I recently returned from the epic ISSN meeting, and it was back to “normal” (if anything I do is really “normal”) Monday. I was tired and after a bit more coffee than usual, I made it to the commercial gym where I do more upper body “bro work” on Mondays.
I was dragging in the session, but prolonged the rest periods between sets, cranked up some new Sepultura (Eloy’s drumming is so amazing and Derrick crushed the vocals) and dropped my plan on the first exercise of incline DB presses from set at 5 -7 reps with the 90s to the 80s for sets of 7.
Ditto for 1 arm rows and only worked up to a top set of 120 x 8, using straps once I was past the 100s.
I did less work on the accessory exercises, used the sauna to down-regulated, and walked home.
My sleep was terrible and my body was still thinking it was time to stay up to 1 am again like I did most of the previous week.
Fast forward to Tuesday’s session in the Extreme Human Performance Center (aka my garage gym) where front squats felt fine, but dropped my goal again by a few reps and split them out over a few more top-end sets.

Saxon pinch bar deadlifts were slow to warm up and in the end, I came within 5 lbs of my PR weight, so I was happy with those went.
Both Monday and Tuesday my low back felt a bit tight and had more sensation than usual.
After front squats on Tuesday, I was feeling it a bit more again and figured it was just from not much movement later last week.
You can probably see where this is going. I moved on to some higher pull deadlifts (14-inch pick) and I was starting to feel much more fatigued.
Baaaaaw- it’s probably just the heat.
Then on my 4th rep at only 275 lbs, I felt a kink in my back and the weight instantly went down to floor.
My first thought was —ah sheeeeeeeeeet. Now I did it.
For better or worse, I’ve had all sorts of injuries over my almost 48 years on the planet.
Everything from a completely ripped out right shoulder –broomball accident, dislocated left shoulder – me vs tree on my mountain bike, pulled/severely strained both adductors/groin – being an idiot doing high incline sprints on the treadmill, pulled hamstring –hard impact off a small cliff drop snowboarding, strained both wrists – learning to windsurf, bruised/cracked ribs a few times – kiteboarding and snowboarding, completely spiraled right ankle- snowboarding, partial tore left knee LCL- go-kart incident, low back snafu – strongman comp.

You get the picture.
I have many reps with injury, so I knew not to catastrophize the incident.
I stood up and moved around okay. Most movements tested ok, with no nerve pain, only back extension was weird.
I was 90% sure it was just a muscle strain in my lower erector spinae and/or my QL in my lower back.
I immediately shut down the session and went for a walk to just get some pain-free movement and relax. My gait was off a bit although I could walk without pain – a great sign.
Looking back, there are 2 big lessons here that you can apply to avoid my stupidity.
Lesson 1: Listen To Your Body – For Real
I know, I know, you hear this all the time
“Yo Bro- you need to listen to your body.”
Listening is step 1 and actually doing something is where most fail.
On the deadlifts, rep 3 felt hard. Baw, it can’t be.
I cranked out 1 more rep.
I could feel my left back was a bit more ouchy.
Nah- I can do 1 more rep easily. This is about 100 lbs less than what I have typically done.
That was a bad idea.
It does not matter at that point in time if my max was 700 lbs, my body was saying “Hey, dumbass, I am not having this. Time to shut it down.”
I didn’t listen.
My body then yelled and shut me down for the day.
Some days you can still skate by.
Other days you can’t.
Listen, then act appropriately.
Lesson 2: Load Spike
Many lifters get injured in the gym when their total volumes goes up dramatically and there is research to support this idea (1-7).
Yes, there is a bunch of debate about where the line is and what qualifies as “dramatically,” the takeaway here is going from zero to more than I did in the previous week was a no-bueno idea.
While I did a similar session the previous Tuesday, I did nothing for lifting until that Monday.
I am not 100% sure this contributed, since if I just listened to my body I would have been fine; but watching for load spikes is something to pay attention to in your programming.
With my online M3 1-1 clients, I spend a bunch of time giving them programs to do while they are on vacation, even if it is just a day or two of bodyweight training. Something is better than nothing.
Then once they’re back I will drop the volume down for a re-entry week to avoid them going from very very low volume to even moderate volume since the rate of change is high (aka load spike).
What to do if you’re injured
Step 1: if you really foobard yourself, go see a doc.
Get it checked out!
Do not pass GO and collect $200.
Shout out to my buddy Steven Horney, DPT at Integrated Health Sciences in NY for the chat today. If you are in this area and need help, hit him up!
Strap on your crash helmet and lube up the slide as we are going head-first down the nerd chute hard. You have been warned!
Step 2: Biomech Interventions
Katie Dabrowski, DPT, and I cover this topic on the Flex Diet Podcast. We go in-depth on it, but for me, the next step is to determine the endpoint.
Just like with training clients for their goals, what is your goal? It may be to lose 20 lbs, deadlift 405, bench press 315, etc. It doesn’t matter, as your goals are your goal.
Healing from an injury is the same.
What is the goal?
To me, a good goal is to do the thing you did when the injury happened successfully. My bias is to do it without any compensation and in time, with no fear of re-injury doing it.
This one is simple. Deadlift 275 x 5, double overhand from a higher pick point of 14 inches (the bar is starting higher off the ground).
This will happen in time.
I have zero hesitation that I will do it.
How long- that is always the unknown, and I am in no hurry to be an idiot again and rush the process.
If you are a professional getting paid top money for performance, then you can take a few more risks. For most, it is not worth it.
My goal is to accumulate as many pain-free reps that are as close to the above position as I can.
For example, yesterday I was able to get to the start position without any load with only a slight amount of pain (1 out of 10) to start the movement.
Again, this is completely unloaded- no bar or weight in my hand, just supporting my upper body weight in the start position.
Over time I will add reps of just bodyweight and then top and bottom position work.
Yesterday I did those on a 45-degree back extension – the top was a supported version using my hands to support my body, and the bottom position was fine so I went up about 1 inch. I did 30-sec isometrics in those positions also without any pain.
My progression is to do a full range of motion 45-degree back extension, add reps, then slowly add load.
Outside of the deadlift, this will be my main testing exercise.
And it goes without saying that I am still training per usual. I had to modify my goals a bit for now, but there are a ton of exercises I can do without pain to still make progress toward my goals. I did a review of a couple in my IG stories.
Step 3: Biochemical Interventions
The normal advice about nutrition matters- eat more protein, some carbs to fuel training, some fat, mostly whole foods, and lots of micronutrients. All the stuff I cover in detail in the Flex Diet Cert.
I have opted to push up my calories a bit more.
Yes, that means I will probably gain a bit of fat. Oh my!
Remember that tissue healing takes energy and your body is very reluctant to pull that energy from fat stores.
How many more calories is hard to pin down since trauma and burns are the common models use (1-7).
I don’t think it’s anywhere close to those massive amounts; however, my goal is tissue healing in the shortest time possible so I will hedge my bets towards a surplus.
I’ve seen this happen with several clients in the past where they get injured, have to drop their training volume, and thus slash and burn their calories super low. It seemed to take forever for them to heal.
My bias is to keep calories a bit higher, even if that results in some fat gain, then once you are back to 100% good to go, you can easily lose what you gained in a few weeks.
Beyond that, I am using more collagen at 15 grams with 50 mg Vit C at 40 -60 min before isometric exercise to help strengthen the soft tissue.
I have no idea if I tweaked up the muscle, soft tissue or both, so I am going to hedge my bets and work on both via collagen for soft tissue and complete proteins for muscle recovery.
For a deep dive on collagen and exercise, listen to the 2 podcasts I did below.
I did add some turmeric to potentially help with healing and the usual creatine monohydrate, fish oil, multi-vite, and magnesium.
Miscellaneous
In the land of a bit woo-woo, here is what I am doing.
My caveat here is that much of the data I have is done in mice, rats, some cell cultures, different human populations and for different indications.
I am fully aware of the limitations of the research here, but in light of perfectly controlled randomized controlled trials, this is what I am opting to do.
The pubmed ninjas can stuff a sock in it as I still have 30 references, which is 30 more than Biceps Billy has on any one post.
AM Red Light
I’ve been using a red light in the AM for coming up on 3 years now and it seems to help. It has been used for a wide variety of conditions in research (8-17).
Right now I am at 10 minutes total and changed it to only 3 minutes in front and 7 minutes on my back to bias it more towards that area. I have the classic 2 panel from Red Rush. I have no disclosures with them and don’t make a dime from them.

Micro-Current: Dolphin
I use the Dolphin micro-current device with its scar protocol around the injury. This is a bit tricky to do on myself, but I am making do since Jodie is out of town.
I’ve used this technology for over 6 years now on myself- my midline scar from open-heart surgery in 1978 looks much much better now, and many clients over the years. The research on it is generally positive (18-27)
Nothing to disclose. I had an NDA in the past to better understand the tech, but it was unpaid because I am an idiot with business consulting when I want to understand something in detail as I will take it in the financial shorts to figure it out.

Passive Micro-Current
The other device I am using is the Healy device. This is much easier to use as you can attach sticky pads above and below the area and then set it up via your smartphone on the pain setting.
I will be honest, I don’t understand how the thing works other than it is some form of micro-current. It sounds woo-woo AF; however I’ve used it on other settings and in the past – it seems to work really well.
Maybe it’s all placebo, but better is better, and other than the initial cost, it is easy to apply while I am working. I also use it on clients during in-person sessions.
Note-I am an affiliate for them so I do make a bit of coin (honestly I forgot how much), and click HERE if you want more info or just email me.

Hot/Cold
If I had more access to a sauna, I would be using it.
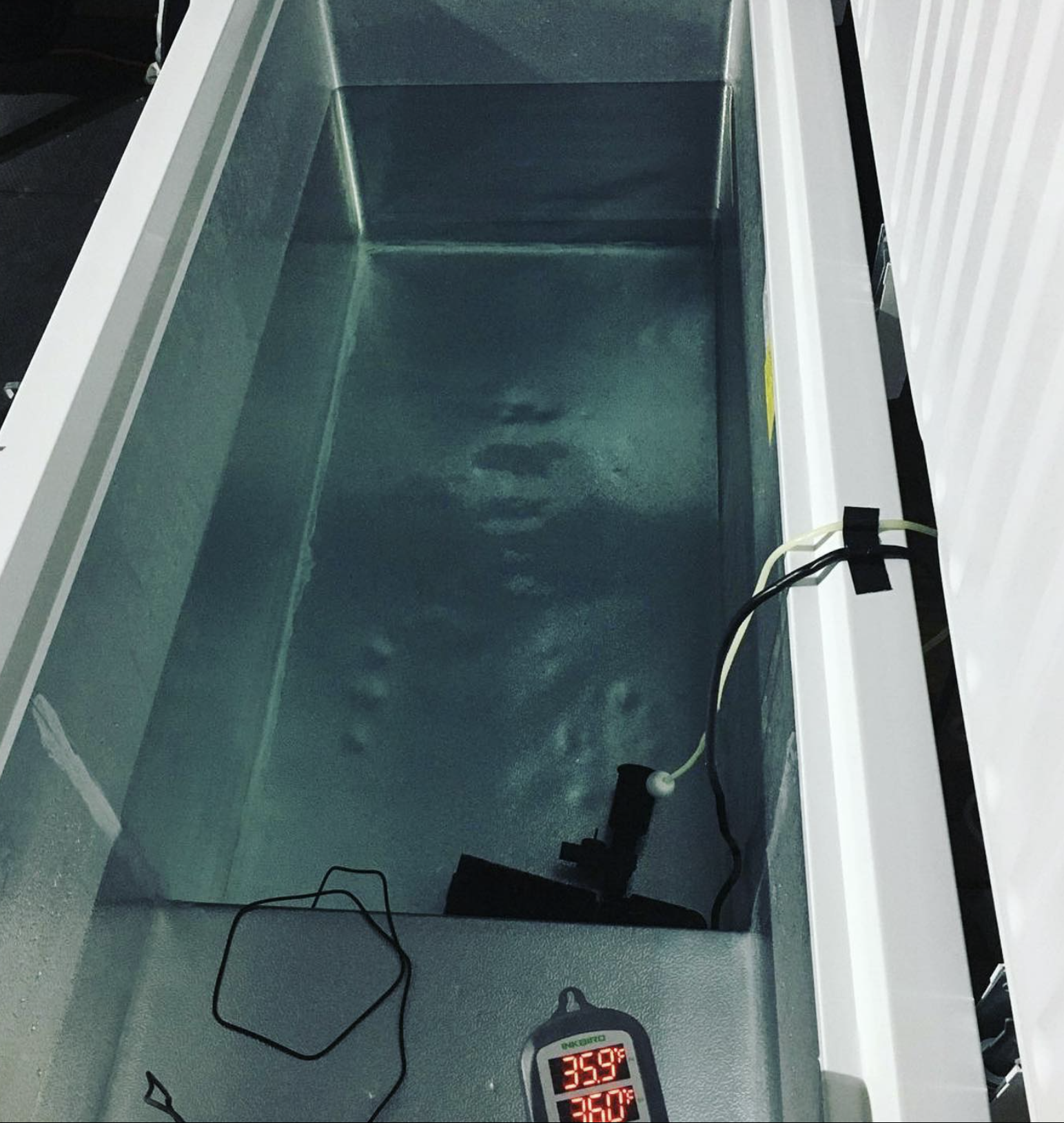
Ditto for cold, and while I have a converted cold water immersion in my garage, getting in and out of it right now is a bit tricky. Once I am able to do that I will be in there again.
I discuss all the pros and cons of hot/cold in the Phys Flex Cert.
Future: WAEF
Aka When All Else Fails.
I still have more options if this all craps the bed and does not work out. A few of those would be:
Chiro/Neurology
My go-to is Dr Schmoe here at the Functional Neurology Center. I’ve been there many times and did a 1-week intensive in the past for my eye / vestibular function. He and his team are top-notch.
Pulse Centers PEMF
PEMF is pulse electromagnetic frequency stimulation. I know Dr Schmoe just got one at his center. I’ve used them a few times in the past and it really seemed to make a big difference.
Nothing to disclose, but if you are interested in them, ask to speak to Emilio and tell him I sent you. I make nothing off it.
Peptides
There is some data that some peptides can help speed up healing. I have coordinated this with a few M3 1-1 clients via Dr Ryan Greene. To date, I have not done any HRT or peptides (other than Kambo, which I guess is peptides maybe?) Again, that is just my personal choice at this point; but it is not something I am going to rule out.
For more info, check out the podcast I did with Dr Greene and Dr Andy Galpin:
Note- listen to the podcast first before contacting Dr Greene so you have a background on what is going on as it is not just about “hey give me peptides” approach.
Nothing to disclose as I don’t make a dime if you see him; however, I trust him 100%.
Wow, congrats if you made it this far!
This is the bleeding edge of what I am doing to get back on track in record time.
Hopefully, you can pull a few ideas from here to talk with your PT, trainer, coach, doc, etc.
Or save this for future use if you ever need it.
PS- let me know what you thought of this one. If you know someone who has niggly issues, kick this over to them. Thank you!
References (AKA, stuff it Pubmed Ninjas)
Blanch P, Gabbett TJ. Has the athlete trained enough to return to play safely? The acute:chronic workload ratio permits clinicians to quantify a player’s risk of subsequent injury. Br J Sports Med. 2016 Apr;50(8):471-5. doi: 10.1136/bjsports-2015-095445. Epub 2015 Dec 23. Erratum in: Br J Sports Med. 2019 Sep;53(18):e6. PMID: 26701923.
Gabbett T. J. (2020). The Training-Performance Puzzle: How Can the Past Inform Future Training Directions?. Journal of athletic training, 55(9), 874–884. https://doi.org/10.4085/1062/6050.422.19
Gabbett TJ. Incidence, site, and nature of injuries in amateur rugby league over three consecutive seasons. Br J Sports Med. 2000 Apr;34(2):98-103. doi: 10.1136/bjsm.34.2.98. PMID: 10786864; PMCID: PMC1724194.
Gabbett TJ. How Much? How Fast? How Soon? Three Simple Concepts for Progressing Training Loads to Minimize Injury Risk and Enhance Performance. J Orthop Sports Phys Ther. 2020 Oct;50(10):570-573. doi: 10.2519/jospt.2020.9256. Epub 2019 Nov 15. PMID: 31726926.
Seshadri DR, Thom ML, Harlow ER, Gabbett TJ, Geletka BJ, Hsu JJ, Drummond CK, Phelan DM, Voos JE. Wearable Technology and Analytics as a Complementary Toolkit to Optimize Workload and to Reduce Injury Burden. Front Sports Act Living. 2021 Jan 21;2:630576. doi: 10.3389/fspor.2020.630576. PMID: 33554111; PMCID: PMC7859639.
Soligard T, Schwellnus M, Alonso JM, Bahr R, Clarsen B, Dijkstra HP, Gabbett T, Gleeson M, Hägglund M, Hutchinson MR, Janse van Rensburg C, Khan KM, Meeusen R, Orchard JW, Pluim BM, Raftery M, Budgett R, Engebretsen L. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br J Sports Med. 2016 Sep;50(17):1030-41. doi: 10.1136/bjsports-2016-096581. PMID: 27535989.
Vanrenterghem J, Nedergaard NJ, Robinson MA, Drust B. Training Load Monitoring in Team Sports: A Novel Framework Separating Physiological and Biomechanical Load-Adaptation Pathways. Sports Med. 2017 Nov;47(11):2135-2142. doi: 10.1007/s40279-017-0714-2. PMID: 28283992.
Parent B, Seaton M, O’Keefe GE. Biochemical Markers of Nutrition Support in Critically Ill Trauma Victims. JPEN J Parenter Enteral Nutr. 2018;42(2):335-42.
Clark RG. Caloric requirements after operation. The Proceedings of the Nutrition Society. 1971;30(2):158-65.
Sears B, Perry M, Saha AK. Dietary Technologies to Optimize Healing from Injury-Induced Inflammation. Antiinflamm Antiallergy Agents Med Chem. 2021;20(2):123-31.
Stoner HB. Energy metabolism after injury. J Clin Pathol Suppl (R Coll Pathol). 1970;4:47-55.
Davari M, Moludi J, Asghari Jafarabadi M, Ahmadi-Nejad M, Sanaie S, Aref-Hosseini SR. Impact of clinical factors on calorie and protein intakes during Icu stay in adults trauma patients: results from a prospective observational study. Int J Burns Trauma. 2019;9(3):59-65.
Wischmeyer PE. Tailoring nutrition therapy to illness and recovery. Crit Care. 2017;21(Suppl 3):316.
Moreira E, Burghi G, Manzanares W. Update on metabolism and nutrition therapy in critically ill burn patients. Med Intensiva (Engl Ed). 2018;42(5):306-16.
Salehpour F, Mahmoudi J, Kamari F, Sadigh-Eteghad S, Rasta SH, Hamblin MR. Brain Photobiomodulation Therapy: a Narrative Review. Mol Neurobiol. 2018;55(8):6601-36.
Ram Y, Hadany L. Condition-dependent sex: who does it, when and why? Philos Trans R Soc Lond B Biol Sci. 2016;371(1706).
Assis L, Manis C, Fernandes KR, Cabral D, Magri A, Veronez S, et al. Investigation of the Comparative Effects of Red and Infrared Laser Therapy on Skeletal Muscle Repair in Diabetic Rats. Am J Phys Med Rehabil. 2016;95(7):525-34.
de Melo CA, Alves AN, Terena SM, Fernandes KP, Nunes FD, da Silva Dde F, et al. Light-emitting diode therapy increases collagen deposition during the repair process of skeletal muscle. Lasers Med Sci. 2016;31(3):531-8.
Avci P, Gupta A, Sadasivam M, Vecchio D, Pam Z, Pam N, et al. Low-level laser (light) therapy (LLLT) in skin: stimulating, healing, restoring. Semin Cutan Med Surg. 2013;32(1):41-52.
Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516-33.
Souza NHC, Mesquita-Ferrari RA, Rodrigues M, da Silva DFT, Ribeiro BG, Alves AN, et al. Photobiomodulation and different macrophages phenotypes during muscle tissue repair. J Cell Mol Med. 2018;22(10):4922-34.
Mosca RC, Ong AA, Albasha O, Bass K, Arany P. Photobiomodulation Therapy for Wound Care: A Potent, Noninvasive, Photoceutical Approach. Adv Skin Wound Care. 2019;32(4):157-67.
Glass GE. Photobiomodulation: The Clinical Applications of Low-Level Light Therapy. Aesthet Surg J. 2021;41(6):723-38.
Ribeiro BG, Alves AN, Dos Santos LA, Cantero TM, Fernandes KP, Dias Dda S, et al. Red and Infrared Low-Level Laser Therapy Prior to Injury with or without Administration after Injury Modulate Oxidative Stress during the Muscle Repair Process. PloS one. 2016;11(4):e0153618.
Naclerio F, Seijo M, Karsten B, Brooker G, Carbone L, Thirkell J, et al. Effectiveness of combining microcurrent with resistance training in trained males. European journal of applied physiology. 2019;119(11-12):2641-53.
Piras A, Zini L, Trofè A, Campa F, Raffi M. Effects of Acute Microcurrent Electrical Stimulation on Muscle Function and Subsequent Recovery Strategy. International journal of environmental research and public health. 2021;18(9).
Naclerio F, Moreno-Perez D, Seijo M, Karsten B, Larrosa M, García-Merino JÁ L, et al. Effects of adding post-workout microcurrent in males cross country athletes. European journal of sport science. 2021;21(12):1708-17.
Kwon DR, Park GY. Efficacy of microcurrent therapy in infants with congenital muscular torticollis involving the entire sternocleidomastoid muscle: a randomized placebo-controlled trial. Clin Rehabil. 2014;28(10):983-91.
Ohno Y, Fujiya H, Goto A, Nakamura A, Nishiura Y, Sugiura T, et al. Microcurrent electrical nerve stimulation facilitates regrowth of mouse soleus muscle. Int J Med Sci. 2013;10(10):1286-94.
Fujiya H, Ogura Y, Ohno Y, Goto A, Nakamura A, Ohashi K, et al. Microcurrent electrical neuromuscular stimulation facilitates regeneration of injured skeletal muscle in mice. J Sports Sci Med. 2015;14(2):297-303.
Ranker A, Husemeyer O, Cabeza-Boeddinghaus N, Mayer-Wagner S, Crispin A, Weigl MB. Microcurrent therapy in the treatment of knee osteoarthritis: could it be more than a placebo effect? A randomized controlled trial. Eur J Phys Rehabil Med. 2020;56(4):459-68.
Zickri MB. Possible local stem cells activation by microcurrent application in experimentally injured soleus muscle. Int J Stem Cells. 2014;7(2):79-86.
Stößlein BAC, Kuypers KPC. Self-Rated Recovery and Mood Before and After Resistance Training and Muscle Microcurrent Application. Front Psychol. 2022;13:836695.
Moon YS, Kwon DR, Lee YJ. Therapeutic effect of microcurrent on calf muscle atrophy in immobilized rabbit. Muscle Nerve. 2018;58(2):270-6.
Rock on!

Dr. Mike T Nelson
Dr. Mike T Nelson
PhD, MSME, CISSN, CSCS Carrick Institute Adjunct Professor Dr. Mike T. Nelson has spent 18 years of his life learning how the human body works, specifically focusing on how to properly condition it to burn fat and become stronger, more flexible, and healthier. He’s has a PhD in Exercise Physiology, a BA in Natural Science, and an MS in Biomechanics. He’s an adjunct professor and a member of the American College of Sports Medicine. He’s been called in to share his techniques with top government agencies. The techniques he’s developed and the results Mike gets for his clients have been featured in international magazines, in scientific publications, and on websites across the globe.
- PhD in Exercise Physiology
- BA in Natural Science
- MS in Biomechanics
- Adjunct Professor in Human
- Performance for Carrick Institute for Functional Neurology
- Adjunct Professor and Member of American College of Sports Medicine
- Instructor at Broadview University
- Professional Nutritional
- Member of the American Society for Nutrition
- Professional Sports Nutrition
- Member of the International Society for Sports Nutrition
- Professional NSCA Member







Leave A Comment