On today’s episode of the Flex Diet Podcast, registered dietician Catherine Saffieri and I dive into the world of preventive health and personalized nutrition. With Catherine’s guidance, we unravel the intricacies of glucose response and the impact of various lifestyle choices on glucose levels.
Sign up for my geeky, almost-daily email newsletter about how to add muscle, increase your performance, and improve body comp all without destroying your health.
Episode Notes:
- [7:23] Catherine’s personal health story
- [11:54] CGM and personalized nutrition
- [17:59] Understanding glucose response and context
- [28:42] Improving glucose levels in short timeframes
- [36:59] Lifestyle and sleep’s impact on glucose
- [47:26] Metabolic health and cold water immersion
Links:
Reference:
Stork MJ, Marcotte-Chénard A, Jung ME, Little JP. Exercise in the workplace: Examining the receptivity of practical and time-efficient stair climbing “exercise snacks”. Appl Physiol Nutr Metab. 2023 Sep 25. doi: 10.1139/apnm-2023-0128. Epub ahead of print. PMID: 37748202.
Rock on!

Dr. Mike T Nelson
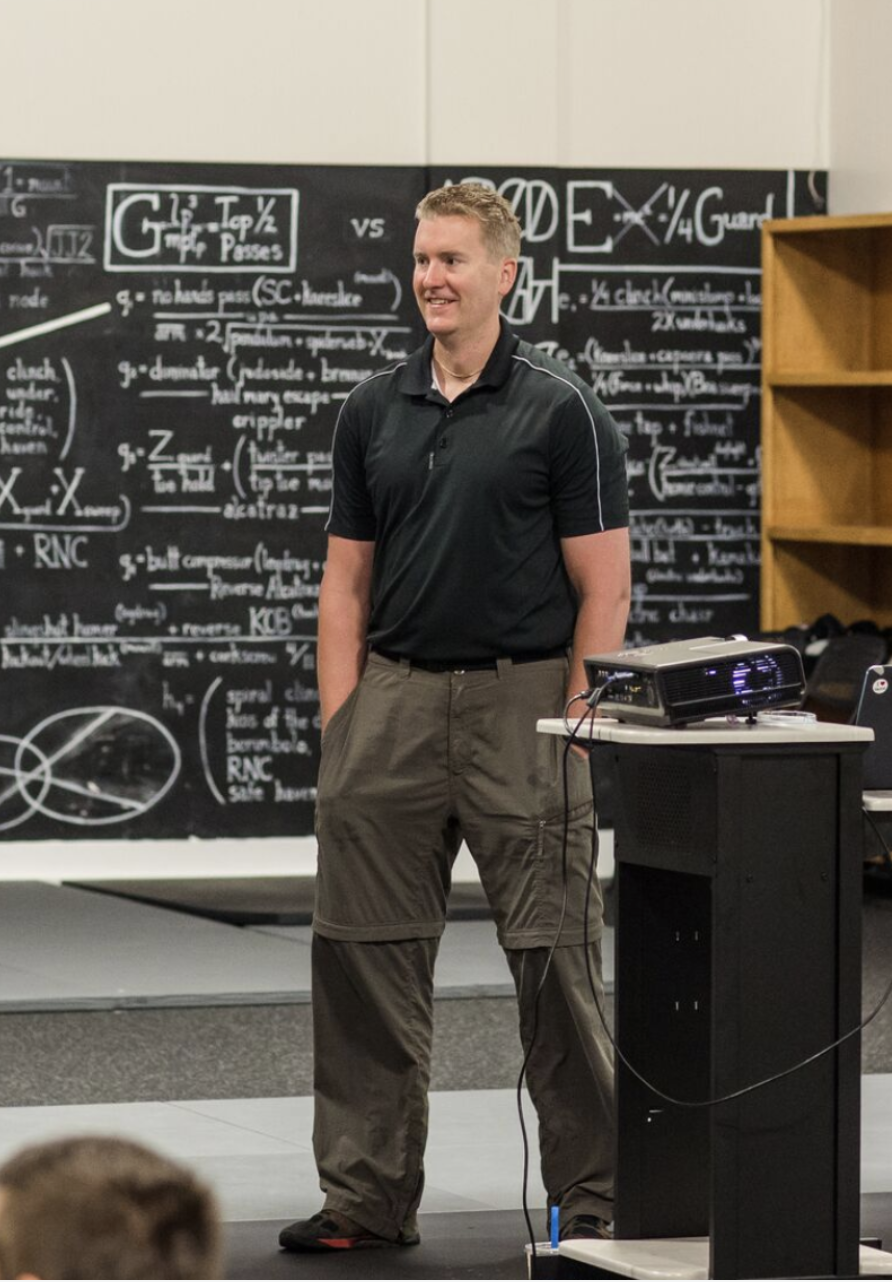
Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member
[00:00:00] Dr Mike T Nelson: Welcome back to the Flex Diet Podcast. I’m your host, Dr. Mike T. Nelson. On the podcast, we talk about all things to increase performance, add more muscle, improve body comp, and do it all without destroying your health in the flexible framework. A huge thanks to everyone who enrolled in the physiologic flexibility certification.
[00:00:23] Super stoked for all of you to get into the material there. Really appreciate it. And related to glucose that we talk about in a big dive in the PhysFlex cert, which is closed now, closed on Monday night, I wanted to talk about continuous glucose monitors. And so we’ve got a whole podcast here with Catherine from NutriSense talking about just that, continuous glucose monitors.
[00:00:56] So Katherine is a registered dietitian, nutritionist, and she currently works as a nutrition manager at NutriSense, which is one of the companies that provides continuous glucose monitoring, and they allow you to talk to a professional about what you’re actually seeing. So you actually get good interpretation of your data because it can be a little bit confusing.
[00:01:19] She’s worked with thousands of clients and has reviewed over 750, 000 hours of glucose data. In recommendation of different meals and follow ups. She has a Master’s in Nutrition Education from Columbia University also, and done her undergraduate work at the University of Pennsylvania. So in this podcast, we talk about how she got into continuous glucose monitoring.
[00:01:43] Based on all of the data that she’s seen, what trends does she notice? The dreaded grapes and are they good or bad air quotes here for your glucose? More data equals more awareness. So one of the tricks I do with online clients and what I teach in the flex diet mentorship is it’s not worth arguing with clients.
[00:02:07] You probably need to get their awareness first. And this is where I think data becomes incredibly powerful. The dynamics between insulin and the glucose, and I’ll link to a podcast I did with my buddy dr. Tommy Wood about insulin and glucose. You can go on a deep dive on that. And then how should you set up your continuous glucose monitor?
[00:02:29] What kind of experiments should you do? So I’ve been working off and on with continuous glucose monitors, man, probably going on four years now. Maybe it’s even over that. First with Dr. Ben House in Costa Rica where we threw a bunch of continuous glucose monitors on people and had them eat all sorts of, crazy things for down there, pineapple, rice cakes, et cetera.
[00:02:52] And what was really shocking to me is there was a huge difference from one person to the next. Even when we tried to control the same amount of carbohydrate. These are a bunch of lifting dude bros who were like super healthy. And it didn’t really have any pathologies going on. So I’ve had a glucose monitor on myself.
[00:03:12] I even stuck one of my wife’s right arm in her left arm just to compare them. To make sure they were semi accurate. So shout out to Krista from The Points Retreat for originally hooking me up with those many years ago. Podcast.
[00:03:33] There is, in essence, a wrong way of doing this, too. I’m not a big fan of using data, whether it’s HRV, continuous glucose monitors, ketone levels, whatever, into scaring people, the bejesus out of them, into doing things. You definitely want to show them where they can improve and what they’re doing well.
[00:03:52] But just like looking at your sleep data from Aura or your HRV from iFleet or whatever. The goal is to use the data to become more resilient and more healthy, not to feel like you have to live in this box and never color outside lines. So again, that’s my biased opinion. I think some people get a little bit too neurotic about their data and that also can be a negative.
[00:04:20] But overall, I think awareness, in most cases, is definitely going to be a good thing. Enjoy this podcast on Continuous Glucose Monitors with Catherine from NeutroSense.
[00:04:34] Dr Mike T Nelson: and welcome back to the Flex Diet podcast. Yeah, Catherine, thank you so much for being here. Really appreciate it.
[00:04:40] Catherine Staffieri: Thank you for having me. I’m excited to be here
[00:04:42] Dr Mike T Nelson: and talk to you. Yeah, so today we’re talking about continuous glucose monitors, which have been around for some time, but I think they’re becoming more and more popular now.
[00:04:55] And how did you get into working with continuous glucose monitors? Usually most people have a interesting story related to it.
[00:05:04] Catherine Staffieri: Yeah I wouldn’t say it’s, super I would say, I’ll start with this as a second career for me, oh, okay. I used to work, yeah, I used to work in finance in in New York City in the hedge fund space.
[00:05:15] That was all my undergrad work. And I really felt like after about eight years, 10 years, I was like, this is not where. It’s not where I feel like, my passion lies. It’s not where I, what I wanna be doing in 20 years, so I was lucky enough, I went back to school. I got my master’s in nutrition education.
[00:05:32] And then from there, as you meet I’m a registered dietician. As you meet other registered dieticians, you start to hear their stories. And I remember one of ’em once said to me, you will wear many hats in this career. You will not just have one job. And had a bunch of different jobs after going to school.
[00:05:48] And then it was during the pandemic, I had a private practice. I was seeing a lot of people locally and during the pandemic I said, gosh, I really miss working with people and I miss working collaboratively and outside of the box. When you’re a dietician you’re trained in those very traditional clinical areas, right?
[00:06:07] You have your low sodium diet in the hospital. You have your low carbohydrate diets in the hospital. You’re not really allowed to think differently outside of that. And so I hunted around and I came upon Nutri Sense, which is a company that I work for right now, and they are providing CGMs, continuous glucose monitors.
[00:06:26] To a non-diabetic population, although we do take type two dia diabetic people. And it’s really a preventative health effort, and that just got me fired up, right? Because that’s really where my passion lies as a dietician, is helping people prevent those chronic diseases that can occur later in life because it takes decades to get there and you need to start early.
[00:06:50] So that’s how I found them. I’ve been working for Nutrisystem for a little over two years now. And it’s been incredible.
[00:06:57] Dr Mike T Nelson: Awesome. For, if you don’t mind speaking about it for yourself, what was most illuminating out of the course of just your, I dunno, personal health story and then the second part to that question is what trends have you seen, especially given your background looking, I would assume at a whole bunch of data in a different domain, but now you can maybe apply those same skills to your new domain here.
[00:07:23] Catherine Staffieri: Yeah. Personally I’ve always had GI issues just gut health stuff, and that is a real kind of wild west frontier right now with the research. There’s a lot of research. There might not be as many conclusions. And so I was always looking for, what could be causing this, what could be doing that, all those kinds of things.
[00:07:41] And I had no idea how much glucose can be impacting not my immune system and then therefore my gut health. And what I loved about learning about using the continuous glucose monitor was I compared to basically a window inside your gut. A window inside your body, really to see what’s going on.
[00:08:00] Who wouldn’t wanna see what’s happening in your body real time, right? You can see what’s going on with exercise. You can see what’s going on with food, with stress, with sleep. So I was really intrigued by the live. Continuous feedback data that I was getting from it so I could really test out the different foods that I was having to see what kind of responses I was getting.
[00:08:20] That’s me personally. And then, oh my gosh, yes. In terms of hours of data, I’ve looked at hundreds of thousands of hours of data thousands of members of I’ve helped counsel throughout my time at Nutri Sense, and that’s been really fascinating to see how certain people coming to us, say with a general goal of, longevity or I’m training for a race or something like that.
[00:08:44] They have these aha moments where things that they thought were really fantastic and working well in their life maybe aren’t, there’s a be there’s a way to better optimize it, right? Or, helping someone realize the stress, how that’s impacting their life. It’s these aha moments for people that have been so rewarding.
[00:09:02] Dr Mike T Nelson: Cool. I guess general trends related to specific types of foods. Cuz one of my pet peeves with continuous glucose monitors, this is not the monitor itself for the companies or anything. It’s the oversimplification of one guru gets a device, puts it on their arm, and all of a sudden, oh, I had grapes and look at my blood glucose, it went bonkers.
[00:09:27] Therefore, grapes are bad for everyone. It’s eh I wouldn’t really jump to that conclusion, but I get it that people listening want this is a good food, this is a bad food. Oh, it was bad for this person, so I’m gonna avoid this too. And it just seems like if that’s, The mode of operandi you can find anyone and next thing you’re just eating, I don’t know, grass fed steak or something, right?
[00:09:52] You end up doing a carnivore approach cuz you get so scared off of like any other foods versus using a device like trying to get your own data. How do you feel? How do you perform? What is best for you as an individual instead of applying somebody else’s an individual data to themselves.
[00:10:08] Catherine Staffieri: You hit the nail on the head.
[00:10:09] That’s exactly it. We, I could not agree more. We say a lot of this n equals one. That this device this data, this is your own experiment, right? When you read any type of scientific journal article study, there’s always the n equals that, that’s the population in the study.
[00:10:26] So n equals 5,000, n equals 10,000, depending on the size. Of the study. This is a study of one. This is your study. And so grapes for you are different than grapes for me, oatmeal for me is different than oatmeal For you, not only is it just body composition, right? Depends on your muscle mass versus my muscle mass.
[00:10:44] It depends on my stress level versus your stress level. What are you pairing it with? There’s all these nuanced factors that, that’s why we really find this kind of data to be so specific and really helpful because it’s not just watching someone on Instagram say, oh gosh, I had grapes.
[00:11:01] And look what happened. Therefor, exactly. We’re only eating steak from now on. It’s okay, so I love having this food. I love watermelon or I love to go out on a date night with my, my, my spouse. How can I have that in the best way possible? Because I don’t wanna give up my lifestyle.
[00:11:17] I don’t wanna not eat carbohydrates. We’re not anti carbohydrates, right? It’s just about finding a way to optimize it.
[00:11:26] Dr Mike T Nelson: Have you seen any kinda general trends of foods that tend to be more problematic or is it really individual? And the reason I ask is if someone were to start testing, what would be a spectrum to start from?
[00:11:41] Okay, yeah, these are things that generally are good and then these things, can get a little bit more squirrely on the other end.
[00:11:49] Catherine Staffieri: Yeah, I think there are a lot of. There are a lot of surprise foods that, that people don’t realize can spike their glucose. So something like sushi or oatmeal quinoa, things that people are like, this is so healthy.
[00:12:02] I’ve been having it for years. They don’t realize necessarily what’s going on and then really what’s happening afterwards. So what you’re seeing in the glucose monitor data, I don’t know how familiar your audience is with it, is that, you’re seeing a graph and you’re seeing it real time. So what’s interesting is, What we look at in terms of a meal is the two hours after you start eating.
[00:12:26] And we offer a meal score in our app so you can rate yourself as to how you’re doing. And there’s lots of metrics involved in how that score comes out. But we wanna see what happens after that. Do you have a crash? Is your glucose spiking super high and then crashing down? Or are you doing things to mitigate that spike to make you have more gentle, gentle ups and downs, gentle sort of ocean waves is what I compare it to.
[00:12:49] So a lot of times, yes, someone will have a bunch of grapes and then they sit down, they’re at their desk and they’re not moving around. And so absolutely their glucose will spike, right? But if they’re having those same grapes after chicken salad or tuna salad or something like that where they’ve had protein, maybe some healthy fats, some avocados before that, you’ll have a very different response.
[00:13:08] Same if you’re breaking your fast, right? So breaking your fast. Could be a 12 hour fast. It could be, dinner to breakfast or up and, whatever your schedule is. But anytime you’re breaking a fast, if you’re hitting it with carbohydrates, if you’re hitting it with some orange juice first thing in the morning, something like that can really raise your glucose super high and come crashing down afterwards.
[00:13:28] So in terms of those trends, what we see is it really depends on what you’re eating, when you’re eating and in what order you’re eating in.
[00:13:37] Dr Mike T Nelson: Got it. Yeah. I think the context is what people forget about all the time, like they did. Even you, I had various clients do the same experiment, and we’ve played around a lot with continuous glucose monitors.
[00:13:50] God probably going back almost four years now, and it’s very easy for a client to look at something and be like, we’ll just pick on grapes of, oh, I had grapes for breakfast, and, oh, look at this, it spikes super high and then dropped. It’s Okay. What else did you have? I didn’t have anything else.
[00:14:06] It was the only thing I had. Okay. It was first thing in the morning. Did you train yesterday? Were you high stressed? And even just movement throughout the day or post-training. A lot of times I’ve taken clients and had ’em test the same food after they got done doing, 60 minute strength training session.
[00:14:23] And they’re completely bewildered at that point. Cause they’re like, I thought this was bad, but now it’s okay. Just to illustrate that it’s not always necessarily the food itself, it’s the context. When did you do it? Timing, movement, all these other things can play into everything too.
[00:14:41] Catherine Staffieri: And absolutely to your point with strength training is the amount of muscle that you have is the amount of storage space. You, the more muscle you have, the more storage space you have for glucose, right? And so your body’s ability to handle a glucose load of carbohydrates and grapes can be very different depending on, a woman with much less muscle mass than someone who’s a guy who’s working out all the time and has a lot more room for storage.
[00:15:05] So that’s also a real eye-opener for a lot of people. And that’s why we really try and encourage all sorts of movement, not just cardio. Cause a lot of women just think, oh, I’ll be on the elliptical for an hour and everything will be great. And then as they get older, it’s not really working in the same way that it used to.
[00:15:20] So we really promote making sure that they’re maintaining and if they can build that lean body mass, not only for good glucose control, but as for all sorts of functional movement, functional health not falling, not breaking anything, all that.
[00:15:34] Dr Mike T Nelson: And for numbers, what do you consider for, let’s say just a fasting blood glucose number, that kind of a range you guys would consider as, good or a target range?
[00:15:44] And then what would you consider for sort of a spike post-meal? And about what levels would you wanna see that come back down to?
[00:15:51] Catherine Staffieri: Yeah, so we start out with our default ranges and our default when you open our app, we have a time within range band. And that’s just the default.
[00:15:59] That’s the general what we expect most people not coming to us perhaps with the type two diabetes diagnosis where those. That bandwidth and those metrics might be elevated at the time. So our fasting glucose range that we like to see is 70 to 90 in the mornings.
[00:16:16] And then our time within range is 70 to one 40. So we like to see a meal spike to stay underneath that one 40, but it’s all adjustable. And so we have some people that say, I absolutely don’t wanna go over one 20. Some people are like, I don’t wanna go over 100. And sometimes people are coming to us with their glucose wildly dysfunctional.
[00:16:36] They, they’ve got a dysfunctional metabolic health and they’ve got dysregulated glucose metabolism. And so we just, we don’t wanna discourage anyone. We just up that band and we, we really work with them towards their goals wherever they are.
[00:16:51] Dr Mike T Nelson: Yeah, I like that. My, my bias for normal range, it’d say 80, 90, I think you could go a little bit lower as long as you’re not symptomatic, I think is fine.
[00:16:59] Peaks, I would agree, one 20 to one 40. It just seems like people get more as they monitor stuff. It seems like there’s a, on the fringe aspect, a driven desire to show your numbers are better than your neighbors. And sometimes I think I had one person who didn’t wanna ever go above a hundred and there were normal healthy person like no issues.
[00:17:21] And I’m like, I don’t know. I think if we gave you a whole bunch of carbohydrates, seen a spike to one 20 or one 30, as long as you can clear it on the backside, I’m not really that worried about it. I think there’s been an over extrapolation of some of the data from, as from type two diabetics showing that yeah, if your glucose is definitely on the high range and it’s staying up there for periods of time, like you’re definitely gonna be in a world de hurt.
[00:17:46] But it’s not this nice linear response where if you can, get it below a hundred all the time, you’re gonna be better than someone who hits one 20. I don’t it physiology doesn’t work in that nice, neat, linear response.
[00:17:59] Catherine Staffieri: Exactly. And glucose is not the enemy, right? The body really thrives on it.
[00:18:03] The brain particularly loves it. Not that I’m against ketones, but what we love to see is that the ability to flex in and out of your different fuel sources, right? Nothing wrong with getting into ketosis, nothing wrong with staying in ketosis for whatever you want, however long you want. But we like to see that, the that then you can have some carbohydrates.
[00:18:23] Add them, whole grain carbohydrates into your diet and your body can handle it. What we see sometimes with people that have been on a ketogenic diet are very low carb for a very long time, is that sometimes you get a little bit of physiologic insulin resistance. Yeah. So it’s short term.
[00:18:37] Yeah. You might be familiar with it. So it’s short term. The body should, get right back to, being able to use glucose again pretty efficiently. But it can be a couple days of readjusting to that fuel source. But we wanna see people that can flex in and out of both of them, because long-term can be really hard to follow a ketogenic diet for the next 40 years, whatever it is.
[00:18:59] Very few people, I would say, can handle that kind of dietary restriction for such a long period of time. Therefore, we wanna make sure that our members are able to live a healthy lifestyle. And to have those periods where you might have some higher carbohydrates and some lower carbohydrates.
[00:19:15] Dr Mike T Nelson: Yeah, and obviously that’s my bias with metabolic flexibility, right? So can you handle higher periods of carbohydrates? Can you handle lower periods of carbohydrates, right? You wanna be able to handle, both fuel sources, fats and carbohydrates. And one of the, one of the very first times we did this was with the I think at the time the reader only could look at a week’s worth of data.
[00:19:37] So only one person in our little group had a reader. So we had a local nurse she’s Hey, do you mind if you guys run this experiment? Yes, this would be great. We had six people that did it. We came over, had this little party stuck, all little sensors on us, and she was like, if it’s okay with everyone, can we get back together in, two weeks?
[00:19:53] We’ll collect all the data at once and just compare notes. We’re like, yeah, it’s great. And so during that time, we didn’t see any of the data, we didn’t know what was going on. We’re, doing all of our food logs and everything. So we get together and we’re just, she has all her individual reports for us, and we’re going around the table.
[00:20:09] And the person I knew at that time was very strict keto. And the nurse is Hey, what happened on this day? I see, your blood glucose was, high. And she had, I don’t know, some like three crackers or something like that. It wasn’t a high amount of carbohydrates. And she was all very upset about it because she was like I’m supposed to be doing this healthy diet, and I just had this small amount of carbohydrates and now my glucose is super high.
[00:20:36] And it happened again on this other day. And I was trying to explain to her like, what’s going on? It’s probably not a negative thing. It’ll probably, change over a few days. It’s a non, pathological insulin resistance, the muscle level, blah, blah, blah, blah, blah. And she got mad and she’s oh, what did you have for breakfast that morning?
[00:20:54] And I’m like let’s see. Oh, this was the day I was seeing, what levels of glucose I could get to. So I had oatmeal and three cookies and she’s what were your levels? I’m like, 1 23. She’s oh, I hate you. You suck. You’re horrible human being. I’m just like, but I generally exercise a lot.
[00:21:12] I generally have higher amounts of carbohydrates I’m more used to it, so I thought it was very interesting that even going as you go more extreme, you can see these kind of temporary changes. And then also it’s very hard for people to not get hung up on their values of what you get on a score is kind of part of your identity of who you are at the same time too.
[00:21:36] Catherine Staffieri: Absolutely. And listen, to be fair, this can be a triggering thing for people. Oh yeah. Very. This, just as any tracker wearable, calorie counting track can be a triggering thing for some people and can motivate you in an unhealthy way. But what we like to see is that it can help liberate some people’s diet, so that some people that have been so strict can say gosh, maybe I can work on this and incorporate some carbohydrates on a slow basis so that I don’t have this reaction when I do eat some.
[00:22:06] And then you get those physiological feelings after, I wonder how she felt after that big cracker spike, right? If she crashed down and felt crummy afterwards. We feel like it can be liberating for some people, but it can be triggering for others. So you just have to be pretty careful.
[00:22:20] And, with the scores, we talk a lot about calibration. People get very upset What is my baseline? I need to know what my baseline is. And, all of these devices have a bit of, margin of error built into them. We, we really emphasize trends, right? We wanna see, that’s really the point of the continuous glucose monitor, right?
[00:22:37] You can just take a finger stick every day and get your fasting glucose right? But what we wanna see is the trends over time. That’s way more important. And frankly, the glycemic variability is a bigger predictor of insulin resistance over time. And that’s very hard to measure that glucose variability with, finger sticks throughout the day.
[00:22:55] So that’s why we really try and emphasize people looking at more of that holistic picture as opposed to getting, focused on the
[00:23:02] Dr Mike T Nelson: one number. Yeah. And I believe you guys are using, is it the Libre Freestyle? Is that what you’re using? Correct. Yeah. And have you seen pretty good agreement between that’s actually measuring the interstitial level of glucose compared to blood glucose?
[00:23:14] So it’s not the exact same thing, but we did a bunch of experiments for a while where I freaking hate needles. So I, a buddy of mine were like seeing how often we could tolerate finger pricking ourselves and measuring blood glucose and looking at the C G M and they weren’t always exactly the same, but I, it did appear that the trends were following in the same direction.
[00:23:35] And then later on I also took and put a sensor on my wife’s left deltoid, and then we waited 10 minutes to put one on her. And so we had the two graphs done at different times and we superimposed them, just to make sure the trends were kinda lining up. And you did see a little bit of different numbers between ’em, but in general, the trends were in good agreement too.
[00:23:55] So it’s, again I agree that it’s looking at the variability and the trends over time, and I think people easily get hung up on one number or, oh, I went from 80 to 75. It’s who cares? It’s like you’re just so far down in the weeds at that point, especially on the low end of these things.
[00:24:10] It’s ah.
[00:24:12] Catherine Staffieri: Yeah. No, I agree. I agree. What I think what’s so rewarding is seeing, those people that do have those higher swings and they’re able to lower them down, right? Or the people that do have very high fasting glucose or, something like that that they’re able to bring it down over the course of a couple weeks, of a couple months.
[00:24:27] How about of your, people that you’ve been helping with this, what have been the time, the timeframes that you’ve seen with the most improvement in their glucose values? Has it been three months? Has it been shorter than that weeks?
[00:24:40] Dr Mike T Nelson: We’ve generally seen, and we don’t work with a lot of pathologic people, but through the one nurse she had a couple of people that, were frank Type two diabetics, so were in the supervision of her physician.
[00:24:49] And there was one guy who, and he was pinging like, 300, 2 50, just really high. And what was fascinating is that, He was very non-compliant with everything, but once he saw the actual data, it was almost like he couldn’t really run from it anymore. And so once he actually started doing stuff, like he saw huge improvements even in just four weeks, so I’ve seen some pretty with people that tend to, fluctuate up a little bit higher. Some people we’ve seen big changes in just a couple weeks, might be modifying when they took the food in sleep. Stress. We do a lot of monitoring of heart rate variability, looking at stress levels and usually just trying to figure out like what is the main leverage point for them.
[00:25:33] Are they just not moving enough? Do they need to make another food choice? Are they need more sleep? Can they manage their stress? And it’s pretty crazy. I think I’d be interested in what you guys have seen, but even in a couple weeks, like you can see measurable changes in a fair amount of people, which.
[00:25:49] Is more responsive than what I would’ve predicted overall. Cause I think we have this thing, and I tend to fall in this category too, that, it took you many years to get to where you’re at. It’s gonna take you many years to get out. But it appears that physiology is very, a symmetry orientated towards your physiology wants to actually get better, it wants to be more efficient.
[00:26:14] Because we’ve seen people, borderline type two diabetics who know how long it took ’em to get there, and in some cases, four to six months, like they look like a normal, healthy person. Blood tests, everything else. To me that’s like fascinating. Your body can take so much abuse for years, but yet you start doing things better and within a few months you can actually get back to a much higher level.
[00:26:37] It doesn’t take you years upon years.
[00:26:40] Catherine Staffieri: Agreed. Absolutely. The body wants to perform efficiently. It’s like the body wants to un gunk. The gears, right? Yeah. And you can, if you can clear some stuff out, you just, and the cellular turnover in your body is, pretty rapid.
[00:26:52] And so as soon as you can start, producing and the mitochondria is running and everything’s working better it snowballs. It’s that flywheel effect, right? And then all of a sudden you’re sleeping better and then all of a sudden you’re sleeping better, you’re more active and you’re making, he like all of that snowballs into a much healthier lifestyle.
[00:27:09] Yeah.
[00:27:10] Dr Mike T Nelson: What are some of the bigger changes you guys have seen on your end, since you obviously have a, like way more data than I see.
[00:27:16] Catherine Staffieri: Yeah, it’s the same thing we get people coming in with, I’m on Metformin, I’m on X, Y, z. We don’t take type two diabetics that are on insulin.
[00:27:23] But, on any number of blood pressure medications, cholesterol medications, within three months they’ve lowered their dosages within six months. They, maybe are off medications. I had a member who ha was a diagnosed type two diabetic. Couldn’t perform at his job.
[00:27:40] He had to take some leave from his job, wasn’t able to do it. And then maybe it was a full year. I think just because of like scheduling and hearings and stuff like that, he was back at his job. He basically, had not reversed it, but had gotten back down to the levels where they then allowed him to perform, which I thought was pretty incredible.
[00:27:58] And again, I don’t know how long it took him to get there, but it certainly wasn’t one year. It was much longer than that. Six to nine months probably when he was actually, his labs were showing no a1c elevated A1C or elevated fasting glucose. So it’s pretty incredible.
[00:28:12] I do think it depends on the commitment and the motivation of the person. Some people really jump in and are like, I’m ready for a change. I’m gonna make this happen. It just can take longer for some people to really institute those behavior changes. Cuz that’s what you’re, that’s what you’re looking for, right?
[00:28:26] You’re looking for someone to really commit to this. For the rest of their life so that they can mitigate that chronic disease on the long term. And if it doesn’t stick, if you’re not gonna do it, you gotta find something else.
[00:28:38] Dr Mike T Nelson: What would be some, for people listening, like leverage points you would look at?
[00:28:42] So let’s say you’re looking at someone’s data, eh, they’re generally pretty decent, but they have excursions that kind of go up to, 1 50, 1 60 and they hang out there for, quite a while. It takes them, two, three plus hours to get back down to baseline. What would you be thinking as things they could try to improve that then?
[00:29:05] Catherine Staffieri: Lots of different ways to attack it. We, depends if they’re logging their meals in the app. If not, that’s the first question, right? What did you eat? Sure. What’s the fat composition? We see a fat and alcohol can really impact the body’s recovery. That recovery is your return back to baseline.
[00:29:23] So depending on the composition of your meal, when we see really high fat carbohydrate foods like a fettuccine alfredo or a lot of pizza, something like that, the fat will delay the body’s ability to process the carbohydrate. So that’s when we see those higher swings and, it doesn’t even have to be that high, but it’s that slow recovery.
[00:29:44] They’re not coming back down. The body isn’t able to clear it because it’s processing the fat, the second thing is when there’s alcohol involved, so the body will pri well, the body will make the priority of processing the alcohol first. So a lot of times at dinner we’ll see oh, this, it just, it didn’t, I didn’t come back down for a long time.
[00:30:00] And we talk about, what did you have anything to drink with your dinner? What was going on there? Cuz that can delay and even the fat, you can see double and triple spikes later on as the body is able to process some glucose, then it has to stop, then it’s able to process some glucose and then it stops.
[00:30:13] So we talk about the composition of the meal and then we talk about movement after the meal. That’s a huge, easy free hack that someone can do to help. Manage their glucose and get that recovery back down. Because if you’re eating at your desk and then you’re just sitting there, taking phone calls, maybe you’re stressed out, whatever, it’s, you’re not moving, what’s your body gonna do with all that incoming energy?
[00:30:35] Same for dinner. If you’re eating late at night, you get home, you spend, stressful day. You just cram something in really quick, and then you watch Netflix and you roll into bed. Your body is doing nothing, right? Your body’s doing nothing with that incoming energy. So those are two things that we talk about.
[00:30:50] First and foremost, what did you eat when? What was the composition of your meal? And did you do any kind of movement afterwards? It is incredible to see the drop in your glucose from a walk after J. It’s so simple. It’s so ridiculous. And then when people see it, they’re like, oh my gosh, I had no idea.
[00:31:06] Also, just eating a little bit earlier in the day as you guys might already know, we’re more sensitive to insulin earlier in the day. There’s a huge movement towards krono, nutrition, eating more tur in terms of our circadian rhythms during daylight hours, which. Goes against the intermittent fasting trend of eating later in the day.
[00:31:26] But a lot of people have found that if they just move that last meal earlier in the day, the body’s able to process it better, more efficiently. So we talk about all that kind of stuff. Are you having a dessert late at night? What if you switch that dessert to earlier in the day, maybe an afternoon dessert, and then your body can handle that glucose load better, just physiologically?
[00:31:45] Dr Mike T Nelson: Yeah. I think the, excuse me, the walking and movement after like just for most people is a huge thing. I know Stanine has talked a lot about this when I’ve talked to him about it, and I think we tend to forget that just muscle contraction in and of itself from simply walking. Independent of insulin can pull blood glucose directly out of the bloodstream.
[00:32:08] I know it’s called non-insulin mediated uptake. And there’s been some super interesting studies, some older work in dogs that’s showing in that at lower to moderate levels, like most of where your glucose is coming from might be related to that mechanism. So I think a lot of times, excuse me, we think of just formal exercise, like you gotta go train really hard and you’re using more glycogen then, which is true, but I think we forget about the just low intensity activities can be super beneficial.
[00:32:39] Catherine Staffieri: Absolutely. Absolutely. And yeah, coupled with the strength training. But yeah, I just, I always tell people, I have this really lame motto that my husband always rolls his eyes at. I say, after you eat, move your feet. And he’s
[00:32:49] Dr Mike T Nelson: Oh, I like that.
[00:32:51] Catherine Staffieri: I gotta get like a trademark and put it on a t-shirt. But it’s incredibly powerful.
[00:32:55] You look at, people that live in urban areas, people that live in Europe it’s very common to eat and then take a walk or to walk home from, whatever’s going on. And so it, our lifestyle is not built that way. So many people in this country they don’t even get off of work until late.
[00:33:11] They don’t have time to prep for a healthy meal. They get home. They have x, y, z number of stressors that they’re walking into in their house. The last thing they can do is prep for a healthy meal and then go for a walk. They’re like, it’s 10 o’clock at night, what do you expect me to do? So we try and work on some ways to, to institute that as often as one can. And once you make. Room for that in your brain and you make it a priority. There is, you can find those 10 minutes, right? We’re not looking for an hour long walk. It can be a 10 minute brisk walk and really, depending on any kind of weather or whatever’s going on, you can do that.
[00:33:45] Dr Mike T Nelson: Yeah, there is a fascinating study I read the other day, using the term exercise snacks and they did it, I think as low as six bouts during the day for one minute each of just going up and down the stairs, right? So they didn’t even have people go outside, like if they have stairs in their house walk up and down your stairs for one minute, do that six times a day.
[00:34:05] And these are in, generally healthy people, not athletes, but they saw some, pretty nice improvement in a fair amount of metrics with literally just six minutes a day and it wasn’t like high intensity training either. So I thought that was pretty fascinating.
[00:34:19] Catherine Staffieri: Yeah, there was a study I saw back in, I think, March, and it was that same idea, that 30 minutes broken up into 10 minute chunks throughout the day actually resulted in better glucose control than one single 30 minute exercise done.
[00:34:32] And then being sedentary for the rest of the day. It’s a case to be made. You don’t have to work out and be crazy and, carve out hours and hours at the gym. You just need to move around throughout your day, be more
[00:34:42] Dr Mike T Nelson: active. Yeah, I remember talking to John Brody about this years ago because we were at a seminar and people were saying that, oh, but I have a desk job, but I exercise really hard for an hour a day.
[00:34:54] And he is that’s good. Exercise is definitely beneficial, you should try to get some other movement during the day. He is if we looked at your overall movement pattern during the day, it’s not much. Huge spike. Back to not much. Not much. Not much. And so now it’s, there’s obviously a lot more emphasis on, walking and getting step count and stuff, which is good. Yeah.
[00:35:11] Catherine Staffieri: Yeah. And it’s motivating. I think it is motivating, when you see that in your glucose monitor, it’s really motivating to know that, okay, I can have a work lunch or I can enjoy the bagel that I used to love all the time or something, but I, now I can go out for my, the sushi dinner that I love, but I know what to do to ha to optimize it better in my body.
[00:35:31] I know that I need to build in that walk afterwards. I know I need to build in a strength training session before I go out to dinner. Something like that, so that you’re able to see exactly what happens to your body and how you can make it better.
[00:35:45] Dr Mike T Nelson: Agree. What do you see related to sleep both acutely, since it’s a continuous glucose monitor, we can get little snapshots during the night.
[00:35:54] We don’t have to wake up and poke our finger, which is good. Which you could say even potentially alters the data. I’ve tried that. I don’t recommend it. What have you seen over the course of the night? Both acutely and then, Thoughts about what you’ve seen chronically with sleep impacting blood glucose?
[00:36:11] Yeah.
[00:36:12] Catherine Staffieri: So a couple things, right? A. Poor choices for dinner can result in some poor sleep later on as the body, again, like I said, is processing either just higher loads of carbohydrate later in the day when, you know, having a big dessert late at night maybe after a couple of drinks and a higher carbohydrate meal can just send it high, keep it high.
[00:36:35] You can crash down and you can wake up. Then you might be really hungry. I’ve seen a lot of people wake up and they’re like, I was starving, so I had to have something else to eat in the middle of the night. That then sends you up again and then down. It’s very dysregulated. You’re also waking up tired. And when you’re waking up tired, how often do you wanna go work out when you’re super exhausted from a po, right?
[00:36:54] So just mentally, you don’t want to make the healthier choices that your body frankly needs the next day. You are less sensitive to insulin the next day. So even a meal that you typically tolerate very well you are spiking higher from, recovering, slower from so we, we definitely see that in the data.
[00:37:12] And sometimes, that is one of those probing questions we ask. Again, one of those aha moments where someone says I’m, I ate the same breakfast that I had yesterday. Why is my score on this meal so much worse? And I say how did you sleep last night? They’re like, oh, it was terrible.
[00:37:24] I was like there you go. So there’s the physiologic response to poor sleep. There’s just the glucose response that can cause poor sleep. And it’s really interesting. We actually just did a little lunch and learn internally about cortisol. It was glucose spikes at night and how they are related to cortisol.
[00:37:42] And dreams or a dysregulation, it could be, heat, temperature changes, things like that. So we were exploring all of those areas cuz we’ve all seen it in our in our members’ data. Someone will say, I woke up in the middle of the night. Why did I was actually high.
[00:37:57] Some people say I woke up in the middle of the night and I crashed down low. So you can really see some different dysregulations and you probe a little bit more. Were you very hot? Were you cold? What did you have the night before to eat for dinner? And sometimes honestly it can be like a bad dream and a cortisol spike, which is a funky thing to see.
[00:38:13] So lo lots of different factors can impact sleep and it’s just more probing to figure out which ones, as you said, pulling the lever.
[00:38:22] Dr Mike T Nelson: Got it. Very cool. What are your thoughts about? So this is what I’ve told people for experiments to do. And this was before you could get access to each meal.
[00:38:33] So this is general. My recommendation now, and I’d be curious on your thoughts, is, in a perfect world, take three to four, ideally seven days. Let’s say you have a monitor for two weeks. So take week one, take three, four, maybe five days, seven days if you can. Just do whatever you were doing. Train normal, do your sleep, do whatever.
[00:38:51] And my bias of almost no one will do this now is don’t look at any of the data, try to be blind to all the data which drives them. Absolutely crazy. So I’m like, okay, let’s just do three days or four days. I want to get at least a weekend. I want to get some cardio days, I wanna get some strength training days.
[00:39:07] I wanna work day and off day. And then after that period of time, just record everything you eat, put your little timestamp on it, and then we’ll take a period of time, we’ll unveil all the data and then look at it, and then the following week, Look based on that data, what experiments do we wanna run?
[00:39:25] Do you wanna, let’s say you love Pop-Tarts, so maybe you have Pop-Tarts first thing in the morning or after training or whatever your favorite food is, or something that looked a little bit funky in your data. Play with that more in isolation and then see if there’s different things that, that can modify it.
[00:39:43] What are your thoughts about that approach?
[00:39:46] Catherine Staffieri: Yeah, absolutely. I would say I’ve only had a handful of members that have really taken a scientific approach about it. I had one guy who was like, adamant to figure out what kind of pasta he could tolerate. So he would, he, his exercise the same every morning.
[00:40:01] He would wait two hours without eating anything to be in a sort of, Fasted state, then he would eat different kinds of pasta every morning. And then he would sit there, he would basically do his own, like at-home glucose top test, he would take grams of pasta every day. Yep. I will say not many people do that yeah.
[00:40:18] It’s hard to do that. I agree. It’s the same. It’s the idea of let’s get a baseline reading, let’s see how you’re doing, and then what means, what’s, what means the most to you in terms of your health goals, if you are looking to optimize your performance. Okay, great.
[00:40:33] So we’re gonna test out various fuel sources, 15 minutes, an hour, whatever it is. And then let’s test out what we’re reading afterwards. Keep your exercise consistent. We’re going to change your fuel sources. And again, it’s just hard with people’s lives, right?
[00:40:47] They’re like, oh, I had a work dinner, or, yeah. Town last minute. So that’s why our programs the shortest you can work with us is one month, so it’s two sensors, cuz then at least we get a, a couple weeks worth of data depending on all the different lifestyle factors. But I agree, some people want to see, some people wanna test those foods and isolation.
[00:41:08] Like my guy with the pasta, he really just wants to see how his body handles pasta. But in my mind, that’s not really real life. You’re never just gonna sit down to a bowl of pasta at 10 in the morning. So it’s more interesting to see. Okay. Date night, and this is what you usually order on date night. So order that and do your regular day.
[00:41:26] Okay, this is where you are at baseline, now let’s do date night where you have some apple cider vinegar beforehand. Let’s do date night where you eat the chips and salsa at the end of your meal and you start with a salad or even some protein first. Like you can, let’s live in the real world and make those real world adjustments to optimize your glucose.
[00:41:47] And so that’s where it’s more applicable to these people, and that’s where they’re going to then carry that behavior forward. They’re not just going to eat, pasta at 10:00 AM
[00:41:56] Dr Mike T Nelson: Yeah, no, I agree with that. And I. For the record, I get all the crazy clients, which I love, which is great.
[00:42:01] But same thing, right? So even if we tested in isolation, then the next step is, okay, when would you normally have this? What does that meal normally look like? And let’s see if it’s still occurs then, right? Because most of ’em are like I wanna know which things specifically it is. It’s okay, we can test a complex meal, but we won’t know what particular thing is in there if it gets wacky.
[00:42:23] But you can pull them out and then test them. But again, you’re dealing with, internal versus external validity. And one of them will answer the question of why it’s not super practical. The other ones are more practical. But for some people that doesn’t give them the why, the detail that they really wanted, which you could argue may or may not matter, but, so I agree.
[00:42:43] It’s definitely a, an individual type thing. Yeah. Yeah. You mentioned Apple CI or vinegar and other, the fancy word people throw around is like a glucose disposal agent, which, these things have been around, and especially bodybuilding, folklore for, decades. I remember people taking, was it vanadium sulfate and all sorts of crazy stuff, which potentially in high doses can be very toxic.
[00:43:05] But any thoughts on that kind of classification of compounds? What have you seen? Just, I’m always curious because does it even work? And then if it does work, what is the kind of mechanism, Yeah.
[00:43:19] Catherine Staffieri: Apple cider vinegar, it can, it’s not a silver bullet for everyone.
[00:43:24] So again,
[00:43:25] Dr Mike T Nelson: This won’t fix everything if I just douse all my food in it, make it taste like crap.
[00:43:30] Catherine Staffieri: I’ve had people that have just taken it straight and they’re like, I can’t do that. I was like, you asked me to do that. Oh my God.
[00:43:36] Dr Mike T Nelson: Yeah. It’s pretty, it’s not fun tasting,
[00:43:39] Catherine Staffieri: right? No, absolutely. I think it’s, I think it’s.
[00:43:42] Again it’s n equals one for some people, right? It’s a huge difference in their meal. Others, it doesn’t, right? And again, there could just be other factors at play. It’s, again, it’s really hard to just say it’s no ozempic, right? I just gonna lower you, no matter what. So we see this with bitter melon.
[00:44:00] We see it with chromium, we see it with berberine. Some people respond really well to 500 milligrams of berberine before a meal. Some people don’t. Some people respond to chromium, some people don’t. You have to remember to take it or have it with you. If you’re traveling or going out to eat.
[00:44:15] It’s just another step that, do you have apple cider vinegar on you before you go out to dinner? Probably not. And you need to have it right before you eat. A lot of it’s more sort of lifestyle changes and testing things out and saying, okay, if you love to have.
[00:44:30] Popcorn after dinner or something like that. Okay, least you’re at home. Why don’t we try, why don’t we experiment with having, something before that and see how your body responds to it. But let’s also try something that you could do no matter what, like taking a walk afterwards. Does one respond better than the other?
[00:44:46] Do you just wanna keep Bering in your car all the time? But, there’s a lot of different ways to go about it. There’s different, I always get a little bit nervous about supplements because they are unregulated. I don’t know how much burberine they say is in there, is truly in there.
[00:45:01] You you can get into that murky world of supplements and some people just don’t even wanna take anything. Or they’re already taking so many, they don’t wanna take anything else. It’s, again it’s not a perfect system, but it can be
[00:45:13] Dr Mike T Nelson: helpful. Yeah, and I agree. And I was a supplement.
[00:45:17] Industry is regulated, but the issue of enforcement, and unfortunately, I would not take exactly what’s on the bottle and assuming that it’s in there from some very Unfortunately shady companies, there’s this study published the other day and I didn’t recognize a lot of the company brand, but some of them unfortunately had 1% of what was actually claimed to be on the bottle, like in there.
[00:45:41] So unfortunately, it is not as good as what we would like it to be. Yeah. And that’s,
[00:45:48] Catherine Staffieri: something against taking supplements. I’m, oh no. I think particularly when we had people that are following, certain lifestyle diets and they are missing out on nutrient, nutrients.
[00:45:59] And so you absolutely need that. You, the vegans need b12. Like you, you have to add things in at times and there’s nothing wrong with taking Zim zinc if you feel like you’re coming down with something. None of this is bad. What is interesting is when we see people with when they get those IV infusions, I don’t know if you’ve ever seen that in any of your people’s data, but super high doses of vitamin C can cause your.
[00:46:20] Skyrocket And so people Oh yeah.
[00:46:22] Dr Mike T Nelson: I don’t goof that sensor up like big time. Yeah. I don’t scare the shit outta people. They’re like,
[00:46:28] Catherine Staffieri: am I dying? You’re like no. It is your IV infusion.
[00:46:32] Dr Mike T Nelson: Yeah. Yeah. That would be freaky cuz you’re looking at it and you’re like, oh my God, what the hell?
[00:46:37] Catherine Staffieri: And it’s a very narrow spike.
[00:46:38] The body, you know that’s not thing that your body Yeah it clears very quickly. Yeah.
[00:46:43] Dr Mike T Nelson: Have you seen like sauna and cold water have any effects? So I did this a couple times and I have a converted freezer I made into a cold water immersion. And I was pricking my finger before, as I was getting in.
[00:46:57] And while I was in and while I was getting out, which wasn’t really horribly hard to do. It was a little bit tricky and again, n of one, but my glucose would typically in the morning. This was all just done fasted, no exercise beforehand. Think 85, 89, 87. And it would reliably drop into the fifties.
[00:47:18] Like I hit 55, 57. I didn’t feel hypoglycemic at all. I felt perfectly fine. I don’t know if you’ve seen weird stuff like that. I’m more the extreme ends.
[00:47:30] Catherine Staffieri: Yeah, absolutely. Not surprised to see something weird. And I’m assuming you probably recovered, I don’t know if you took a finger stick like an hour or two later.
[00:47:39] Generally, these are very short
[00:47:41] Dr Mike T Nelson: term. Oh yeah, it was very short. Yeah. Yeah. Like within, I don’t remember. I think the longest I checked it later was 45 minutes, maybe an hour. And it was back to normal. It didn’t stay for a long period of time. But yeah, I just thought that was interesting. It would drop that aggressively.
[00:47:56] Catherine Staffieri: Yeah. I’ve seen, I have a friend who wears one pretty religiously and he jumps in his freezing cold pool, Okay. To see what happens. And his shoot’s high. His really just skyrockets. Interesting. And that’s more of that stress effect as in yeah. Oh my God, the body’s like cortisol shock, releasing like large amounts of glucose.
[00:48:15] Cuz it’s like what’s happening to me? A lot of times I think it, it depends on, I think of a sauna. It’s almost that mental preparation. And I think sometimes when people do a cold. Plunge. I think it, it’s almost are you jumping into an ice cold pool or are you like sitting it’s almost like the stress going into it, it’s hyped up. Are you amped up? Are you like at a good, steady state and you just ease yourself into it? The body can, it can absolutely just like lower down. Or you hit it with that jolt and that spike, and you can see that, and with sauna as well, sometimes it can be very relaxing.
[00:48:48] I think for some people they find it very relaxing and so there’s no cortisol response and it’s, it can be, an increase due to the temperature and the interstitial fluid, the, the high sort of the dehydration kind of factor. Which, you can see and then the body comes back to normal.
[00:49:03] But I think it is interesting over time you can see a lowered. Glucose, lower average glucose. They’re starting to show that in the research. It’s not definitive, but I think some people will see it in the short term. And it can be very helpful kind of in the short term, but generally over time, hot and cold therapy can be very helpful.
[00:49:23] It can also just reduce inflammation overall in your body. And when you have less inflammation, you know your body can handle glucose better. It all works together.
[00:49:31] Dr Mike T Nelson: Yeah. And there’s some very preliminary research on the metabolic effects of both heat and cold. And I have a guess that I think in the future we’ll find that they are more beneficial on a metabolic health standpoint than what we probably realize now.
[00:49:47] That’s my guess, but there’s just not as much data on it. And I agree. It just depends also on adaptation. So I wasn’t able to grab a sample like as soon as I got in, cause my hands were still doing weird stuff. Maybe I should grab a. CGM and tested again. But I did it after I was in for three to four minutes at about 48 degrees.
[00:50:05] And this is after I had been doing it for probably around six months. So I was probably more adapted, more, more relaxed. But I could definitely see that when you get in initially there’s probably a huge spike too. Cause you’ve probably seen this data on people who exercise too. Like people are shocked that they’re like, oh my god, my blood glucose went up, I’m exercising.
[00:50:25] I’m like yeah, because you need some fuel in order to exercise, so your liver’s gonna dump out a bunch of blood glucose and your bloodstream like, it’s okay. Like you don’t need to freak out about it.
[00:50:37] Catherine Staffieri: A hundred percent. That’s also one of those aha moments. People are like, wait, what? Why did my glucose go up when I was exercising?
[00:50:42] And we always say, what were you doing? And it’s generally that anaerobic, hit type workouts where the body just doesn’t have enough to fuel the exercise and so it pulls it outta storage and people are like, oh my God, is that okay? It’s yeah, absolutely. It’s okay. You can play around with fueling.
[00:50:56] I think a lot of women tend to exercise fasted. And we can, we encourage them to test something else out, try and eat a little bit before you work out. Let’s see, how your energy levels can you work out harder, faster, stronger if you give yourself a little bit of fuel as opposed to, hoping your body gives you enough in time.
[00:51:13] Yeah. And
[00:51:14] Dr Mike T Nelson: fascinating side note, the liver is actually under what’s called a feed forward mechanism. So it’ll actually dump out more than what it probably initially needs where a lot of stuff is on a feedback mechanism where it’s looking at different levels. Last question as we wrap up, what do you think is coming in the future?
[00:51:31] What would you, if you could design a sensor, would you wanna see insulin levels? Would you wanna see cortisol? Would you wanna see, we’ve got a marker for glucose. I know some people I know have been testing the lactate and the ketone continuous monitors. Any thoughts on that and what you think might be sooner than later?
[00:51:54] Catherine Staffieri: Absolutely. In continuous insulin monitor would be, would be awesome for the mass. Yeah. And you could overlay ketones on it and just a continuous creactive protein monitor to level your Sure. Levels of inflammation would be incredible. I just, I really hope access to all of this is improves, be it, the incredible things that just the Apple Watch has done.
[00:52:15] Wearables, Garmin, just even having access to steps has really been helpful and motivating to a lot of people. I just think the more people that can get access to the data will have a better idea of what’s actually going on in their body now as opposed to going to their doctor one time a year and getting the news like, oh my gosh, you’re pre-diabetic.
[00:52:34] Like, why, when did that happen? Yeah. And the more that people can get an idea of what’s happening in January, what’s happening in April, what’s happening in July, The better they will, the better motivated and the better in charge of their own health they will be. So I hope we can get more data, but I also, we can, I hope we can just get more people getting data to really help prevent the chronic diseases.
[00:52:55] Dr Mike T Nelson: Yeah. Very last question. I just thought of one more quick one I wanted to get in is, have you seen any weird stuff with the use of like ketone salts or esters in terms of ketones as a supplement and the effect on blood glucose? What I’ve seen is that they do generally tend to lower blood glucose at least is what I’ve seen on just anecdotal on a few individuals.
[00:53:18] Yeah, I think it
[00:53:19] Catherine Staffieri: depends on when they’re taking them. Yes, I’ve seen different things in the morning versus the the afternoon. Some people will take them at night, which I don’t I don’t really recommend if we’re seeing higher levels overnight, we’ll play around with meal composition and meal timing before we would do anything like that.
[00:53:35] And again, it depends on what they’re. If they’re taking them before a workout or versus some people take them if they’re about to do a podcast or, or have a stressful event or something, like a presentation or something related to their work. So a little bit different in terms of like brain energy and and the stress that overlays the glucose output in response to the ketones coming in.
[00:53:57] So yes, I’ve seen the decline. I’ve also seen a steady state and then they say I don’t know if there was a real impact on it, but I say maybe it mitigated a spike that we just didn’t see.
[00:54:07] Dr Mike T Nelson: Yeah. Yeah. And that’s what’s always hard cuz you’re always looking at just the n of one and a snapshot in time too, at that point.
[00:54:14] Catherine Staffieri: Yeah. But I, to, to that point, I just encourage someone to say, encourage someone to do let’s do a five day test if you can try and keep it scientific and take it at the same time every day. Let’s see how your body’s responding to it on a more continuous basis.
[00:54:28] Dr Mike T Nelson: Cool.
[00:54:29] Awesome. Thank you so much. Where can people find out more about Nutri Sense and tell us more about everything you got going on?
[00:54:35] Catherine Staffieri: Absolutely. I have been joking around lately. If you just say it three times, your phone will start sending you ads.
[00:54:41] Dr Mike T Nelson: Oh, nice.
[00:54:43] Catherine Staffieri: I’ll have to test that out.
[00:54:44] They’re all listening. You can find us on the web@ww.nutrisystem.io and I encourage everyone to just check it out. We have an amazing blog. It’s called The Journal and all evidence-based, really fascinating bite-sized articles that can show you how this kind of technology can really improve all aspects of your health.
[00:55:04] So if you’re on the fence, if you’re not totally sure if this is the right tool for you, you can really see how applicable it is. And Nutri Sense is pretty amazing because with your first month you get dietician support, nutritionist support, so you get someone. Along the way, guiding you, showing you trends, showing you what’s going on, helping you navigate, giving you ideas.
[00:55:25] So we think we’re pretty special in that way. You’re not out there on your own and you’re not out there blind. You’ve got someone helping you out. So definitely check out our website. We’re on all the social media avenues. Instagram at Nutri Sense io. And you can watch people putting on their monitors.
[00:55:40] You can watch people with all their different tests and stuff like that. It’s super great. I encourage everyone to check it out.
[00:55:46] Dr Mike T Nelson: Yeah. And I will say that I’ve had clients user service before and I’ve done it just without the early on, just the old school, just stick monitors on ’em and you’re managing it all.
[00:55:56] It is so much nicer to have someone else on the backend that I can refer them to and get their input because sometimes clients can drive you a little bit crazy with some of the questions. So it was nice to have an external expert being like, okay, let’s look at this. And then obviously you guys look at data all the time and can, come up with a game plan and then I would, go over it with them, once a week or something.
[00:56:19] So it was super, super nice to have someone managing the day-to-day, changes and looking at the data and making suggestions and then looking at it as an overview. So for trainers who are working with clients, like having someone else that helps with that whole process and that’s all they do is extremely helpful also too.
[00:56:36] Totally. Absolutely. Yeah. Awesome. Thank you so much for all your time today. I really appreciate it. This was super fun.
[00:56:43] Catherine Staffieri: Thank you so much. It was my pleasure.
[00:56:45] [00:56:46] Dr Mike T Nelson: Thank you so much for listening to the podcast. Huge thanks to Catherine for coming on here and sharing all the trends and everything she’s seen from literally hundreds of thousands of hours of data. Which is great. You get a snapshot of kind of a starting point of what to look for, which is awesome.
[00:57:03] I will put a link to their program and everything there. I don’t have any disclosures with it. I didn’t get paid anything to do this podcast. I don’t make anything selling continuous glucose monitors or anything like that. But I think if they’re done correctly, I do think they can be a good tool to use on occasion.
[00:57:21] I don’t think you probably need to have one on for the rest of your life. But I do think it is a useful experiment to get an idea based on your physiology of what’s going on. So thank you so much for listening to the podcast. Really appreciate it. If you want more podcasts, you can just go to my website, which is MikeTNelson.
[00:57:39] com forward slash podcast, and they’ll have all the listings of all the podcasts we’ve done, including other guest episodes. That I’ve done that don’t show up on your podcast feed here. So go to MikeTNelson. com podcast and at the bottom there will be a way to get on to the newsletter. So that’s the best place to get all content from me.
[00:58:01] I usually send out a newsletter once a day, trying to make them informative and entertaining at the same time. You can go to MikeTNelson. com forward slash podcast, get on the newsletter, see all the old podcasts also. Thank you so much. Really appreciate it. And we will talk to all of you very soon.
[00:58:18] [00:58:19] Personally, I don’t care for puppets much. I don’t find them believable. I don’t believe you!
[00:58:26] Nancy: This podcast is for informational purposes only. The podcast is not intended as a substitute for professional medical advice, diagnosis, or treatment. You should not use the information on the podcast for diagnosing or treating a health problem or disease or prescribing any medication or other treatment.
[00:58:42] Always seek the advice of your physician or other qualified health provider before taking any medication or nutritional, supplement, and with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have heard on this or any other podcast.
[00:58:58] Reliance on the podcast is solely at your own risk. Information provided on the podcast does not create a doctor-patient relationship between you and any of the health professionals affiliated with our podcast. Information and statements regarding dietary supplements are not intended to diagnose, treat, cure, or prevent any disease.
[00:59:15] Opinions of guests are their own, and this podcast does not endorse or accept responsibility for statements made by guests. This podcast does not make any representations or warranties about guest qualifications or credibility. Individuals on this podcast may have a direct or indirect financial interest in products or services referred to therein.
[00:59:33] If you think you have a medical problem, consult a licensed physician.







Leave A Comment