough that we can make a dent so that they don’t end up in the hospital in the middle of night.
[00:16:28] Getting a full metal jacket and
[00:16:31] Dr Mike T Nelson: because cholesterol is actually in the plaque, I assume that’s where the original thoughts of cholesterol is. My little air quotes here, bad because, Oh look, it’s in the plaque. So cholesterol itself must be bad and therefore, Ooh, we must eliminate in our food because that’s where it’s coming from.
[00:16:50] Dr. Michael Twyman: And then this was, in rabbits, that’s how it goes. The type of cholesterol that you get in your diet is not the same cholesterol for the most part that’s inside the plaques. The cholesterol that’s in your plaques was made in your body. It’s made in the liver for the most part.
[00:17:03] So cholesterol is not the boogeyman that was put into you to give you heart attacks. It’s in the response to this endothelial dysfunction, this maladaptive inflammatory response. Without cholesterol, you’re not going to be alive. You need your cholesterol to make your hormones, your bile acids.
[00:17:18] Your cell membranes, basically the outer shells of your cells, are all chock full of cholesterol. The problem is it’s the lipoproteins that ferry the cholesterol, is the problem. Cholesterol is this waxy molecule, and much like oil and vinegar, it’s just not going to float in your liquid blood, your plasma.
[00:17:34] So the liver makes these things called lipoproteins, and this is a video, I always use an example of a tennis ball. Oh, there we go, nice. The lipoproteins are spherical, so the cholesterol goes inside the tennis ball, the triglycerides. The fat soluble vitamins, these phospholipids, all these building blocks for the cells, the liver makes these and then they pump them out through the blood vessels.
[00:17:53] And if the blood vessels are healthy, no harm, no fault. This little particle goes to where it needs to go. So muscles or other organs, grab it, download it, take out what it needs, ships it back to the liver and the liver does the reverse process, grabs it, gets out circulation. And then the way the cholesterol leaves the body when it’s done, it goes out the GI system.
[00:18:12] So if your arteries are healthy, the cholesterol is not the problem. But if you have endothelial dysfunction and these lipoproteins get retained in the artery wall, like Velcro. Then the cholesterol is going to get trapped there, like flypaper, and that cholesterol is irritating to the artery lining, and this kicks off this immune response.
[00:18:32] It’s not a perfect analogy, but it’s like having a splinter. If you have a splinter in your toe, it’s going to turn red, hot, and pus starts developing around it. That’s the way to think about like cholesterol getting stuck in the wrong place.
[00:18:43] Dr Mike T Nelson: And you want to talk a little bit, you mentioned lipoproteins, like what, we talked a little bit about what is a lipoprotein, but what are some things like on a blood test?
[00:18:52] Because we can have a blood test that’ll tell us different levels of these lipoproteins. And what should people be asking their doc about when they have some. Some even basic to even more advanced testing done.
[00:19:03] Dr. Michael Twyman: And that’s a great question is that I know sometimes this gets complicated quick, but I’ll try to simplify this.
[00:19:10] Yeah. Yeah. Most people, if they’ve heard of cholesterol and they’ve had their labs checked, they’re going to be used to seeing something called, your total cholesterol, your HDL cholesterol, your triglycerides. And there’s usually an LDL that’s calculated. Rarely is the LDL actually measured. The cholesterol, again, is just like the passenger.
[00:19:28] So you need to actually measure what’s transporting the cholesterol through the system, and that’s called the lipoproteins. And there’s a couple of different ways to do that. NMR is probably the most popular one. And there’s a few others. NMR or
[00:19:39] Dr Mike T Nelson: VAP test, I think, are the main two. The VAP
[00:19:41] Dr. Michael Twyman: used to be the old one.
[00:19:42] Used to be the old one. Okay. Yeah, there’s a. There’s an ion mobility that Quest does. So there’s a couple different technologies that measure the actual lipoproteins. Basically, how many tennis balls do you have floating around in your blood vessels at any one time? And the names tells you it, like there’s LDL particles, there’s HDL particles, so low density or high density lipoproteins.
[00:20:06] Kind of a dispelled myth, there is no such thing as good cholesterol. There’s no such thing as bad cholesterol. Cholesterol is just cholesterol, but there’s different lipoproteins that vary the cholesterol. And it’s the LDL particles that are the ones that will more likely get retained in the artery wall.
[00:20:22] So if you’re looking at an NMR profile, you’re going to see a number called LDL P as in particle. Typically most labs you generally want that number to be under 1000. On the outside of the lipoproteins, there’s something called apolipoprotein B or APO B like beta. APO B is, based on a tennis ball analogy, it’s going to be the white stripe on the tennis ball that holds this thing together in a sphere, and APO B acts as a key, finds these different receptors.
[00:20:55] And basically, then like a lock and key, you can open the door and get in. ApoB is on all the particles that basically could get stuck to the artery wall and get retained in that intimal lining. So most of them are going to be on your LDL particles, but some people have high levels of VLDL, tends to be more the diabetics or people have a real major issue with their triglycerides.
[00:21:17] ILDL is rarely high in people, but in 20 percent of the population, LPLA. Lipoprotein a, that is a genetically inherited lipoprotein, increases the risk of vascular disease by about double because it’s a lipoprotein that has like an extra protein on the outside of it. Think of it a little corkscrew.
[00:21:39] That just makes it a little bit easier to dive into the arterial wall. It also tends to make the blood clot more. And so ApoB is on the outside of that as well. Back to the making it as simple as possible. You would like to see the full NMR panel. But if you could only check one thing other than your traditional lipid panel, I would like to see the ApoB.
[00:21:59] Now there’s other things we would do, but if you have an ApoB that’s less than 70, 7 0, you’re relatively low risk. You’re not going to have some major genetic abnormality. But if you have an ApoB of 170, you probably have some genetic things that we’re going to take a look at. And then that kind of determines what is the best treatment strategy from there.
[00:22:18] Dr Mike T Nelson: Got it. And if someone were to look at just their standard cholesterol panel, the standard HDL, LDL, even triglycerides, what, any thoughts or recommendations on that? Because it, it seems like to me that’s The main screen and almost everyone has done and it seems like no one can really agree on what value it, it should be.
[00:22:43] I’ve seen, depending on what you look at, like from the ATP treatment panels, it seems like they keep pushing the numbers down lower and lower. Other people argue there isn’t much data for that. Other people argue LDL as it’s standardly measured, doesn’t matter. It’s your HDL or what are your thoughts on just.
[00:22:59] The standard panel and when would people want to know Oh boy, if you see this and this, like you, you definitely need to do some more digging and do some more investigative
[00:23:08] Dr. Michael Twyman: work. Sure. So if you’re looking at a traditional panel and your LDL cholesterol is greater than 190 milligrams per deciliter, and your total cholesterol is greater than 300 milligrams per deciliter, that’s the phenotype of familial hyperlipidemia or FH.
[00:23:25] Now, there are cases where if you’ve had more normal ish levels and then went on a low carb keto type diet, and now you have this type of pattern, you don’t necessarily have a genetic issue, but that doesn’t necessarily mean that is a healthy lipid profile, but it’s less likely if you had normal in your twenties and you change your diet in your forties and your lipids are that way, that it’s a major genetic abnormality.
[00:23:46] So I always ordered that. First, there’s a, a push that people want to do this, triglyceride and HDL ratio. And if the ratio is less than two, they’re metabolically healthy sometimes, but not always. And I wouldn’t hang my hat on that. Your arteries are healthy just because you have a lower triglyceride HDL ratio, but triglycerides, if you’re metabolically flexible, generally should be less than 80.
[00:24:11] You should be able to burn glucose pretty efficiently if you have a decent amount of muscle mass, but the HDL C, I don’t want to say it’s useless. But you have no idea what HDL is doing. HDL, one of its roles is to go into the artery walls and pull out cholesterol. Other roles of HDL is to work on the immune system.
[00:24:30] So if your HDL is high, is that good? Unknown. Because what if the HDL can’t get into your artery walls and actually clean up the plaque and you just have high levels in your blood? What if your HDL is low? The HDL has been going into your arteries and just working really hard and you don’t actually capture any HDLs when you’re drawing the blood.
[00:24:47] You have no idea. And if you’re sick, often the HL is going to be low because the HL is working for the immune system. If your HDL is really high, sometimes it’s because you have high myeloproxidase and inflammation, and then that inflammation keeps damaging the HDL particles, and your body has to keep pumping out more and more to replace them.
[00:25:04] So you have all these HDLs going around, but they’re not actually working or doing anything. So HDL shouldn’t be something that people really focus high on. Focus on the LDL particles and the ApoB side first, and then see what’s going on with HDL after you fix the things that are actually causative to atherosclerosis.
[00:25:22] Dr Mike T Nelson: No, I think that’s useful because I’ve seen Some cases where HDL is really high, LDL is borderline, triglycerides are borderline, and their physician’s Oh, their HDL is high, so they’re fine. I’m like, I’m not a physician, but I don’t know.
[00:25:39] Dr. Michael Twyman: Yeah. And it’s also back to the whole story is you have to look at the biophysical and the biochemical.
[00:25:43] Cause people would want to say I have low cholesterol. There’s no way I can have plaque. That’s not true at all. And there’s people who have plaque. that have normal cholesterol. There’s data, it’s older data, but half the time somebody comes into the hospital with a heart attack, they have quote, normal cholesterol panels.
[00:25:56] And so just one data point doesn’t necessarily put you at ease. You want to look at the arteries themselves. You want to see, do you have endothelial dysfunction? Do you have inflammation in the arteries? Do you have soft plaque in the arteries? Do you have hard plaque in the arteries? If you do, you’re a higher risk than somebody who doesn’t have those things.
[00:26:14] Dr Mike T Nelson: Yeah. And that’s my next question is what testing do you recommend? Because I loved your talk was I guess one of the things that always bothered me was exactly what you said is that it seems to be in standard medicine is a wide scoping thing. You argue, you get some blood work done. And if you’re within the certain parameters, like you’re good, but my background is exercise physiology and I’m like, but I want to know what is the output of your body?
[00:26:38] Like what is the function? Yeah, things leading up to it, whatever that might be interesting that might tell us the mechanism, but what is like the physical output? And so that’s where I’ve always wondered about. Cardiovascular stuff, like what is the function of the vessel?
[00:26:52] Like we talked about there, I did some work doing flow mediated dilation. So trying to look at, vessel function. And whenever I talked to most cardiologists, they were like, eh, I don’t know. If your bloods are fine, this is good. I’m like, but don’t you do like functional testing? And they’re like, oh, you mean like a stress test?
[00:27:08] I’m like but don’t you want to know, like, how your vessels are working? To me, that seems like a very basic question, because we know, based on all other physiologic systems The biochemistry of it, or at least what we can look at, doesn’t always match up to the output or what is the function of the system.
[00:27:27] And at the end of the day, the system has a dysfunction that potentially causes a heart attack. So it wouldn’t, I don’t know, it seems to me like you’d want to look at the function.
[00:27:36] Dr. Michael Twyman: That’s definitely why our practice is set up the way it is. That’s, that was the question was like. Yeah, I was in the cath lab and, nine months, 12 months later, the same guy came back.
[00:27:45] Yeah. I thought we fixed this guy. You’re like, we didn’t fix him yet. And because we weren’t using the right tools or we weren’t looking at the right, answers or right questions, honestly. And most of the time, if you go see a cardiologist, you generally have symptoms. It’s rare that people will say I got nothing wrong.
[00:28:00] I didn’t want to make sure I had nothing wrong. And so if you show up to cardiologist, short of breath, have chest pain, they’re going to recommend a stress test. That’s an appropriate test. Yeah, you want to recreate their kind of workload to see can I have this chest pain and shortness of breath come out when I get the heart rate up to 170 just because you pass a stress test doesn’t necessarily tell you don’t have plaque in your arteries.
[00:28:19] If you don’t have a 70, 80 percent blockage in your artery, if your artery doesn’t look like this, for viewers watching it, you’re probably going to pass your stress test. If your artery, has these like little minor plaques that are like this one, you’re not going to feel that, but that’s still put you at risk of having a heart attack.
[00:28:37] So stress test, that’s abnormal. That’s good. Go, take them to cath lab and fix what you need to fix and try to make their symptoms better. Just because you pass a stress test, you need to go deeper. And that’s where you’re talking about this functional testing, the flow media annihilation or the endopath test.
[00:28:51] That looks at, that’s basically the real stress test what do your arteries do when, there’s this hemodynamic load can your body pump out nitric oxide when it needs it? And if you can pump out nitric oxide
[00:29:01] Dr Mike T Nelson: Yeah, explain what an endoped is, or FMD just in general for listeners.
[00:29:04] Dr. Michael Twyman: I’m definitely more familiar with the endoped, but it’s a similar concept to the Yeah, it’s the same idea. The endoped test is a non invasive test that looks at peripheral arterial tone. There’s probes that are on each of your fingertips. And it’s measuring the flow through the small blood vessels in your fingertips.
[00:29:20] One way to think about it is as the blood leaves your heart, it goes through these small vessels, the blood’s going to expand and contract the arteries, like a little accordion. So there’s a five minute warm up period that we’re monitoring your blood flow through each fingertip, and making sure that, there’s no glitches in the system.
[00:29:34] There’s a five minute occlusion period where we pump up the blood out your cuff on one of your arms higher than your systolic blood pressure, so the flow is temporarily stopped to that one side. It’s not dangerous, maybe a little bit uncomfortable. Your arm will generally fall asleep, like you get that pins and needles sensation in your hand, and then on the endopath, that arm with the finger probe will look like a flat line.
[00:29:54] The other arm keeps looking like a little seismograph going across the screen. After five minutes, you open up the stopcock, the blood’s going to rush back down into the arm, and as that blood rushes back down into the arm, You’re going to get what’s known as reactive hyperemia, that blood’s going to flow across the glycocalyx, the protective gel coating to the endothelium, the body’s oh, here comes a big slug of blood, let’s give some nitric oxide, the nitric oxide gets released, the smooth muscle and artery wall relaxes, and then the flow rushes back down into your hand and your hand wakes back up.
[00:30:25] And then the device calculates a score known as your reactive hyperemia index. It’s essentially, by percentage, how much can your arteries dilate when there’s a stressor. If your score is under 1. 68, you have endothelial dysfunction and bad arteries. Low nitric oxide availability, you’re more prone to developing plaque if you have high lipoproteins, high blood pressure, all the other things that continually damage the arteries.
[00:30:50] If your score is over 2. 1, your arteries double in size. That is normal, but optimal is three to four and it’s rare that people have a three to four unless they are exercising routinely. They’re eating high nitrate diets, which is mostly green leafy vegetables and beets. They’re outside in the sunlight and then they remove the things that break nitric oxide.
[00:31:10] So then a bad test is a great test to tell you like how healthy the arteries today in your arteries make nitric oxide today. And the FMD is very similar using ultrasound technology.
[00:31:20] Dr Mike T Nelson: Yeah, and what I love about it is that it’s literally a functional test of how well Under stress your vessel can dilate right because if listeners are thinking about If you have a vessel in your heart, and it has stress if it can dilate and it can open up great You don’t have a blood flow issue if it can’t then at some point you’re gonna run into more risks
[00:31:44] Dr. Michael Twyman: Sure.
[00:31:45] And, I actually just saw somebody earlier today in the office who had a heart attack last summer. They did an angiogram. They had some 15 percent blockages in the arteries. There was no obvious plaque rupture. So the person did not have a stent place at that time, but they still had mildly increased troponin levels.
[00:32:01] So that always used to be a mystery. People are like if you had a heart attack, but we can’t truly explain why, but it’s microvascular disease. It’s, they call it, classify as a type 2 myocardial infarction, supply demand mismatch. The coronary arteries are approximately 3 4 in diameter, but 99 percent of your blood flow goes through the microcirculation, and your microcirculation is very small.
[00:32:25] It’s reported that approximately 100 of these microvessels could fit inside the diameter of one human hair. Yeah,
[00:32:31] Dr Mike T Nelson: I think it’s like some are so small a red blood cell gets squished going through it. They
[00:32:35] Dr. Michael Twyman: gotta slide through it. And if that, microvessel is stiff, the red blood cells back up, and it takes a while for them to get through there.
[00:32:42] And so often it’s like a nitric oxide issue for these smaller blood vessels. And just because they don’t find a blockage big enough that they need to drop a stent in, It doesn’t mean that you don’t have a problem, you still have to prove the function of that person. And so we did the endopath test on this person after they had changed some stuff in their lifestyle with exercise and they’re doing this beetroot powder.
[00:33:02] They’re nitric oxide availability is good now. So basically think about like their force field was down last year, whatever they’ve been doing, force fields back up. They’re less likely to have that event happen in the future.
[00:33:13] Dr Mike T Nelson: And you find that supplementing with the beet root and nit the nitrate itself is
[00:33:20] Dr. Michael Twyman: beneficial.
[00:33:22] The beet root powders and the juices, it depends. It depends on the quality of ’em and how much nitrate is actually in it. Yeah. So I tend not to use a lot of ’em, but if people already come in on ’em and it’s working for them, I tend to leave ’em alone. But that is sometimes the challenge is that, there are a lot of, marketing claims for some of these nitric oxide promoters.
[00:33:40] . And if it’s. Yeah, just chock full of arginine and citrulline, your body’s not low in those amino acids. It’s more of an issue with this enzyme called endothelial nitric oxide synthase or ENOS. And after the age of 40, this enzyme just doesn’t work as well. And so you can throw all the arginine in the world at it or citrulline, and you’re not going to make more nitric oxide.
[00:34:01] You have to fix the underlying causes. And there are some products that can help do that. They’re either lozenges or capsules that can help the body make nitric oxide. And so often when I get that question, it’s X, Y, Z supplement, do I’m like, I don’t know for sure. Sometimes do these types of endopad testings or pulse wave velocity.
[00:34:18] And if the numbers are improving and your body seems to be making nitric oxide with that product. Yeah, buddy,
[00:34:25] Dr Mike T Nelson: man. I’ll. I’ll leave him nameless. You may not want this as a public conversation, but he did a lot of research on nitrates like many years ago, and they were trying to find a way of testing different products for how much actual nitrate was in it.
[00:34:39] And it was more complicated. It’s a little bit easier now, but he was saying that the variability in products was just astronomical from there was a handful that were pretty decent to some that. You would think would have a lot, had almost nothing. And it was very hard. There’s still not, in my opinion, a lot of good standardization on it from one product to the next.
[00:35:03] Dr. Michael Twyman: And that’s why you want to work with somebody who’s been doing this for a while in the field and has, no real kind of. A, let’s just say, dog in the fight, you don’t want to like have somebody who’s marketing it and promoting it that their device is abnormal.
[00:35:16] You have to buy their product, their
[00:35:17] Dr Mike T Nelson: clinic is sponsored by beet root Rs or whatever. .
[00:35:19] Dr. Michael Twyman: Yeah. It’s like you don’t want to, have that thing. So you gotta take your advice from somebody who’s doing this day in, day out and, and there’s a lot of these kind of like nitric oxide pump things that are in like a lot of these bodybuilder Yeah.
[00:35:29] Pre-workouts. Yeah. Most of them are probably harmless, but that’s not the type of product that you want to use if you actually have vascular disease.
[00:35:37] Dr Mike T Nelson: And you mentioned naloxone. Is that for a type of nitric oxide delivery or are you trying to change like the local microbiome in the mouth to get better conversion?
[00:35:48] Because for listeners. The nitrates are actually converted through the microbiome in the mouth. So again, buddy, mine doing a study on nitrate supplements. He was so worried that if people were using Listerine or mouthwashes that kill all of those little critters, you don’t have any conversion.
[00:36:07] And his study was hosed from the beginning. But even, the bodybuilding bros that use a lot of pump supplements, like on a couple of consults, I’ve been like. Do you use mouthwash by chance? Oh yeah. I’m like you may want to stop doing that. Cause you’re basically just counteracting each other.
[00:36:21] If there even was any effect of what
[00:36:23] Dr. Michael Twyman: you were doing. Correct. Yeah. So these lozenges are designed for people who already can’t make nitric oxide on their own. And so we’ll, when the dissolved nitric oxide is released. And then when you swallow it, it helps recouple that endothelial nitric oxide synthase enzyme.
[00:36:39] So the body’s natural production directly on the artery lining starts working again. But to your point, in normal situations, if you’re eating, a healthy dash Mediterranean type diet, that’s high in green leafy vegetables. If you’re using a ton of antiseptic mouthwash, you’re destroying all the good nitrate reducing bacteria in your saliva.
[00:37:02] You need that nitrate reducing bacteria in your saliva to break those products down into nitrites. And then when you swallow the nitrites into your stomach, you need stomach acid for these chemical reactions to happen that can ultimately lead to making more nitric oxide. So if you’re using antiseptic mouthwash and you’re on a proton pump inhibitor, the odds that you make good levels of nitric oxide are pretty slow.
[00:37:25] And so if you can’t come off those things for whatever reason, which that’s another story, You’re probably going to have to supplement with something that can give you nitric oxide.
[00:37:34] Dr Mike T Nelson: Yeah, and PPIs are very common now. A lot of the clients I work with, and I believe they were only ever approved for a period of weeks.
[00:37:43] So most of the time, I’m like, Hey, go back to your doc, ask him if we make some changes, we do some stuff, see if you can work with your doc, if you could. Titrate your way off them. A lot of times they can, sometimes they can’t. I know it’s more of a medical issue, but a lot of times it’s Oh yeah, they put me on it like a year and a half ago and said, never worry about it again.
[00:38:00] I’m like, they never mentioned it again. Like they’ve never asked you about your symptoms. They’ve never. And tried to, try to titrate your way off or anything like, Oh no, they just said, Oh, I’m fine. I’m like, Oh.
[00:38:11] Dr. Michael Twyman: And that’s a good point. Obviously this is not, direct medical advice.
[00:38:14] You work with the person who put you on it. The question always should be, how long am I on this for? Because you’re right. It was initially prescribed for people who would have H. pylori infections or ulcers. Usually around six weeks, eight weeks, not eight years. Yeah. Now if you’re on it eight years, if you have Barrett’s esophagus, you’ve had multiple peptic ulcers and near bleeding death episodes, maybe you’re going to be on these things forever, but that just means you’re going to need more support for your blood pressure, your nitric oxide pathway.
[00:38:39] Just understand that. And that’s okay. That’s the thing where, it’s a test, don’t guess philosophy is that if you have uncontrolled blood pressure, it might be your proton pump inhibitor. And if you can come off it, you don’t have to take so many blood pressure medication. And
[00:38:52] Dr Mike T Nelson: does that have to do with the connection of nitric oxide and nitrates and conversion then I would assume?
[00:38:57] That’s correct. Yes. Yeah, so I think that’s a good tip too because a lot of times people have multiple issues that are overlapping and just medical and even research tends to be very siloed of. Oh, you had this thing, so we do this, and then you had this, so we do this, but there’s a lot of, you’re dealing with one human organism that has a lot of overlap between different systems.
[00:39:21] Dr. Michael Twyman: And yeah, sometimes that’s the challenge too. And the hospital medicine is it is very siloed. Like people come in and we’re like, we’re gonna fix your heart. And that might put me in renal failure, but the nephrologist will deal with it if you’re going to renal failure yeah, that’s not a good way to you want to treat the whole person, obviously, you want to prevent all the problems in their 60, 000 mile blood vessels.
[00:39:40] So we
[00:39:40] Dr Mike T Nelson: have endopat would be one of them. What would be like the next sort of more functional test you would do or you guys do at your clinic there?
[00:39:47] Dr. Michael Twyman: So two of them would be one would be like, something like that would measure the pulse wave velocity. And the device we particularly use is called the max pulse.
[00:39:54] It’s a non invasive test that clips to your finger, and it’s looking at how fast the arteries expand and contract, a marker of elasticity or stiffness of the artery. An old fashioned way to do it, and you can do it at home, is just what is your systolic blood pressure? Now you won’t, the story is you gotta take your blood pressure in an accurate way, so ideally, no caffeine, no liquor, no nicotine on board, seated.
[00:40:22] Feet on the ground back, support it arm at heart level and resting for approximately five minutes before you check it. Because if you just run in, plop your arm down, check it, you’re probably going to be a little bit high because you’ve always surprised yes, your blood pressure goes up when you exercise, you obviously, you’ve done enough stress tests, blood pressure climb. It’s just you just don’t want them going to 220 systolic with their exercise. So you want to be at rest, and what is your true resting blood pressure? And your true resting blood pressure should ideally always be less than 120 over 80 millimeters of mercury.
[00:40:52] All ages now the risk starts increasing when it’s greater than 110 over 70 now We’re not recommending you take medicines to drive you down that low, but my usual blood pressure probably 105 over 65 I’m not taking any medications to lower that low I’m not dizzy or lightheaded or anything like that people are so concerned like my blood pressure seems too low If you’re dizzy, lightheaded, or yeah, you’ll know exercise, you’ll know.
[00:41:15] And then you back off on those things because maybe you’re exercising more. Maybe, you lost weight. Maybe you don’t need as many medicines. So yeah. Deprescribing is right in many instances, but just because your numbers are low and you’re asymptomatic doesn’t mean necessarily come off the medications per se.
[00:41:29] If you have normal blood pressure, you likely are going to have more elastic arteries and probably better endothelial function. So those are the functional test. And these are getting into imaging tests. They’re like, okay is there actually inflammation in the artery? And that test that we routinely do in people is called the carotid intimal medial thickness ultrasound, or CIMT, that’s looking for intimal thickening, which is a marker of inflammation.
[00:41:53] This is where you will be given a number known as your vascular age. So if you’re biologically 50, but your arteries are 70, you have a problem. That was Dr. Sindenham’s famous saying from the 1600s, a man is as old as his arteries. Artery age is higher than a biologic. You got work to do to cool that down.
[00:42:10] And yes, it is reversible, but you’ve got to get to the root cause of that to make that happen. And then, there’s some other things we’re starting to layer on. We just recently acquired some ABI equipment, so we can check things a little bit more novelly. It’s all wireless, so it’s a pretty cool device called the Smart ABI.
[00:42:26] What does ABI stand for? Ankle Brachial Index. Oh, it is. Okay, that’s what I was thinking, yeah. So just see if you have, flow issues to the lower extremities, because, people Rightfully or concerned, if they have issues in their heart or the carotid or men’s health, you have erection issues, like if you have one issue, one place, you probably have plaque elsewhere.
[00:42:44] So you go looking for it. And so if you look for kind of flow issues to the legs, that sometimes is a telltale sign that they have problems elsewhere. The quick sidebar. Just to be an
[00:42:53] Dr Mike T Nelson: indicator for PAD, right? Peripheral arterial
[00:42:55] Dr. Michael Twyman: disease. Correct. Correct. And that’s the main case for it is if people have.
[00:42:58] Claudication symptoms, which would be like , you’re walking. All of a sudden, like your legs start cramping up, you stop walking, the pain goes away. But every time you walk to the mailbox, you get the cramps. You may have a blockage in one of the arteries in your legs, but sometimes the telltale sign for guys is that they used to have a lot of hair on their toes or their shins, and all of a sudden all that hair is gone.
[00:43:16] That’s because the microcirculation to the hair follicles, oh, it’s dying off and the hair’s dying. If you’ve never had hair on your legs, that’s not a big issue but if you had real furry legs. That might be a sign that you need to get checked out. Very cool.
[00:43:32] Dr Mike T Nelson: And then also you had talk a little bit about like clearly and some of the calcium scans and some of the other on the imaging side that you guys do.
[00:43:41] Dr. Michael Twyman: So those are more for like patients generally to say over the age of 40. Okay, that
[00:43:46] Dr Mike T Nelson: was my next question is when you would start some of these tests.
[00:43:49] Dr. Michael Twyman: Pretty much the other ones are like probably 18 years old. You can start thinking about some of them, especially the functional endopath test, the blood pressure, the pulse wave, because if you can find somebody in the early twenties, you can really halt this stuff right when it’s starting.
[00:44:02] Now the carotid is probably not going to start becoming abnormal into your thirties. But the calcium score tests where I used to say 40, 45 is where I would start. I’ve started to see more and more people, in their mid thirties have significantly abnormal calcium scores. Wow. And the calcium score test for those that don’t know it, it’s a low dose CT scan that looks for calcium on the walls of your heart arteries.
[00:44:26] So calcium is supposed to be in your bones. If it’s in your arteries indicates that, the artery walls have been invaded by lipoproteins and this immune response kicked off your body form plaque. And as a repair mechanism, the body forms scar tissue to try to seal that plaque into the artery wall to prevent it from rupturing.
[00:44:43] And calcium is just one of those things when the plaques become more stable. So the more calcium that you have in your artery walls, the more plaques you have in your artery. And so a normal calcium score is zero, a score over 400 is high risk, a score over a thousand is very high risk. I recently saw a gentleman under the age of 40.
[00:45:04] With the score of nearly 1400, he’s already gotten a couple of stints and now we’re doing the deep dive to figure out why he developed so much plaque at such an early age. Yeah. It’s an unusual case for me. It’s one of those cases where it shows you like you’re never too young to start thinking about your vascular health.
[00:45:20] That’s the thing. It’s like you, if you have a strong family history, you might approach this a little bit sooner. It’s one of those things where you don’t want to wait until you’re like, Oh, I’m starting to have chest pain or, I’m 50 years old. Maybe I go get checked out. It’s not too late, but it’s a lot harder to undo the work at that point.
[00:45:36] But 40 ish is when the calcium score test is generally reasonable. But the reason I say it’s not always sufficient is because at 40, your calcium score really should still be zero. If you follow enough people, I’ve still seen people in their eighties with scores in zero, not common, but it’s almost a thought like at some point you’re going to pop positive.
[00:45:56] It’s just, you want it to be later in life. You don’t want to be 30, 40, 50 when the score is getting high. But the challenge with the calcium score test is that it does not see that soft plaque. And it tends to be more of the soft plaque or more immature plaque that’s prone to rupturing and causing the heart attacks.
[00:46:13] And so that’s where you need to layer on a technology that looks at the wall of the artery. So using a CT cornea angiogram, and then adding on this AI software clearly, you can actually quantify how much salt plaque is in the artery wall. And the difference is that it’s a test that requires an IV, so you get IV contrast to be able to fill the lumen so they can get better pictures and measure the degree of stenosis if there’s any blockages in the arteries.
[00:46:42] And the test does require more radiation absorbed than a calcium score. So that’s why it’s not a Test for everybody, especially not a test that you would continue to repeat because radiation, there’s always risk and benefits of being exposed to medical radiation. So that’s why I don’t think the clearly is the best test for everybody right off the bat.
[00:47:01] There’s some people in my family history. Yep. You should go do it. Other people was like, Nope, we’re already expected pretty low risk. Let’s just monitor this when you’re 45 or 50 years old. And if you’re someone like I’ll ask for myself, like I’ll be 50 next year. Other than basic blood work and basic EKGs, I haven’t had anything done.
[00:47:21] Dr Mike T Nelson: So in something like that case, would like a baseline of clearly in addition to the other tests be useful just to know where you’re at since I am a little bit on the older end of the spectrum?
[00:47:33] Dr. Michael Twyman: Yeah, you’re definitely still not too old to get these type of tests is the first time.
[00:47:38] And yes, generally between 45 and 50, you want to do some type of test that would actually look at your coronary arteries non invasively. So either a calcium score test, they’re a little bit more easily available in most cities clearly is possible, but you got to work with somebody who can get that test ordered for you.
[00:47:53] And help you actually interpret it. That’s actually the biggest challenge is that, while it gives you a very nice printout, you need to know what to do with the information. So either one is reasonable. If your calcium score test is over 400 you’re a high risk person. The clearly test probably isn’t gonna be that useful to start treating that high risk person.
[00:48:09] But if the person has a calcium score of zero, and I’ve seen this many times, is that if you end up getting more clearly at some other later date, They will have not a high level, but they’ll generally have a small volume of soft plaque and you just never saw it on the calcium score and you’re like, okay, we’re going to need a little more aggressive with this person’s lipid management or their blood pressure, because they show that they’re more prone to laying down plaque in these situations.
[00:48:35] So what
[00:48:35] Dr Mike T Nelson: everything about from an algorithm would like a calcium scan, since it’s lower risk, lower costs would be the first thing to do. And depending upon what on that would determine if you want to look to do a clearly
[00:48:46] Dr. Michael Twyman: or not. That’s how I mostly will approach it. That, the calcium score test generally, at least in this region, it’s about 100, maybe it’s 300 and kind of some of the cities on the coast and then that clearly scan, depending where you’re at, it’s probably between 1500 and 2, 500 to do the test.
[00:49:04] And so just to get more people screened, the calcium score test is probably a quicker turn through like low risk bucket, medium bucket, high risk bucket. And then if then that low intermediate, then you can find out later yeah, this person probably should get it clearly because of they have LPLA or, they had a family history.
[00:49:20] Somebody had an event in their fifties. Let’s go looking for that salt plaque a little bit earlier. So I do tend to use that kind of algorithm in my head. There’s no standardized guidelines saying that this is how you would use a calcium score test versus the clear line. So
[00:49:32] Dr Mike T Nelson: if your calcium score is actually higher than you would be like, great, we found the thing we’re looking for.
[00:49:37] We know what’s going on. If it’s lower and you’re older in age, then it’s we know you don’t have like hard plaque, but maybe there’s some soft plaque going on that, obviously would not show up on that
[00:49:48] Dr. Michael Twyman: test. Correct. And then the other real good use case for it is when people would be on the fence of, considering taking lipid lowering therapies, particularly statins is that, I work with patients that, can’t tolerate them or just prefer not to take them.
[00:50:01] I’m like, okay, show me, let’s, I’m from Missouri. Show me show me what your arteries look like. And if they do a clearly scan and they got a significant amount of salt plaque in their arteries, You have that conversation like this didn’t get here by accident. So how would you like best to treat your lipoproteins at this point?
[00:50:15] Stans are one tool. And sometimes it’s okay, I see the plaque in my arteries. I understand why I’m taking this medication now. And so sometimes it helps with kind of medication compliance and also knowing that, if we start this treatment now, then repeat the scan in two, three, four years. And you can see, did that make a difference?
[00:50:30] Did that plaque shrink down taking that treatment?
[00:50:34] Dr Mike T Nelson: And correct me if I’m wrong, but I think One of the main mechanisms that statins work is that they actually are more anti inflammatory to the vessel and to some of those processes and not necessarily, yes, they lower cholesterol, but that’s not, correct me if I’m wrong, the primary mechanism of why they do provide some benefit.
[00:50:55] Dr. Michael Twyman: It’s a little bit debatable. It’s definitely no, I understand. I agree with every single point. Yeah. It might actually be the primary benefit is the lowering of the cholesterol in the liver and then you make less lipoproteins, but there’s definitely a component where it’s anti inflammatory.
[00:51:10] That was shown in the Jupiter trial with resuvastatin, that lowering CRP with resuvastatin. They had less carotid plaques. And it also helps the endothelium while it doesn’t necessarily make the endothelium Pump out more nitric oxide directly. It prevents the oxidative stress and inflammation that damages the endothelium.
[00:51:29] And then there’s some data that it helps shrink the soft plaque that’s inside these kind of like mixed plaques. So the top of the plaque will have a hard cap and the inside is like a gooey mix. The stands over time can help the cholesterol deposits shrink. And so the plaque will go from soft and more vulnerable.
[00:51:47] They’re more hard and stable. So this is one of the tricks too, is that if you get a calcium score test and you’re not on a stand, okay, fine. If you start a stand and then you repeat the calcium score test at any interval, you’ll often will see the calcium score test going up. And then the person thinks, Oh my God, I’m getting so much worse.
[00:52:06] You’re probably just taking all that salt plaque that you can’t see on the skin and you’re turning it into a more solid calcified plaque, which is more stable. Factor. And so you’re not necessarily getting worse. That’s actually what’s expected.
[00:52:20] Dr Mike T Nelson: That’s super interesting. And I remember I did some anatomy dissections.
[00:52:24] I’ve done a bunch of them, but they had one particular case where this lady had, I can’t remember what vessel it was, but it was completely calcified. And so we, dissected it out from the cadaver and we’re looking at it and you could literally thwack it on the table. And it was like a pipe.
[00:52:41] It was, cause I’d read about all this stuff and I had heard about it. I’m like yeah, whatever. But. To see that vessel was the segment of it was literally like as hard as a pipe and it was completely, I don’t know if it was completely closed or not, but it was pretty darn close.
[00:52:56] That was like Oh, wow. That’s crazy.
[00:52:59] Dr. Michael Twyman: That’s just shown you as the body has an amazing ability to try to heal itself. And it’s literally forming bone to try to seal these plaques. And interesting, like the artery lumen often will still be relatively open and the artery just gets bigger and bigger.
[00:53:15] And you are making, and so if they did an angiogram on this person, they would see some blockages, but it probably is not a 90 percent blockage in that artery. It’s probably like 30, 40%, but the artery is probably huge and it’s just a big chunk of calcium.
[00:53:31] Dr Mike T Nelson: Yeah. Which it always amazes me how the body is.
[00:53:34] Because I think sometimes especially with pathologies, we think oh, the body’s doing this horrible thing. It’s no, it’s literally, in almost every case I’ve seen, it’s literally trying to do everything it can to acutely survive. Now those may have long term costs associated with it, and you can run into issues 100%, but in the short term, it’s literally trying to solve the acute issue that could kill
[00:53:58] Dr. Michael Twyman: you.
[00:53:58] That’s a very good way to think about it. It’s the body is. Trying to get, out of the acute danger. It’s not necessarily thinking about longevity at all. I was just recently at a kind of a longevity focused vascular event a couple of months ago. And, the more that you really look at the data is in the early 1900s, infectious disease was still the number one thing taking most people out pretty much knock that down with antibiotics and such.
[00:54:22] And we forget about that, that was the biggest, scourge when our great grandparents were alive. But The average person still barely ever live past 40 years old, going to the past 100 years. And so the human body really is not designed to go 80, 90 years without a problem. And so that’s the kind of switch and pattern that you have to think about is this is a long time game. You’re going to get worse over time. It’s just how fast that going to be. And, traditional medicine is not necessarily geared for that. They’re there to help you during that emergency. They’re not there to set up that glide path where, that’s why I like going to the conferences that like Alli puts on at the silverback summit.
[00:55:00] It’s like people understand, you have to take care of the muscles so that your metabolism works well. You need your muscles for not only mobility, but it’s going to help you when you get injured. You got to break down the amino acids in the muscle to repair the damage. If you don’t have the muscles, it’s like you never saved for a retirement account.
[00:55:17] It’s going to be very hard to age well without money or muscles essentially. So that’s like the way I think about things right now is that like you have to look. At the end game, like you’re going to be on this earth 80, 90, 100 years. What do you need to do right now to be able to try to get there in the best status possible?
[00:55:34] Dr Mike T Nelson: Yeah. As we get close to wrapping up here, what are some things on the preventative side people can do? So if they’re listening to this podcast and they’re like, okay, maybe I need to eat more vegetables, like any. Like on your list from all your experience, like without knowing testing, obviously testing can narrow this down and have them be very specific, but what are some good just general habits they should be doing?
[00:55:59] Dr. Michael Twyman: So I typically talk about four pillars of health, there’s exercise and nutrition and everybody has their own opinions on that. And I can tell you they’re not important. They very much are, but the two other pillars that people sometimes really neglect is their stress management.
[00:56:12] You’re not going to lead a stress free life. You would not be alive without stress, but not everybody’s so great at dialing it back when they need to dial it back. So doing something that trains your vagal tone. So if it’s, meditation or deep breathing exercises or yoga, like how to dial down that stress response is critical.
[00:56:28] And then the big one that I harp on, and if you were watching, I’m wearing the blue blackened glasses. Yeah, I was going to ask about that too. It’s circadian rhythms over everything. If you do not get your rhythms set and you do not sleep well, it is almost like you took an engine, you never changed the spark plugs, you never changed the oil.
[00:56:47] And then you’re going to put premium gas in it, premium, organic food. And they’re going to try to run that engine at 200 miles an hour the next day, doing kit training, expect that engine to do anything. If you do not sleep well, things are not going to go very well for you. So if you’re not sleeping seven and a half, eight hours a night and waking up, like I feel awesome.
[00:57:04] Figure out what’s making you not sleep awesome, work there first, and then after you got that dialed in, then start tweaking the nutrition, the exercise routine, and then that car will start going 200 miles an hour again. So I’m always about, figuring out if that person’s circadian rhythms are off, and so we’re beings of light.
[00:57:22] We’re supposed to be outside during daytime and then when it’s dark, that’s when you’re inside. I’m supposed to be recovering We’re not supposed to be on these screens 24 7 these screens are amazing that I can talk to you I could talk to whoever’s on the other side and that might be across the world the light that comes off this screen It’s set at the same color temperature as noon to wherever you’re at.
[00:57:44] And so if it’s noon right now great But if this is 10 o’clock at night and you’re looking at this Your brain keeps getting a hit that it’s daytime and your body’s gonna make different hormones and neurotransmitters in relationship to that information. And so you’ve got to get tight with your light environments if you want to have optimal hormones, if you want to have optimal sleep.
[00:58:02] So I always start with circadian rhythms and sleep first, and then we dive into your exercise, your nutrition, and then we’re looking at the endothelial function test, the vascular test in your labs.
[00:58:12] Dr Mike T Nelson: And the reason you’re wearing an orange tint, is that to limit some of the blue light because you’re in front of a screen?
[00:58:19] Is that correct?
[00:58:20] Dr. Michael Twyman: Correct. So the lenses I’m wearing, they block approximately 450 nanometers of light, and that’s in the blue spectrum of light. So blue light is, not necessarily bad for you. That’s one of the reasons the sky is blue, but it’s the unmitigated blue light that the technology pumps out.
[00:58:38] It pumps out anywhere between four and five times more blue light than red light. Mother Nature Those things are more balanced. And so blue light is stimulating. It tells the body it’s daytime and you pump up more and more cortisol in response to that blue light. And so I don’t want my brain to think it’s the wrong time of day.
[00:58:55] So these glasses filter out about 40 percent of that blue light from hitting the back of my retina. At night, if I was having trouble sleeping, I would switch to a darker lens, the red or Amber lens, and that blocks all the blue light from reaching the back of the eye. So if you’re watching TV, your brain still thinks it’s like midnight and your body’s going to.
[00:59:14] suppress cortisol, and then melatonin, the hormone of darkness, will start being secreted. And that’s going to help you stay asleep, and melatonin is also what repairs the mitochondria, like the things that are behind me. Melatonin is a powerful antioxidant, and it’s released when there’s darkness. So if you protect the light from hitting your eyes, you’ll release the hormones in the right time.
[00:59:37] Dr Mike T Nelson: And quick question, I think looking at your website, and from what you just said, you are a fan of red light therapy? And do you think the red light therapy devices have any chrono effect? Meaning we are programmed to see more red light in the morning and evening if we look at like the, what rays are coming off of the sun, that type of thing.
[01:00:00] Dr. Michael Twyman: So yeah, so for the the photo by modulation panels I get that question a lot. Yeah, but probably the ideal time is use them like, you’re mimicking sunlight. So sun up to sundown is when you should be using them and yeah. Some people, will sleep better if they use it in the evening time.
[01:00:15] And there’s other people, just the intensity of light, not the color tends to mess with their sleep onset. And so you got a biohack this one to see if you’re one of those sensitive people or not. Yeah. I just, from a time standpoint, just like to do it more in the morning time. It hasn’t really affected my sleep in the past.
[01:00:32] I’m always about trying to recreate what mother nature has for you. So you would not, Blast yourself with intense light two minutes before you wanted to put your head down on the pillow. So I just thought it made more sense to do it earlier in the day. If possible.
[01:00:46] Dr Mike T Nelson: Any recommendations on length of time, or I know it depends on the panel and how bright and your skin exposure and, that’s another hour and a half
[01:00:57] Dr. Michael Twyman: podcast, at least another hour and a half podcast.
[01:00:59] But yeah that’s a challenge with these panels and the topical devices and the beds is that they’re not. Apples to apples, right? There’s three variables that you have to look at. You have to look at the wavelengths of light that come off the device. You have to look at the irradiance, which is basically what’s known as the power density.
[01:01:18] So think of it as is it a faucet that’s dripping photons or is it a fire hose? And then there’s the time. So shorter doesn’t always mean better. Like you could technically cook a turkey by dropping it in boil oil, but is that always better? Not necessarily. If you try to use a flashlight to cook a turkey, it’s never going to happen.
[01:01:38] So there is a Goldilocks window of like treatment for these devices. Now, broad strokes, it’s usually between 10 and 20 minutes for most of these devices. And for guys that are listening more is not necessarily better. So the device tells you 15 minutes is good doing it for two hours. You’re not going to get eight times the benefit.
[01:01:57] You’re going to lose the benefit because there’s something called the biphasic response. You essentially overcharge the circuit and you lose all the benefits that you got from putting the light in the first place and then you have to wait a day or two before the circuit basically fires back up and can accept those photons again.
[01:02:12] Got it.
[01:02:12] Dr Mike T Nelson: That’ll be a podcast for another time. I just spent Oh God, I started reading some research on it five years ago and I spent the last six months reading. Like hundreds of papers on red light therapy for this presentation I was doing and trying to figure out okay, based on the actual research and experience, like, how do you translate this and do something that’s useful?
[01:02:31] Because, like you said, there’s a lot of parameters, more power isn’t necessarily better. You build up a reactive oxygen species, which is good for a while, and then that can be a negative. And it’s not as simple as just buy a panel and sit in front of it for hours a day. That’s actually not a good thing.
[01:02:49] Awesome. So working people, if they’re interested in finding out more about you or working with you directly, I know you said you work with people from all over the world. Give us kind of the rundown of how they would do that.
[01:03:01] Dr. Michael Twyman: First off, thank you for the opportunity to use for
[01:03:03] Dr Mike T Nelson: great. Yeah, for sure. I appreciate all the
[01:03:04] Dr. Michael Twyman: info.
[01:03:05] This is great. I always love geeking out on the, like the end of field function tests. And then, you’re aware of, photo modulation. So it all kind of pieces together with exactly what we talk about with our people here. We are located in St. Louis for those that are willing to travel.
[01:03:16] We’re happy to work with them one on one for those that want to learn more about this information, I. Do some social media, mostly on Instagram. My handle’s just Dr. Twyman. Monday nights at 6 p. m. Central, I will do, ask me any things often. So if you have questions, I’ll answer them live and try to educate the people about certain topics, and it’s often very similar to these questions.
[01:03:39] You’re asking about, what does blue, black, and glasses do? And, what about ApoB? And how’s the best way to lower it? Those are the type of questions I’ll answer there. And then my website, it’s just drtweiman. com, and there’s links to some of my previous podcasts and some of the products that I talked about in these type of talks.
[01:03:55] Dr Mike T Nelson: And I believe if people are coming in, it’s typically just like a one day kind of a testing, right? So it’s not really a multiple day. If people are thinking about it, it’s not a, you don’t have to hang out in your place for a week. It’s a relative, you can get the test done kind of one after another and be on your way then, correct?
[01:04:11] Dr. Michael Twyman: Correct. And it really depends on what they’re coming for, but we often will help people actually do the clearly scan in St. Louis because they can’t get it to where they’re located. So often they’ll come in, for example, let’s get in by Thursday evening, they come see us very early, Friday morning, we do, about two hours in the office, and then we send them out to go get the clearly at one o’clock, and then they can fly out later Friday afternoon, if they like.
[01:04:32] Cool.
[01:04:33] Dr Mike T Nelson: Awesome. Thank you so much for listening to the podcast. Really appreciate it. Thank you to Dr. Twyman for all of his time here, all the great work he’s doing with this clinic there. We definitely do have that on our list to hopefully visit him there and do some more testing ourselves. If you want to hear his top four takeaways of tests, everyone should consider doing for cardiovascular health.
[01:04:57] Go to miketnelson.com/flex4 that’s F L E X, the number four. You’ll be able to get access to that directly there. If you’re on the newsletter, you will automatically get it there. So check that out. Big thanks to LMNT for sponsorship. Go to drinklmnt.com/mikenelson. You’ll be able to check out all their wonderful flavors.
[01:05:21] I’ve really been enjoying the grapefruit flavor a fair amount here as we’re wrapping up our stay in El Cuyo, Mexico. So thank you so much for listening to the podcast as always really appreciate it. If you have time to drop us a couple of stars or whatever stars you think it’s worthwhile. A short review on your favorite podcast player.
[01:05:42] That really helps us out with distribution of the podcast. Also, if you have someone who is interested in advanced cardiovascular testing or even performance related components, by all means, please forward this podcast to them. And if you want to share it online, that’d be awesome. And tag me so I can say, thank you.
[01:06:01] Thank you so much for listening. Really appreciate it. We’ll be back next week. See ya.
[01:06:07] Do you suppose they have any life on other planets? What do you care? You don’t have any life on this one!
[01:06:15] Nancy: This podcast is for informational purposes only. The podcast is not intended as a substitute for professional medical advice, diagnosis, or treatment. You should not use the information on the podcast for diagnosing or treating a health problem or disease or prescribing any medication or other treatment.
[01:06:31] Always seek the advice of your physician or other qualified health provider before taking any medication or nutritional, supplement, and with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have heard on this or any other podcast.
[01:06:47] Reliance on the podcast is solely at your own risk. Information provided on the podcast does not create a doctor-patient relationship between you and any of the health professionals affiliated with our podcast. Information and statements regarding dietary supplements are not intended to diagnose, treat, cure, or prevent any disease.
[01:07:04] Opinions of guests are their own, and this podcast does not endorse or accept responsibility for statements made by guests. This podcast does not make any representations or warranties about guest qualifications or credibility. Individuals on this podcast may have a direct or indirect financial interest in products or services referred to therein.
[01:07:22] If you think you have a medical problem, consult a licensed physician.
[01:07:26]

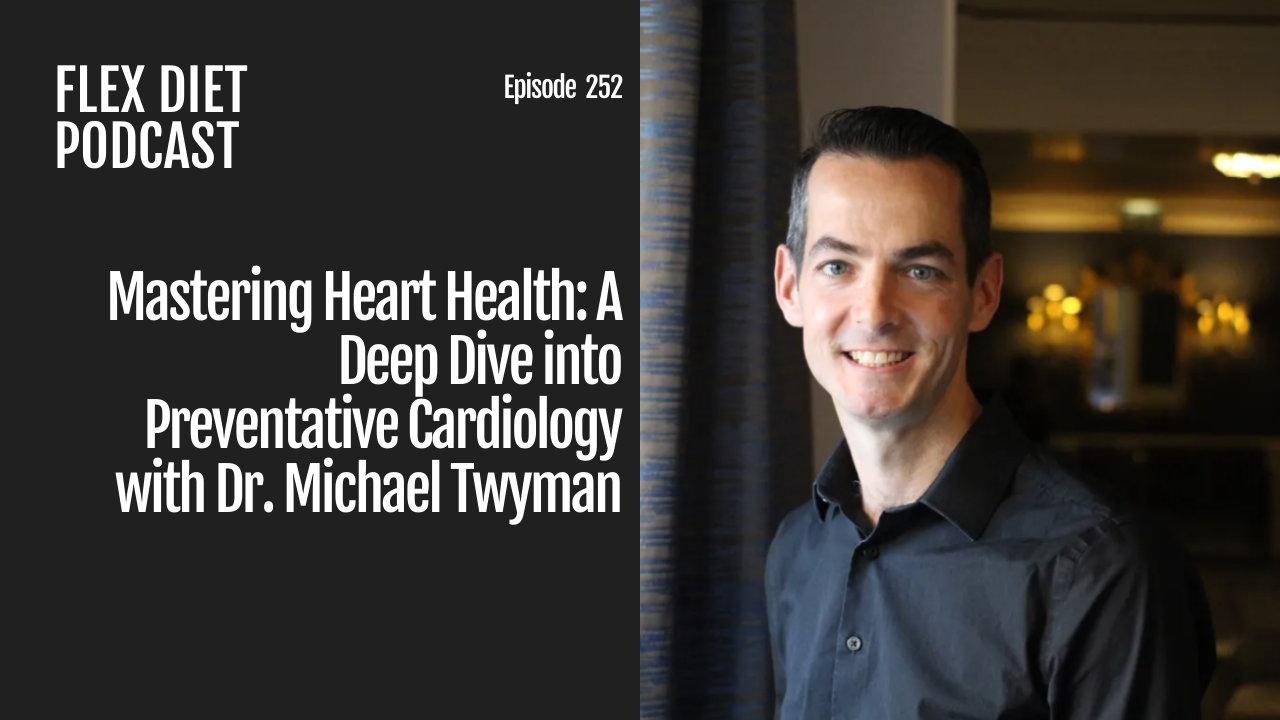




Leave A Comment